Peripheral Arterial Disease (PAD) affects millions worldwide, yet its impact often goes unrecognized. This silent condition, characterized by narrowed arteries in the limbs, can lead to serious complications if left untreated.
In this blog post, we'll delve into the intricacies of PAD, exploring its causes, symptoms, diagnostic methods, and treatment options. By increasing awareness and understanding of PAD, we aim to empower individuals to recognize the signs, seek timely medical intervention, and make informed lifestyle choices to manage this condition effectively.
What is Peripheral Arterial Disease (PAD)?
Peripheral Arterial Disease (PAD) is a circulatory condition characterized by narrowed arteries that reduce blood flow to the limbs, typically the legs. This narrowing, often caused by atherosclerosis, inflammation, injury, or radiation exposure, results in decreased oxygen and nutrient supply to the affected tissues. PAD is associated with various risk factors including diabetes, smoking, obesity, high blood pressure, and high cholesterol levels.
Symptoms of PAD
PAD manifests through a range of symptoms, reflecting the compromised blood flow to the lower extremities:
- Intermittent Claudication: One of the hallmark symptoms of PAD is intermittent claudication, which refers to leg pain or discomfort that occurs during physical activity, particularly walking. This pain typically subsides with rest but recurs upon resuming activity. It stems from inadequate blood supply to the leg muscles, leading to oxygen deprivation during exertion.
- Numbness, Tingling, or Weakness: Patients with PAD may experience sensations of numbness, tingling, or weakness in their legs. These sensations often indicate nerve damage due to reduced blood flow, leading to impaired sensory and motor functions.
- Skin Changes: PAD can cause noticeable changes in the skin of the legs and feet. These changes may include discoloration, where the skin appears pale or bluish due to reduced blood flow. Additionally, patients may experience hair loss on the legs and feet, as well as alterations in skin temperature, which can feel cooler than the surrounding areas.
- Non-healing Wounds or Ulcers: Chronic insufficient blood flow in PAD can result in the development of non-healing wounds or ulcers, particularly on the lower extremities. These wounds may appear as open sores or ulcers on the feet or toes and are often slow to heal due to compromised tissue repair mechanisms.
Diagnosing PAD
Diagnosing Peripheral Arterial Disease (PAD) involves a comprehensive evaluation combining various clinical assessments and specialized tests to confirm the presence and severity of the condition.
Physical Exam and Medical History
The initial step in diagnosing PAD typically involves a thorough physical examination and a detailed medical history review. During the physical exam, a healthcare provider may assess the patient's pulses in the affected limbs, looking for weak or absent pulses, which can indicate reduced blood flow. They may also examine the patient's legs for signs of skin changes, such as discoloration or ulcers, and evaluate any symptoms reported by the patient, such as leg pain or numbness.
A comprehensive medical history review helps identify potential risk factors for PAD, such as diabetes, smoking, hypertension, and hyperlipidemia. Understanding the patient's medical history provides valuable insights into their overall health status and aids in determining the likelihood of PAD.
Ankle-Brachial Index (ABI) Test
The Ankle-Brachial Index (ABI) test is a non-invasive diagnostic tool used to assess blood flow and detect arterial obstruction in the lower extremities. During the ABI test, blood pressure measurements are taken at the ankles and compared to blood pressure measurements taken at the arms (brachial arteries).
A ratio of the ankle systolic blood pressure to the brachial systolic blood pressure is calculated, with lower ratios indicating poorer arterial circulation. An ABI value of less than 0.90 is generally considered abnormal and indicative of PAD. This simple and cost-effective test is often performed in a clinical setting and provides valuable information about the severity of arterial obstruction in the lower limbs.
Imaging Tests
Imaging tests play a crucial role in diagnosing PAD by providing detailed anatomical information about the arterial system and identifying areas of stenosis or occlusion. Two common imaging modalities used in the diagnosis of PAD include ultrasound and angiography.
Ultrasound
Ultrasound imaging, also known as duplex ultrasonography, utilizes high-frequency sound waves to visualize blood flow within the arteries and assess the presence of arterial narrowing or blockages. This non-invasive technique provides real-time images of the blood vessels, allowing healthcare providers to evaluate blood flow velocity, detect plaque buildup, and identify any abnormalities in the arterial walls.
Ultrasound is particularly useful for assessing the severity and location of arterial lesions and guiding treatment decisions, such as determining the suitability for endovascular interventions like angioplasty or stenting.
Angiography
Angiography is a more invasive imaging procedure that involves the injection of a contrast dye into the arterial system followed by X-ray imaging to visualize the blood vessels. This technique provides detailed images of the arterial anatomy, including the location and extent of arterial blockages.
Peripheral angiography can be performed using conventional X-ray angiography or newer techniques such as magnetic resonance angiography (MRA) and computed tomography angiography (CTA). These advanced imaging modalities offer high-resolution images of the arterial vasculature and help guide treatment planning for patients with PAD.
Stages of PAD
Peripheral Arterial Disease (PAD) is often classified into stages based on the severity of symptoms and the degree of arterial obstruction. Two commonly used staging systems for PAD are the Fontaine and Rutherford classifications.
Fontaine Stages
The Fontaine classification system categorizes PAD into four stages based on the presence and severity of symptoms:
- Stage I (Asymptomatic): Patients with Stage I PAD are asymptomatic and do not experience any symptoms of arterial insufficiency.
- Stage II (Mild): Stage II PAD is characterized by intermittent claudication, where patients experience leg pain, cramping, or discomfort during physical activity. Symptoms typically resolve with rest.
- Stage III (Moderate): In Stage III PAD, patients experience more severe intermittent claudication, with pain occurring at shorter walking distances and potentially affecting their daily activities.
- Stage IV (Severe): Stage IV PAD is characterized by critical limb ischemia, where patients experience rest pain, non-healing wounds or ulcers, and tissue necrosis. Severe arterial obstruction puts patients at high risk of limb loss and requires immediate medical intervention.
Rutherford Stages
The Rutherford classification system also divides PAD into four stages based on the severity of symptoms and tissue damage:
- Stage 0 (Asymptomatic): Patients with Stage 0 PAD are asymptomatic and do not exhibit any signs of arterial insufficiency.
- Stage I (Mild): Stage I PAD is characterized by mild claudication, where patients experience intermittent leg pain or discomfort during physical activity but can walk without limitation.
- Stage II (Moderate): In Stage II PAD, patients experience moderate claudication, with pain occurring at shorter walking distances and potentially limiting their daily activities.
- Stage III (Severe): Stage III PAD is marked by severe claudication, rest pain, and tissue loss, indicating critical limb ischemia. Patients are at high risk of limb amputation without prompt intervention.
The Fontaine and Rutherford staging systems provide valuable frameworks for assessing the severity of PAD and guiding treatment decisions based on the patient's clinical presentation and functional status. Early diagnosis and appropriate management are essential for optimizing outcomes and reducing the risk of complications associated with PAD.
Complications of Untreated PAD
Untreated Peripheral Arterial Disease (PAD) can lead to various complications, posing significant risks to an individual's health and well-being.
Increased Risk of Heart Attack and Stroke
PAD shares common risk factors and underlying mechanisms with coronary artery disease (CAD) and cerebrovascular disease, increasing the likelihood of heart attacks and strokes. The atherosclerotic plaques responsible for narrowing peripheral arteries can also affect the coronary arteries supplying the heart and the carotid arteries supplying the brain. Consequently, individuals with untreated PAD are at a heightened risk of developing myocardial infarction (heart attack) and ischemic stroke.
Limb Amputation due to Severe Tissue Damage
In advanced cases of PAD, severe and prolonged arterial insufficiency can result in critical limb ischemia (CLI), a condition characterized by inadequate blood flow to the affected limb. CLI can lead to tissue necrosis, non-healing wounds, and gangrene, significantly increasing the risk of limb amputation. Without timely intervention and revascularization procedures to restore blood flow, the risk of limb loss becomes substantial, profoundly impacting an individual's mobility and quality of life.
Treatment Options for PAD
Effective management of Peripheral Arterial Disease (PAD) focuses on relieving symptoms, improving vascular health, and reducing the risk of complications through a multidisciplinary approach.
Lifestyle Changes
Lifestyle modifications play a fundamental role in PAD management and often form the cornerstone of treatment. Key lifestyle changes include:
- Smoking Cessation: Quitting smoking is crucial for patients with PAD as smoking exacerbates arterial narrowing and impairs blood flow, significantly increasing the risk of complications.
- Exercise: Regular physical activity, particularly walking exercises, can improve arterial blood flow, enhance exercise tolerance, and alleviate symptoms of intermittent claudication.
- Diet: Adopting a heart-healthy diet low in saturated fats, cholesterol, and sodium can help manage PAD risk factors such as hypertension and dyslipidemia, promoting overall cardiovascular health.
Medications
Pharmacological interventions are commonly prescribed to manage PAD and its associated risk factors:
- Antiplatelet Drugs: Medications such as aspirin or clopidogrel are often prescribed to reduce the risk of blood clot formation and cardiovascular events in patients with PAD.
- Cholesterol-Lowering Drugs: Statins are widely used to lower cholesterol levels and stabilize atherosclerotic plaques, slowing the progression of PAD and reducing the risk of cardiovascular events.
Endovascular Procedures
Endovascular interventions are minimally invasive procedures performed to improve blood flow in obstructed arteries:
- Angioplasty: During angioplasty, a catheter with a small balloon at its tip is inserted into the narrowed artery and inflated to widen the vessel, restoring blood flow.
- Stenting: In some cases, a stent—a small mesh tube—is inserted into the artery during angioplasty to help keep it open and prevent re-narrowing (restenosis).
Surgical Interventions
In cases where endovascular procedures are not feasible or effective, surgical interventions may be necessary:
- Bypass Surgery: Bypass surgery involves creating a new pathway for blood flow by grafting a healthy blood vessel from another part of the body or using a synthetic graft to bypass the obstructed artery, restoring adequate circulation to the affected limb.
The choice of treatment modality depends on various factors, including the severity of PAD, the extent of arterial obstruction, the patient's overall health status, and their treatment goals. A personalized treatment plan tailored to the individual's needs and preferences is essential for optimizing outcomes and improving long-term prognosis in PAD management.
Conclusion
Peripheral Arterial Disease (PAD) is a significant vascular condition that demands attention and proactive management. By understanding its causes, recognizing its symptoms, and seeking prompt diagnosis and treatment, individuals can mitigate the risks of complications such as heart attack, stroke, and limb amputation.
Lifestyle modifications, medications, and interventional procedures offer avenues for improving vascular health and enhancing quality of life for those affected by PAD. With awareness and action, we can combat PAD and its detrimental effects, promoting better cardiovascular outcomes and overall well-being.
Effective pain management is paramount for athletes striving for peak performance while minimizing the risk of injury. Understanding the complexities of pain perception, its impact on athletic performance, and implementing comprehensive strategies is vital.
This necessitates a holistic approach encompassing non-pharmacological interventions, training modifications, nutritional considerations, and mental health support. In this blog we will talk about pain management for athletes.
Understanding Pain in Athletes
Understanding pain in athletes involves distinguishing between acute and chronic pain and recognizing their respective durations, causes, symptoms, and management approaches. Below are ways of differentiating between acute and chronic pain in athletes:
| Criteria | Acute Pain | Chronic Pain |
| Duration | Typically, short-term, sudden-onset | Persistent, lasting beyond injury |
| Cause | Often due to recent injury or trauma | Can result from prolonged overuse |
| Symptoms | Sharp, localized pain | Dull, persistent discomfort |
| Management Approach | Focus on immediate relief and healing | Requires comprehensive treatment plan |
Exploring common causes of pain in athletes
Pain is a prevalent issue among athletes, often stemming from various factors related to their rigorous training and competition schedules. Below are the common causes of pain in athletes:
- Overuse injuries: Result from repetitive stress on muscles, tendons, and joints.
- Traumatic injuries: Sudden impacts or accidents during sports activities.
- Poor biomechanics: Incorrect movement patterns leading to strain and injury.
- Muscle imbalances: Weakness or tightness in certain muscle groups predisposing athletes to pain.
- Inadequate rest and recovery: Insufficient time for the body to repair and regenerate tissues.
Impact of pain on athletic performance and overall well-being
Pain not only affects an athlete's physical performance but also has significant implications for their mental and emotional well-being. Below are the impact of pain on athletic performance and overall well-being:
- Reduced performance: Pain can impair movement, agility, and strength, limiting an athlete's ability to perform at their peak.
- Psychological effects: Chronic pain can lead to frustration, anxiety, and depression, impacting motivation and confidence.
- Quality of life: Persistent pain can interfere with daily activities and diminish overall enjoyment of life.
- Risk of further injury: Ignoring pain or overcompensating for it can increase the likelihood of sustaining additional injuries.
- Disruption of training and competition: Pain may necessitate breaks in training or withdrawal from competitions, affecting long-term goals and aspirations.
Strategies for Pain Management
Non-pharmacological approaches are essential in managing pain among athletes, focusing on techniques like physical therapy, stretching, and modalities such as ice and heat therapy.

Non-Pharmacological Approaches
Non-pharmacological approaches play a pivotal role in managing pain effectively among athletes. One of the primary methods is physical therapy, which involves targeted exercises and techniques to improve flexibility, strength, and overall function.
Physical therapists work closely with athletes to develop personalized rehabilitation programs that address the underlying causes of pain and promote healing. Through a combination of therapeutic exercises, manual therapy, and modalities such as ultrasound or electrical stimulation, physical therapy aims to alleviate pain, restore mobility, and prevent future injuries.
Stretching and strengthening exercises are essential components of any pain management regimen for athletes. Stretching helps improve flexibility and range of motion, reducing muscle tension and the risk of strain or injury. Dynamic stretching before exercise and static stretching after can help athletes prepare their bodies for physical activity and aid in recovery post-workout.
Strengthening exercises, on the other hand, target specific muscle groups to enhance stability and support around joints, reducing the likelihood of pain and dysfunction. Incorporating exercises that focus on core strength, balance, and proprioception can help athletes maintain proper biomechanics and prevent overuse injuries.
Modalities such as ice, heat, and massage therapy are commonly utilized by athletes to alleviate pain and promote recovery.
- Ice therapy, or cryotherapy, can help reduce inflammation and numb sore muscles or joints, making it particularly beneficial for acute injuries or post-exercise recovery.
- Heat therapy, in the form of hot packs or warm baths, can help increase blood flow, relax muscles, and alleviate stiffness or chronic pain.
- Massage therapy, whether performed by a licensed therapist or through self-massage techniques, can help release tension, improve circulation, and enhance tissue healing. These modalities can be used alone or in combination to address different types of pain and support overall recovery.
- Rest and recovery are integral components of pain management for athletes. Adequate rest allows the body time to repair and rebuild tissues damaged during exercise or competition, reducing the risk of overuse injuries and chronic pain.
Incorporating rest days into training schedules and prioritizing quality sleep are essential for optimizing recovery and minimizing the impact of pain on athletic performance. Active recovery strategies such as light exercise, foam rolling, or yoga can help promote blood flow, alleviate stiffness, and enhance overall well-being.
Pharmacological Approaches
While non-pharmacological approaches are preferred for managing pain in athletes, pharmacological interventions may be necessary in certain situations. Common pain medications used in sports medicine include nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics, and muscle relaxants.
- NSAIDs, such as ibuprofen or naproxen, work by reducing inflammation and pain, making them effective for treating acute injuries or conditions characterized by swelling and discomfort. Analgesics, such as acetaminophen, provide pain relief without addressing inflammation and are often used for mild to moderate pain management.
- Muscle relaxants may be prescribed to alleviate muscle spasms and promote relaxation in cases of musculoskeletal pain or injury. It is essential for athletes to approach medication use responsibly and under the guidance of a healthcare professional.
While pharmacological interventions can provide temporary relief from pain, they do not address the underlying causes and may carry risks of side effects or adverse reactions. Athletes should be cautious of over-reliance on pain medications, as masking pain without addressing its root cause can lead to further injury or complications.
Certain medications may be prohibited in competitive sports due to their potential for performance enhancement or adverse health effects. Athletes should be informed about the risks and benefits of medication use and work closely with healthcare providers to develop a comprehensive pain management plan that prioritizes safety and long-term well-being.
Balancing Performance and Injury Prevention
Proper technique, varied training regimens, and nutrition play pivotal roles in preventing injuries among athletes, emphasizing the importance of balance between performance enhancement and injury prevention.

Training Modifications
Proper technique and form are paramount in preventing injuries among athletes. By ensuring athletes use correct biomechanics during training and competition, coaches and trainers can help minimize the risk of strain, sprains, and other musculoskeletal injuries. Emphasizing the importance of proper technique from the outset of an athlete's career can instill good habits and reduce the likelihood of injury later on.
Incorporating cross-training and periodization into athletes' training regimens can also play a significant role in injury prevention. Cross-training involves incorporating a variety of activities and exercises into an athlete's routine, which helps prevent overuse injuries by reducing repetitive stress on specific muscles and joints.
Periodization involves systematically varying the intensity, volume, and type of training over time to optimize performance while minimizing the risk of overtraining and injury. By alternating between periods of high-intensity training and periods of rest or lower-intensity activity, athletes can avoid burnout and maintain physical and mental well-being.
Balancing the intensity and volume of training is essential for preventing pain and injury among athletes. Pushing limits and challenging oneself are inherent in athletic pursuits; however, striking a balance between training intensity and recovery is crucial to avoid overtraining and overuse injuries.
Coaches and trainers should monitor athletes' workloads and adjust training plans as needed to prevent excessive fatigue and minimize the risk of injury. Incorporating rest days, recovery sessions, and proper warm-up and cool-down routines into training schedules can help athletes maintain optimal performance while minimizing the risk of pain and injury.
Nutrition and Hydration
Nutrition plays a critical role in pain management and injury prevention for athletes. Consuming a well-balanced diet rich in nutrients is essential for supporting overall health and optimizing athletic performance. Adequate intake of macronutrients such as carbohydrates, protein, and healthy fats provides the energy and building blocks necessary for muscle repair, recovery, and injury prevention.
Micronutrients like vitamins and minerals play key roles in maintaining bone health, immune function, and muscle contraction. Hydration is equally important for athletes, as even mild dehydration can impair muscle function, decrease exercise performance, and increase the risk of cramps and heat-related illnesses.
Athletes should strive to maintain proper fluid balance by drinking water regularly throughout the day and during training and competition. Electrolyte-rich sports drinks can be beneficial for replacing fluids and minerals lost through sweat during intense exercise, particularly in hot or humid conditions.
Certain nutrients have been shown to support muscle recovery and injury prevention among athletes. For example, consuming adequate protein helps repair and rebuild muscle tissue damaged during exercise, reducing the risk of overuse injuries and promoting recovery between workouts.
Omega-3 fatty acids, found in foods like fatty fish and flaxseeds, have anti-inflammatory properties that may help reduce exercise-induced muscle soreness and inflammation. Antioxidants, found in fruits, vegetables, and other plant-based foods, can help combat oxidative stress and promote tissue repair and regeneration.
Mental Health and Stress Management
The impact of stress and mental health on pain perception cannot be understated in the realm of athletic performance. Stress, whether from external pressures or internal anxieties, can exacerbate the perception of pain and impair an athlete's ability to cope with discomfort.
Addressing stressors and prioritizing mental health is essential for promoting resilience and optimizing pain management strategies among athletes. Exploring techniques such as mindfulness, visualization, and relaxation can help athletes manage stress and reduce pain perception.
- Mindfulness practices, such as meditation and deep breathing exercises, promote present-moment awareness and can help athletes cultivate a sense of calm and focus amidst challenging circumstances.
- Visualization techniques involve mentally rehearsing movements or scenarios to enhance performance and reduce anxiety associated with pain or injury.
- Relaxation techniques, such as progressive muscle relaxation or guided imagery, can help athletes release tension and promote physical and mental relaxation. Seeking professional help for mental health issues affecting pain is crucial for athletes facing significant challenges.
Sports psychologists and mental health professionals can provide athletes with coping strategies, support, and guidance to navigate the psychological aspects of pain and injury. By addressing underlying emotional and psychological factors, athletes can better manage pain, enhance resilience, and maintain overall well-being.
Conclusion
Prioritizing pain management in athletes requires a multifaceted approach that addresses the physical, mental, and emotional aspects of well-being. By integrating non-pharmacological techniques, training modifications, nutritional support, and mental health strategies, athletes can optimize performance while minimizing the risk of pain and injury. Embracing this holistic approach fosters long-term success, resilience, and overall well-being in the pursuit of athletic excellence.
Living with chronic pain can be stressful, affecting every aspect of a person's life, from their physical well-being to their emotional and psychological health. Opioid therapy has long been recognized as a cornerstone in managing chronic pain, offering relief and restoring functionality to those who struggle daily with persistent discomfort.
However, the complexities surrounding opioid therapy extend beyond its pain-relieving benefits. The decision to undergo opioid therapy for chronic pain is not one to be taken lightly, as it requires a comprehensive understanding of the benefits and risks involved, as well as a commitment to careful management and monitoring.
The Benefits of Opioid Therapy
Opioid therapy stands as a pillar in the management of chronic pain, offering individuals relief from persistent discomfort that may otherwise severely impact their quality of life.
1. Effective Pain Relief
Opioids are potent analgesic medications that act on the body's opioid receptors to alleviate pain. Unlike many other pain medications, opioids have a unique ability to provide substantial relief, even in cases of severe or refractory pain.
Opioids efficiently reduce pain by attaching to opioid receptors in the brain and spinal cord to alter pain perception and transmission. This analgesic effect is especially helpful for people with chronic pain issues when typical pain treatment techniques may not be effective, such as neuropathic pain, cancer-related pain, or musculoskeletal ailments.
2. Improved Quality of Life
Chronic pain not only causes physical discomfort but also takes a toll on an individual's emotional and psychological well-being, leading to decreased quality of life. Opioid therapy has been shown to significantly enhance the overall quality of life for many individuals living with chronic pain.
Opioids allow patients to participate more completely in everyday activities, social interactions, and recreational pursuits that may have been restricted by pain by effectively lowering pain severity and frequency. Furthermore, the pain relief that opioid medication offers can have a profound impact on mental health, reducing the symptoms of anxiety, stress, and depression related to chronic pain.
3. Increased Functionality and Mobility
The ability of opioid therapy to help people with chronic pain regain their mobility and functionality is one of its main advantages. Opioids allow patients to resume activities of daily life, such as walking, standing, and doing housework, with more ease and comfort as they lessen physical limits and pain.
This restoration of functionality is essential for preserving independence and autonomy, allowing individuals to maintain a sense of normalcy in their lives. Furthermore, opioid therapy can facilitate participation in rehabilitative efforts aimed at improving strength, flexibility, and range of motion.
Administration Methods to Prevent Side Effects
Effective administration of opioid therapy is essential not only for optimizing pain relief but also for minimizing the risk of adverse effects that may accompany its use. Proper dosing, monitoring, and adherence to safe prescribing practices are critical in preventing or mitigating potential side effects associated with opioids
1. Proper Dosage and Monitoring
One of the primary considerations in opioid therapy is ensuring that patients receive the appropriate dosage based on their individual pain levels, medical history, and tolerance to opioids. Starting with the lowest effective dose and titrating gradually based on the patient's response is crucial for preventing overdose and minimizing side effects.
Regular monitoring of patients receiving opioid therapy is essential for detecting signs of inadequate pain control, medication misuse, or adverse reactions. Monitoring may include periodic assessments of pain intensity, functional status, and medication adherence, as well as screening for signs of opioid-related side effects such as constipation, sedation, or respiratory depression.
2. Slow Titration and Careful Adjustment
The principle of "start low and go slow" applies to opioid therapy, particularly when initiating treatment or adjusting dosage levels. Slow titration allows patients to acclimate to the effects of opioids gradually, reducing the likelihood of adverse reactions such as sedation, nausea, or dizziness.
Patients transitioning from short-acting to long-acting opioid formulations or vice versa require careful adjustment of dosage to maintain optimal pain control while minimizing side effects. Individualized treatment plans tailored to the patient's specific needs and circumstances are essential for optimizing the safety and efficacy of opioid therapy.
3. Use of Extended-Release Formulations
Extended-release (ER) or long-acting (LA) opioid formulations offer several advantages over immediate-release (IR) formulations in terms of both efficacy and safety. ER/LA opioids provide sustained pain relief over an extended period, allowing for less frequent dosing and improved medication adherence.
ER/LA formulations help reduce changes in pain intensity and lower the likelihood of breakthrough pain and opioid-related adverse effects by maintaining stable plasma concentrations of opioids. In addition, because of their longer onset of action and tamper-resistant characteristics, ER/LA opioids are less likely to be abused and diverted than IR formulations.
4. Avoidance of Concurrent Sedative Medications
Concurrent use of opioids with other sedative medications, such as benzodiazepines, muscle relaxants, or certain antidepressants, can potentiate central nervous system depression and increase the risk of respiratory depression, sedation, and overdose.
Whenever possible, alternative non-sedating medications or non-pharmacological approaches should be considered to minimize the risk of adverse drug interactions and respiratory complications.
5. Individualized Treatment Plans and Risk Stratification
Opioid therapy should be individualized based on the patient's unique characteristics, including age, comorbidities, concurrent medications, genetic factors, and history of substance abuse or mental health disorders. High-risk patients may require closer monitoring, lower initial doses, and more frequent follow-up visits to ensure their safety and well-being.
When starting opioid medication, healthcare professionals should also involve patients in shared decision-making, going over the advantages, disadvantages, and alternatives to opioids depending on the patient's preferences and treatment objectives. Better treatment outcomes and patient satisfaction are patient-centered care's ultimate goals, which strongly emphasize cooperation, openness, and respect for the patient's autonomy in making decisions.
The Side Effects of Opioid Therapy
Opioids can elicit a range of adverse effects that may impact physical, emotional, and psychological well-being. Identifying the underlying causes of opioid-related side effects is essential for implementing targeted interventions to manage symptoms effectively while minimizing the risk of complications.
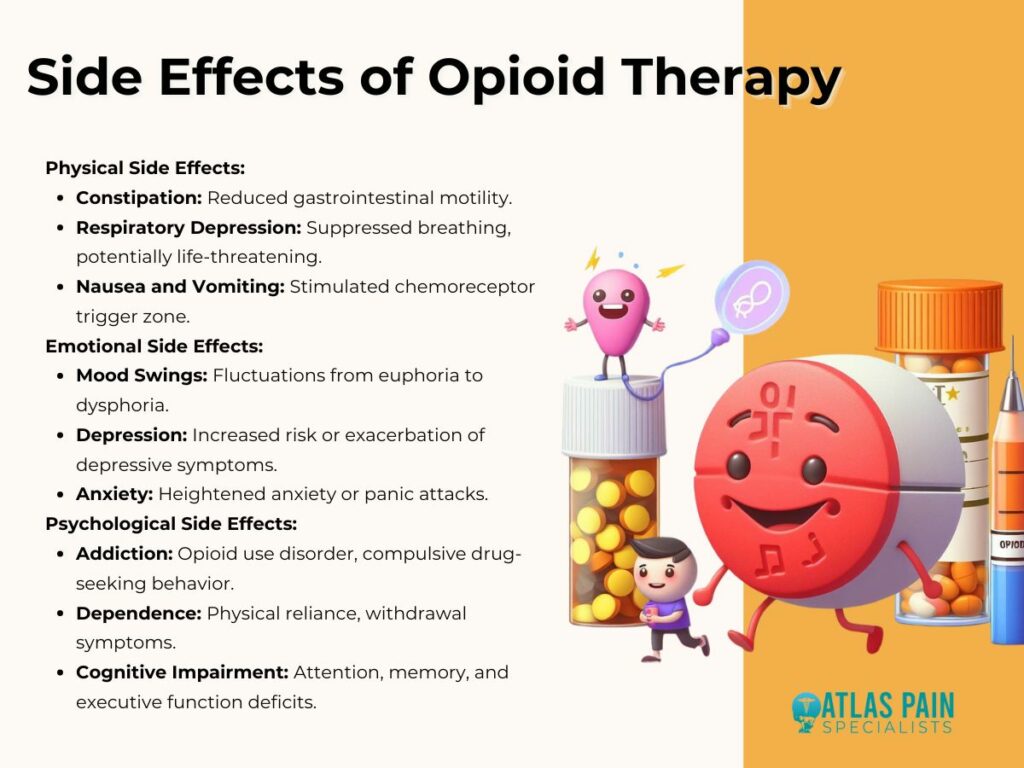
1. Physical Side Effects
- Constipation: Opioids bind to opioid receptors in the gastrointestinal tract, leading to decreased gastrointestinal motility and constipation. This common side effect can significantly impact patients' quality of life and adherence to opioid therapy.
- Respiratory Depression: High doses of opioids can suppress respiratory drive, leading to shallow or slow breathing and potentially life-threatening respiratory depression. Respiratory depression is a serious concern, particularly in patients with underlying respiratory conditions or those receiving concurrent sedative medications.
- Nausea and Vomiting: Opioids can stimulate the chemoreceptor trigger zone in the brain, resulting in nausea and vomiting, especially during initiation of therapy or dose escalation. Antiemetic medications may be prescribed to alleviate these symptoms and improve medication tolerance.
2. Emotional Side Effects
- Mood Swings: Opioids can affect neurotransmitter systems involved in mood regulation, leading to mood fluctuations ranging from euphoria to dysphoria. Patients may experience emotional instability, irritability, or mood swings while on opioid therapy.
- Depression: Prolonged opioid use has been associated with an increased risk of developing depression or exacerbating pre-existing depressive symptoms. The neurobiological mechanisms underlying this association are complex and may involve alterations in neurotransmitter signaling and neuroplasticity.
- Anxiety: Some individuals may experience heightened anxiety or panic attacks while taking opioids, particularly during periods of dose adjustment or withdrawal. Anxiety-related side effects can be distressing and may necessitate adjustments to the opioid regimen or adjunctive treatment with anxiolytic medications.
3. Psychological Side Effects
- Addiction: Opioid use disorder (OUD) is a significant concern associated with long-term opioid therapy, characterized by compulsive drug-seeking behavior, loss of control over drug use, and continued use despite adverse consequences. Genetic predisposition, environmental factors, and neurobiological changes contribute to the development of addiction.
- Dependence: Physical dependence on opioids can occur with prolonged use, leading to withdrawal symptoms upon abrupt discontinuation or dose reduction. Tolerance, the need for escalating doses to achieve the same level of pain relief, is also a hallmark of opioid dependence.
- Cognitive Impairment: Chronic opioid use has been linked to cognitive impairment, including deficits in attention, memory, and executive function. These cognitive side effects can impair daily functioning and quality of life, particularly in elderly patients or those with pre-existing cognitive deficits.
Combining Opioid Therapy with Other Modalities
While opioid therapy can be effective in managing chronic pain, a multimodal approach that combines opioids with other treatment modalities offers several advantages, including enhanced pain relief, reduced opioid requirements, and a lower risk of adverse effects. Integrating non-pharmacological therapies, interventional procedures, and complementary modalities with opioid therapy allows for a more comprehensive and individualized approach to pain management.

1. Multimodal Approach to Pain Management
- Comprehensive Pain Relief: Combining opioids with non-opioid medications, such as NSAIDs, acetaminophen, or adjuvant analgesics, can provide synergistic pain relief by targeting different pain pathways and mechanisms. Multimodal analgesia allows for lower opioid doses, reducing the risk of opioid-related adverse effects while maximizing pain control.
- Addressing Multifactorial Pain: Chronic pain is often multifactorial, involving physical, psychological, and social dimensions. A multimodal approach that addresses these various aspects of pain can lead to more holistic and effective pain management outcomes. Incorporating interventions such as physical therapy, cognitive-behavioral therapy (CBT), and mindfulness-based techniques can help patients develop coping skills, improve functional outcomes, and reduce reliance on opioids for pain relief.
2. Integration of Non-pharmacological Therapies
- Physical Therapy: Physical therapy plays a crucial role in pain management by improving strength, flexibility, and mobility, reducing musculoskeletal pain, and promoting overall physical function. Exercise-based interventions, manual therapy techniques, and modalities such as heat or cold therapy can complement opioid therapy by addressing underlying musculoskeletal dysfunction and promoting tissue healing.
- Cognitive-Behavioral Therapy (CBT): CBT is a psychotherapeutic approach that focuses on modifying maladaptive thoughts, beliefs, and behaviors associated with pain. By teaching patients coping skills, relaxation techniques, and stress management strategies, CBT can help reduce pain intensity, improve mood, and enhance overall coping abilities, thereby reducing the need for opioids and minimizing the risk of psychological side effects.
3. Minimizing Side Effects through Complementary Treatments
- Adjunctive Medications: Certain medications, such as antidepressants, anticonvulsants, or muscle relaxants, can augment the analgesic effects of opioids and target specific pain mechanisms, such as neuropathic pain or muscle spasms. Adding adjunctive medications to opioid therapy can improve pain relief, reduce opioid requirements, and mitigate the risk of opioid-related side effects.
- Integrative Therapies: Integrative therapies, including acupuncture, massage therapy, chiropractic care, and biofeedback, offer additional avenues for pain management while minimizing reliance on opioids. These modalities can modulate pain perception, promote relaxation, and enhance overall well-being, providing patients with alternative strategies for managing pain and improving quality of life.
Are Alternative Pain Management Techniques Effective?
Even though opioids can be quite helpful for those with chronic pain, there are risks and restrictions associated with them that should be carefully considered and closely monitored. We can maximize treatment success while lowering the danger of side effects by understanding the advantages of opioid therapy, putting safe delivery techniques into practice, and investigating coping mechanisms and substitutes.
The inclusion of alternative pain management approaches in an opioid treatment plan is important in delivering patient-centered, holistic care. This conversation naturally led to the question, "Are Alternative Pain Management Techniques Effective?" which encourages additional research into complementary therapies, interventional techniques, and non-pharmacological interventions that provide effective substitutes for opioids.
Through fostering communication across traditional and non-traditional pain care modalities, patients have a more customized and varied toolkit to manage their pain and reduce their dependency on opioids.
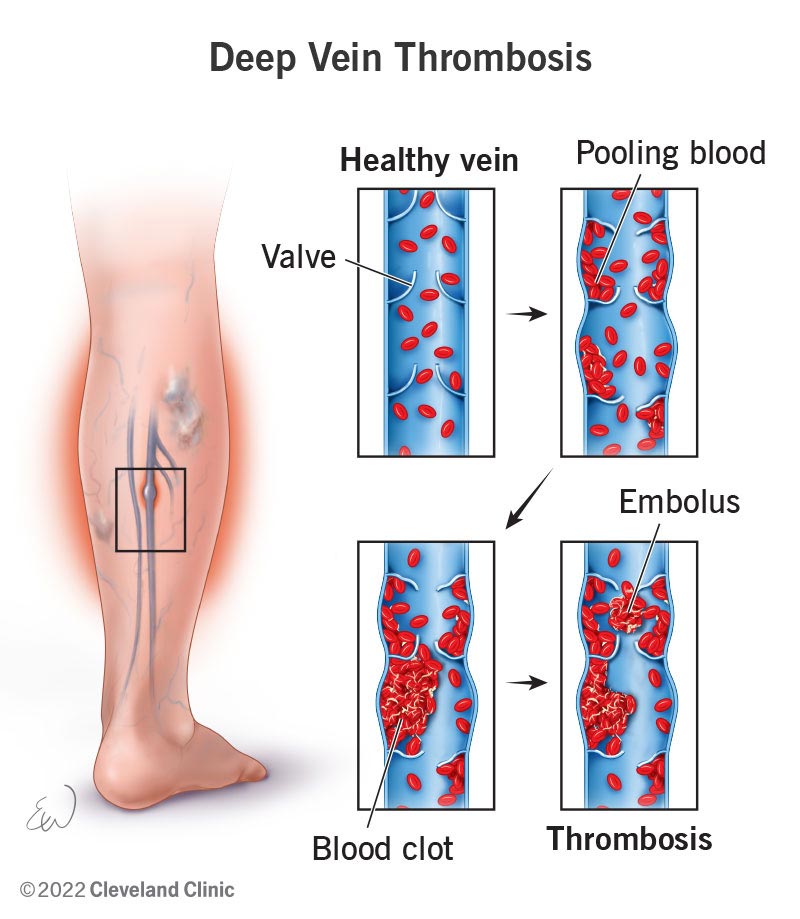
A blood clot in a deep vein, usually in the legs, can cause a medical disorder called deep vein thrombosis (DVT). Though DVT can affect any deep vein, the legs are most commonly involved, leading to not only local discomfort but also the potential for serious complications.
The implications of an untreated DVT extend beyond immediate health concerns, as clots can dislodge and travel to the lungs, causing a life-threatening pulmonary embolism. The pathophysiology of DVT is complex, influenced by factors neatly categorized by Virchow's Triad with elements that contribute to its risk and development. Let as now delve into a comprehensive guide to deep vein thrombosis.
What is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis (DVT) is a condition characterized by the formation of a blood clot, or thrombus, within a deep vein in the body. Although DVT can occur in any deep vein, it most commonly affects those in the legs, including the calves, thighs, or pelvis.
The concern with DVT extends beyond the local symptoms it may cause, such as pain, swelling, and redness. The development of DVT is influenced by several factors, including lifestyle risks such as smoking, genetic risks such as inherited clotting disorders (Factor V Leiden), and health-related risks such as certain cancers and their treatments.
The Pathophysiology of DVT
Central to the pathophysiology of DVT is the Virchow's Triad. It outlines the three primary conditions that predispose individuals to thrombosis: venous stasis, vascular injury, and hypercoagulability.
Additionally, whether the DVT is actute or chronic has an impact on the condition's full spectrum, from initial onset to potential long-term management.
- Venous Stasis
Venous stasis occurs when the normal flow of blood through the veins is slowed or interrupted, a common predisposing factor for DVT. This condition is particularly prevalent in individuals who are immobilized for long periods, such as those undergoing prolonged bed rest, travelers on long flights, or patients with paralysis.
Venous stasis leads to an accumulation of blood in the lower limbs, increasing the contact time between blood components and the vein walls. This prolonged contact time facilitates the aggregation of clotting factors and the formation of thrombi.
- Vascular Injury
Vascular injury to the inner lining of the vein (endothelium) is another critical component of Virchow's Triad. Such injuries can result from surgical procedures, traumatic events, or the insertion of intravenous catheters.
The damage to the endothelium triggers the body's natural coagulation cascade as a repair mechanism. However, this process can become pathological if the coagulation is excessive, leading to thrombus formation within the vein.
- Hypercoagulability
Hypercoagulability refers to an increased tendency of the blood to clot, which can be inherited or acquired. Conditions such as Factor V Leiden or prothrombin gene mutation, antiphospholipid syndrome, and certain cancers can inherently increase clotting risk.
Acquired hypercoagulability may result from hormone therapy, pregnancy, or cancer. This heightened state of coagulability significantly elevates the risk of forming thrombi.
Types of DVT and Severity Scale
Deep Vein Thrombosis (DVT) can be classified based on the location of the clot within the venous system. This classification into proximal and distal DVT is critical for assessing the risk of complications, guiding treatment decisions, and understanding the potential outcomes associated with each type.
The severity scale of DVT hinges on this classification, influencing both immediate management strategies and long-term care.
1. Proximal DVT
Proximal DVT refers to clots that occur in the deep veins located above the knee, including the popliteal, femoral, and iliofemoral veins. These veins are responsible for carrying a significant portion of the blood back to the heart from the lower limbs.
Due to their larger diameter and the higher volume of blood they handle, clots in these veins pose a greater risk for serious complications, such as pulmonary embolism.
2. Distal DVT
Distal DVT, also known as calf vein thrombosis, involves clots in the deep veins below the knee, such as the peroneal, tibial, and gastrocnemius veins. While these clots are generally considered less dangerous than proximal DVTs, they are not without risk.
There is a potential for distal DVTs to extend into the proximal veins, thereby increasing the risk of pulmonary embolism.
3. Acute vs. Chronic DVT
Acute DVT refers to the initial phase of thrombus formation and is characterized by sudden symptoms such as swelling, pain, and redness in the affected limb. The immediate implications of acute DVT include the risk of the clot growing or dislodging and causing a pulmonary embolism. Prompt diagnosis and treatment are essential to mitigate these risks.
Chronic DVT refers to the long-term consequences that can arise after an initial DVT episode, including the possibility of post-thrombotic syndrome (PTS). PTS can result in chronic pain, swelling, and discoloration of the affected limb, and, in severe cases, venous ulcers.
Symptoms of Deep Vein Thrombosis (DVT)
It's important to note that DVT can occur without any noticeable symptoms. Therefore, being aware of the risk factors and preventive measures is crucial, especially for individuals with a high risk of developing blood clots.
DVT symptoms can vary from subtle to pronounced, and in some cases, the condition may be asymptomatic. However, when symptoms do occur, they typically manifest in the affected limb and may include the following:
Common Symptoms
- Swelling: One of the most noticeable signs of DVT is swelling in the leg, ankle, or foot on one side. It can come on gradually or suddenly, depending on the size and location of the clot.
- Pain: DVT can produce pain that feels like cramps or soreness and frequently begins in the calf. When walking or standing, the pain could get greater.
- Warmth: The skin around the painful area may feel warmer to the touch compared to surrounding areas.
- Red or Discolored Skin: The affected leg may show redness or a noticeable discoloration, which is a sign of inflammation and reduced blood flow.
- Enlarged Veins: Veins near the skin's surface may become more visible or feel firm or enlarged.
Signs That Require Immediate Medical Attention
- Severe Swelling and Pain: Sudden and severe swelling and pain in the leg, especially if accompanied by the symptoms listed above, necessitate prompt medical evaluation to rule out DVT.
- Difficulty Breathing: Pulmonary embolism is a condition marked by abrupt dyspnea, fast heartbeat, disorientation, and chest pain that may get worse with deep breathing if a clot breaks free and goes to the lungs. This is a medical emergency that has to be treated right away.
- Coughing Blood: Coughing up blood is a severe symptom that can indicate a pulmonary embolism, and urgent medical care is essential.
Diagnosis of Deep Vein Thrombosis (DVT)
Diagnosing Deep Vein Thrombosis (DVT) involves a combination of clinical assessment, imaging studies, and laboratory tests. Accurate diagnosis allows for timely and appropriate treatment to prevent the progression of the clot and reduce the risk of complications.
Here’s an overview of the diagnostic process for DVT:
1. Clinical Assessment
- Patient History: The initial step involves a thorough review of the patient's medical history, including any previous episodes of DVT, family history of blood clots, and potential risk factors such as recent surgeries, immobility, or underlying health conditions.
- Physical Examination: A physical examination is conducted to check for signs of DVT, such as swelling, warmth, redness, and tenderness along the vein's path. However, these symptoms can be similar to other conditions, making further diagnostic testing necessary for confirmation.
2. Imaging Studies
- Ultrasound: The most common imaging test for diagnosing DVT, an ultrasound uses sound waves to create images of blood flow in the veins. A Doppler ultrasound can specifically detect irregularities in the flow of blood, indicative of a clot.
- Venography: Although less commonly used today due to the invasiveness of the procedure, venography can be employed in complex cases. A contrast dye is injected into a large vein in the foot or ankle, and X-rays are taken to visualize the veins in the legs
3. Laboratory Tests
- D-dimer Test: A D-dimer test measures a substance that is released when a blood clot breaks down. High levels of D-dimer in the blood can indicate the presence of an active clotting process. However, elevated D-dimer levels can be caused by various factors other than DVT, making the test non-specific. Therefore, a positive D-dimer test is usually followed by imaging studies for confirmation of DVT.
Other Diagnostic Tests
In some cases, when ultrasound results are inconclusive and the patient's clinical probability of DVT is high, additional imaging tests may be required. These could include:
- MRI (Magnetic Resonance Imaging): MRI can provide detailed images of the veins and may be used in cases where ultrasound is inconclusive, particularly for pelvic or abdominal veins.
- CT Venography: For detecting clots in the pelvis and abdomen, CT venography can be an option, involving the injection of contrast material and CT imaging.
Treatment Options for Deep Vein Thrombosis (DVT)
The treatment of Deep Vein Thrombosis (DVT) is aimed at preventing the clot from growing and reducing the risk of complications, such as a pulmonary embolism. Treatment strategies can vary based on the location of the clot, the patient's overall health, and the presence of any underlying conditions.
Here are the primary treatment options for DVT:
1. Anticoagulants (Blood Thinners)
Anticoagulants, commonly called blood thinners, decrease the blood's ability to clot. They don't break up existing clots but can prevent clots from getting bigger and reduce the risk of additional clots forming.
Anticoagulants include warfarin (Coumadin) and direct oral anticoagulants (DOACs) such as rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa). The choice of medication depends on the individual's specific situation, with DOACs offering the advantage of not requiring regular blood monitoring.
2. Thrombolytics (Clot Busters)
In severe cases of DVT, especially when there is a significant threat to limb viability, thrombolytics may be used. These drugs can dissolve blood clots quickly but are associated with a higher risk of bleeding than anticoagulants.
Thrombolytic therapy is typically reserved for life-threatening situations, such as a severe pulmonary embolism or phlegmasia cerulea dolens (a rare form of DVT that threatens limb loss).
3. Compression Stockings
Compression stockings are designed to prevent swelling and reduce the chance of complications of DVT. By applying pressure to the lower legs, they help maintain blood flow and decrease the risk of post-thrombotic syndrome.
They are often recommended for at least two years after a DVT diagnosis to manage symptoms and prevent long-term complications.
4. Inferior Vena Cava (IVC) Filters
An IVC filter can be an alternative for patients who are medically unable to take anticoagulants. Blood clots are prevented from reaching the lungs by placing this tiny device into the inferior vena cava, a major vein that returns blood from the lower body to the heart.
IVC filters are generally used as a temporary measure, and in some cases, they may be removed once the risk of pulmonary embolism decreases.
5. Lifestyle and Home Remedies
- Physical Activity: Staying active and moving around as soon as possible after surgery or during prolonged bed rest can help prevent clots from forming.
- Hydration: Drinking plenty of fluids can prevent dehydration, which is a risk factor for DVT.
6. Surgical and Other Procedures
- Catheter-directed thrombolysis: This minimally invasive procedure involves threading a catheter to the site of the clot and delivering thrombolytic drugs directly to dissolve it.
- Venous thrombectomy: In rare cases, surgery might be necessary to remove a large vein clot, particularly if it's causing significant symptoms and other treatments aren't effective.
The Role of Physical Therapy in Pain Management
Deep Vein Thrombosis (DVT) represents a significant health concern with potential for serious complications, emphasizing the importance of early detection, effective treatment, and diligent management. The process of learning about DVT fundamentals and working through treatment and prevention choices highlights how difficult it is to manage the condition.
Central to this journey is the integration of medical interventions, lifestyle modifications, and supportive therapies tailored to individual needs. For patients recovering from DVT, physical therapy offers a targeted approach to alleviate pain, improve circulation, and restore function in the affected limb.
Through personalized exercise programs, patients can safely engage in activities designed to enhance venous return, reduce swelling, and prevent the stiffness and discomfort often associated with DVT and its aftermath, such as post-thrombotic syndrome (PTS).
Welcome to our exploration of temperature-based therapies, where the fusion of ancient wisdom and contemporary science leads to profound healing.
Throughout our journey, we'll delve into the transformative capabilities of heat and cold therapy. These age-old practices, cherished for centuries, offer more than mere relief from discomfort; they serve as gateways to restoration, rejuvenation, and revitalization.
Join us in exploring the benefits of heat and cold therapy for pain relief.
Understanding Heat Therapy
Heat therapy, also known as thermotherapy, is a therapeutic technique that involves the application of heat to the body to promote healing and alleviate pain. When heat is applied to the skin, it penetrates deep into the tissues, causing blood vessels to dilate.
This increase in blood flow brings a surge of oxygen and nutrients to the affected area while aiding in the removal of metabolic waste products. The fundamental principle behind heat therapy lies in its ability to induce vasodilation, the widening of blood vessels.
Consequently, heat therapy promotes tissue relaxation, reduces muscle spasms, and enhances flexibility and mobility.
Benefits of Heat Therapy for Pain Relief and Healing
Heat therapy offers numerous benefits for pain relief and healing, making it a popular choice for individuals seeking natural remedies. Here are some key advantages:
1. Muscle Relaxation
Heat therapy helps relax muscles, reducing tension and stiffness.
2. Improved Circulation
Heat promotes blood flow, delivering oxygen and nutrients to tissues, aiding in healing.
3. Pain Relief
Heat can alleviate discomfort by blocking pain signals and reducing sensitivity in nerve endings.
4. Joint Flexibility
Heat therapy enhances joint flexibility and range of motion, beneficial for conditions like arthritis.
5. Stress Reduction
Heat induces relaxation, easing stress and tension in both body and mind.
6. Enhanced Healing
Heat accelerates tissue repair and regeneration, aiding in recovery from injuries or surgeries.
7. Versatility
Heat therapy can be applied in various forms, making it convenient and accessible for different needs and preferences.
By harnessing the power of heat therapy, individuals can experience relief from pain and discomfort while promoting healing and relaxation throughout the body.
Types and Applications of Heat Therapy
Heat therapy encompasses various methods, each with specific applications:
1. Moist Heat Therapy
Utilizes moisture-producing sources like warm towels or steam baths. Ideal for deep tissue penetration, it's beneficial for muscle strains, arthritis, and menstrual cramps.
2. Dry Heat Therapy
Involves sources like heating pads or heat wraps, which don't produce moisture. Convenient and easy to apply, it's effective for muscle relaxation, minor aches, and stiffness.
3. Heating Pads
Versatile devices offering targeted therapy, commonly used for pain relief and improving circulation in specific areas.
4. Warm Baths (Hydrotherapy)
Immersing in warm water promotes relaxation and relieves muscle tension, joint stiffness, and stress.
5. Heat Packs or Wraps
Portable devices filled with heat-retaining materials, suitable for on-the-go therapy targeting specific areas of discomfort.
6. Infrared Heat Therapy
Penetrates deep into tissues, providing relief for chronic conditions like arthritis, fibromyalgia, and improving circulation.
7. Hot Stone Therapy
Uses heated stones placed on the body to relax muscles, improve circulation, and alleviate stress, often integrated into massage therapy sessions.
Understanding these types and their applications allows individuals to select the most suitable heat therapy for their specific needs, promoting pain relief, relaxation, and overall well-being.
Precautions and Considerations
While heat therapy is generally safe and well-tolerated, certain precautions should be observed:
- Avoid prolonged exposure to high temperatures, as it can lead to burns or skin irritation.
- Individuals with sensory impairments, circulatory disorders, or diabetes should use heat therapy cautiously and under the guidance of a healthcare professional.
- Heat therapy should not be applied to areas of acute inflammation or recent injuries, as it can exacerbate swelling and pain.
Understanding Cold Therapy
Cold therapy, also referred to as cryotherapy, is a therapeutic technique that involves the application of cold or ice to the body to reduce pain, inflammation, and promote healing. The primary mechanism of cold therapy lies in its ability to induce vasoconstriction, the narrowing of blood vessels.
When cold is applied to the skin, it causes blood vessels to constrict, reducing blood flow to the affected area. This decrease in blood flow helps to reduce inflammation, swelling, and pain sensation by numbing nerve endings.
Benefits of Cold Therapy for Pain Relief and Healing
By employing cold temperatures on the body, this treatment presents a range of benefits, including inflammation reduction, pain mitigation, and expedited recovery. Here are some of the key advantages:
1. Reduced Inflammation
Cold therapy causes vasoconstriction, narrowing blood vessels to reduce blood flow and inflammation. This is particularly effective for acute injuries, swelling, and inflammation associated with conditions like arthritis.
2. Pain Relief
Cold numbs nerve endings, providing temporary pain relief by reducing the transmission of pain signals to the brain. It's beneficial for acute injuries, migraines, and post-surgical recovery.
3. Muscle Recovery
Cold therapy helps alleviate muscle soreness and speed up recovery after intense exercise or physical activity. It can reduce muscle fatigue, inflammation, and the risk of delayed onset muscle soreness (DOMS).
4. Joint Pain Management
Cold therapy is effective for managing joint pain and stiffness associated with conditions like osteoarthritis and rheumatoid arthritis. It can improve mobility and reduce discomfort by decreasing inflammation in the affected joints.
5. Accelerated Healing
Cold therapy can promote faster healing by reducing swelling and inflammation, which can inhibit the healing process. By minimizing tissue damage and promoting vasoconstriction, cold therapy supports the body's natural healing mechanisms.
6. Migraine Relief
Cold therapy applied to the head or neck during a migraine attack can help alleviate pain and reduce the severity of symptoms. The cold temperature constricts blood vessels in the head, providing relief from throbbing pain and associated symptoms like nausea and sensitivity to light.
7. Post-Exercise Recovery
Cold therapy, such as ice baths or cold compresses, can aid in post-exercise recovery by reducing muscle inflammation and soreness. Athletes often use cold therapy to speed up recovery between training sessions and competitions.
Understanding the benefits of cold therapy can help individuals effectively incorporate it into their pain management and recovery routines, leading to improved overall well-being and quality of life.
Types and Applications of Cold Therapy
Cold therapy can be administered through various methods, each offering unique benefits and applications:
1. Ice Packs
Portable and convenient, ice packs are commonly used for localized cold therapy. They are applied directly to the skin over the affected area to reduce inflammation, swelling, and pain associated with acute injuries, such as sprains, strains, and bruises.
2. Cold Compresses
Similar to ice packs, cold compresses consist of a cloth or towel soaked in cold water and applied to the skin. They are effective for treating minor injuries, muscle soreness, and inflammation, providing localized relief.
3. Ice Massage
Ice massage involves using ice cubes or frozen massage tools to apply cold therapy directly to the skin in a circular motion. It's beneficial for targeting specific areas of pain or inflammation, such as tendonitis, bursitis, or muscle spasms.
4. Cold Baths or Immersion Therapy
Immersing the body in cold water, such as an ice bath or cold water immersion therapy, is commonly used by athletes to accelerate recovery after intense exercise or competition. Cold baths reduce muscle inflammation, soreness, and fatigue, promoting faster recovery and preventing injury.
5. Cold Sprays or Aerosols
Cold sprays or aerosols deliver a burst of cold temperature to the skin, providing immediate pain relief for minor injuries, strains, and sprains. They are convenient for on-the-go use and are often found in first aid kits or athletic training rooms.
6. Cryotherapy Chambers
Whole-body cryotherapy involves exposing the entire body to extremely cold temperatures for a short duration in a specialized chamber. It's used to reduce inflammation, alleviate pain, and promote recovery from injuries, chronic conditions, and muscle soreness.
7. Cold Compression Therapy
Combining cold therapy with compression, cold compression therapy devices apply controlled cold and pressure to the affected area. This method reduces swelling, inflammation, and pain while improving blood circulation, making it effective for post-surgery recovery, sports injuries, and chronic conditions like arthritis.
Understanding the types and applications of cold therapy allows individuals to choose the most suitable method for their specific needs, whether it's reducing inflammation, relieving pain, or promoting recovery after injury or intense physical activity.
Precautions and Considerations
Cold therapy, while beneficial, requires careful handling. Here are key points to consider:
- Limit exposure. Avoid prolonged cold exposure.
- Check skin sensitivity. Be cautious with sensitive skin.
- Use it properly. Wrap cold packs and avoid direct contact with ice.
- Be cautious with immersion. Monitor immersion duration.
- Watch for reactions. Monitor for adverse skin reactions.
- Consider health conditions. Consult a healthcare professional.
Following these guidelines ensures safe and effective use of cold therapy in pain management and recovery. Always seek advice from a healthcare professional, especially if you have specific health concerns.
Summary
Throughout our investigation, we've revealed the notable benefits of both heat and cold therapy. Heat therapy brings relaxation, enhances circulation, and alleviates pain, making it ideal for addressing muscle tension and improving joint mobility. Conversely, cold therapy diminishes inflammation, numbs discomfort, and facilitates recovery, offering relief for acute injuries and joint discomfort.
These natural remedies provide accessible solutions for pain management and healing, fostering overall well-being without the reliance on medication or invasive interventions.
Shin splints and stress fractures stand as prevalent lower limb injuries among athletes, posing significant challenges to their performance and well-being. These conditions often arise from overuse, biomechanical factors, and training errors, impacting individuals engaged in high-impact sports and activities.
Understanding the distinct characteristics, prevention strategies, and treatment approaches for shin splints and stress fractures is paramount for athletes, coaches, and healthcare professionals alike.
In this comprehensive guide, we explore the causes, symptoms, prevention, and treatment of shin splints and stress fractures, aiming to equip individuals with the knowledge and tools necessary to mitigate the risk of these injuries and optimize recovery outcomes.
Identifying the Causes of Shin Splints
Shin splints, medically known as medial tibial stress syndrome (MTSS), refer to pain along the shinbone (tibia), the large bone in the front of the lower leg.
Common causes of shin splints include overuse, biomechanical issues, and inadequate footwear. These factors lead to repetitive stress on the shinbone during activities like running or jumping. Overuse, biomechanical problems, and poor footwear contribute to muscle fatigue and increased strain on the shins. Understanding these causes is vital for preventing and managing shin splints in athletes.
1. Overuse and Repetitive Stress
Shin splints often occur due to repetitive stress on the shinbone and surrounding muscles. Activities such as running, jumping, dancing, or high-impact sports can lead to microtrauma in the muscles and bones of the lower leg.
2. Biomechanical Issues
Faulty biomechanics, such as overpronation (excessive inward rolling of the foot), flat feet, or high arches, can contribute to the development of shin splints. These biomechanical abnormalities can alter the distribution of forces along the lower extremities, increasing stress on the shins.
3. Inadequate Footwear
Wearing improper or worn-out footwear lacking adequate support and cushioning can exacerbate the impact on the lower legs, predisposing individuals to shin splints. Shoes that do not provide sufficient shock absorption can increase the strain on the shinbone and surrounding tissues.
4. Sudden Increase in Intensity or Duration of Activity
Abruptly ramping up the intensity, duration, or frequency of exercise without allowing adequate time for the body to adapt can overload the muscles and bones of the lower leg, leading to shin splints.
5. Hard or Uneven Surfaces
Training on hard or uneven surfaces, such as concrete or uneven terrain, can increase the impact on the lower limbs, contributing to the development of shin splints.
6. Muscle Weakness or Imbalance
Weakness or imbalance in the muscles of the lower leg, particularly the calf muscles and anterior tibialis, can impair shock absorption and stability, predisposing individuals to shin splints.
By understanding these underlying causes, athletes can implement preventive measures and effectively manage shin splints for sustained performance and well-being.
Identifying the Causes of Stress Fractures
Stress fractures, frequently seen in athletes, stem from multiple factors. Overuse, sudden training intensity changes, and biomechanical issues like flat feet contribute to their occurrence. Poor bone density and nutritional deficiencies also heighten the risk. Recognizing these causes is crucial for prevention and management in athletes.
1. Overuse and Repetitive Stress
Like shin splints, stress fractures often result from repetitive stress and overuse of the bones in the lower extremities. Activities involving repetitive pounding or impact, such as running, jumping, or gymnastics, can lead to microfractures in the bones over time.
2. Sudden Increase in Training Intensity
A rapid escalation in training intensity, duration, or frequency without adequate rest or recovery periods can overwhelm the body's ability to repair and remodel bone tissue, increasing the risk of stress fractures.
3. Poor Bone Density
Individuals with low bone density, such as those with osteoporosis or osteopenia, are more susceptible to stress fractures as their bones are less resilient to repetitive stress.
4. Biomechanical Factor
Structural abnormalities or biomechanical issues, such as flat feet, high arches, leg length discrepancies, or improper gait mechanics, can alter the distribution of forces along the lower limbs, predisposing certain bones to stress fractures.
5. Inadequate Nutrition
Nutritional deficiencies, particularly in calcium and vitamin D, can weaken bones, making them more susceptible to stress fractures. Proper nutrition is essential for maintaining bone health and integrity.
6. Female Athlete Triad
In female athletes, the triad of disordered eating, amenorrhea (absence of menstruation), and osteoporosis can significantly increase the risk of stress fractures due to hormonal imbalances and decreased bone density.
Understanding these underlying causes is crucial for implementing preventive strategies and designing effective treatment and rehabilitation plans for individuals with shin splints and stress fractures.
By addressing contributing factors and modifying training regimens accordingly, athletes can reduce their risk of these debilitating injuries and optimize their overall performance and well-being.
Common Symptoms of Shin Splints
Shin splints and stress fractures present distinct sets of symptoms, both commonly affecting athletes engaged in high-impact activities. Shin splints typically manifest as pain along the shinbone during or after exercise, accompanied by tenderness and swelling.
1. Pain Along the Shinbone
The primary symptom of shin splints is pain along the inner edge of the shinbone (tibia).
2. Pain During or After Activity
Pain typically develops during or after physical activity, particularly running, jumping, or other high-impact exercises.
3. Tenderness and Swelling
Tenderness and swelling may be present along the shinbone, often accompanied by mild to moderate swelling.
4. Dull or Aching Pain
The pain associated with shin splints is often described as dull, aching, or throbbing in nature.
5. Pain Alleviated by Rest
Symptoms may improve with rest but can worsen upon resuming activity.
Recognizing these symptoms is crucial for early intervention and effective management of shin splints. If experiencing persistent or worsening pain, it is essential to seek medical evaluation for proper diagnosis and treatment.
Common Symptoms of Stress Fractures
In contrast, stress fractures exhibit localized pain in specific areas of the lower leg or foot, worsening with activity and often accompanied by swelling and tenderness. Understanding these characteristic symptoms is crucial for accurate diagnosis and appropriate management of these common lower limb injuries in athletes.
1. Localized Pain
Stress fractures cause localized pain in a specific area of the affected bone, typically the lower leg or foot.
2. Pain Worsens with Activity
Pain tends to worsen during weight-bearing activities, such as walking, running, or jumping, and may subside with rest.
3. Swelling and Tenderness
Swelling, tenderness, and bruising may be present over the site of the stress fracture.
4. Pain at Night
Pain may persist even at rest, and individuals may experience increased discomfort, particularly at night.
5. Sudden Onset of Severe Pain
In some cases, stress fractures may present with a sudden onset of severe pain, particularly with a direct impact or sudden increase in activity.
Recognizing these symptoms is crucial for early diagnosis and timely intervention to prevent further complications and facilitate optimal recovery in individuals with shin splints and stress fractures.
Preventing Shin Splints and Stress Fractures in Athletes
Shin splints and stress fractures are often preventable with proper attention to training techniques, equipment, and lifestyle factors. Effective prevention strategies can significantly reduce the risk of these injuries in athletes. Below are guidelines for preventing shin splints and stress fractures:
1. Gradual Progression
Gradually increase the intensity, duration, and frequency of exercise to allow the body to adapt and minimize the risk of overuse injuries.
2. Proper Footwear
Wear appropriate footwear with adequate support and cushioning, suitable for the specific activity and individual biomechanics.
3. Surface Selection
Choose softer, even surfaces for training whenever possible to reduce the impact on the lower limbs.
4. Cross-Training
Incorporate cross-training activities to diversify the stress on muscles and bones, reducing the risk of overuse injuries.
5. Strength and Flexibility
Maintain good lower limb strength and flexibility through targeted exercises, focusing on the calf muscles, anterior tibialis, and surrounding musculature.
6. Biomechanical Assessment
Identify and address biomechanical abnormalities or gait issues through professional assessment and appropriate interventions, such as orthotics or gait retraining.
7. Nutrition and Hydration
Ensure adequate intake of nutrients essential for bone health, including calcium, vitamin D, and magnesium, and maintain proper hydration levels.
Treatment Strategies for Shin Splints and Stress Fractures
Effective treatment strategies for shin splints and stress fractures are crucial for athletes aiming to recover swiftly and return to their sport. Treatment typically involves a combination of rest, pain management, rehabilitation exercises, and addressing underlying factors contributing to the injuries. Timely intervention and adherence to treatment protocols are essential to ensure optimal recovery outcomes and prevent long-term complications.
1. Rest
Rest the affected limb to allow for healing and alleviate symptoms. Avoid activities that exacerbate pain until symptoms resolve.
2. Ice and Compression
Apply ice packs and use compression wraps to reduce pain and inflammation, particularly during the acute phase of injury.
3. Pain Management
Over-the-counter pain relievers such as ibuprofen or acetaminophen may help alleviate discomfort associated with shin splints and stress fractures.
4. Stretching and Strengthening
Perform gentle stretching exercises for the calf muscles, Achilles tendon, and anterior tibialis to improve flexibility and prevent muscle imbalances. Gradually incorporate strengthening exercises to enhance muscle stability and support.
5. Physical Therapy
Seek guidance from a physical therapist for personalized rehabilitation programs focusing on restoring function, addressing biomechanical issues, and preventing recurrence.
6. Orthotics and Supportive Devices
Consider using orthotic inserts or supportive devices, such as braces or splints, to provide additional stability and cushioning during activity.
7. Gradual Return to Activity
Once symptoms improve, gradually reintroduce activity, starting with low-impact exercises and gradually progressing to higher-intensity activities.
8. Medical Evaluation
Consult with a healthcare professional if symptoms persist or worsen despite conservative measures, as further evaluation may be necessary to rule out underlying conditions or complications.
By implementing these preventive measures and appropriate treatment strategies, athletes can effectively manage shin splints and stress fractures, minimize downtime, and safely return to their sport or activity with reduced risk of recurrence.
However, it's essential to listen to your body, seek professional guidance when needed, and prioritize long-term musculoskeletal health and injury prevention.
Summary
In summary, understanding the nuances between shin splints and stress fractures is vital for athletes and sports enthusiasts alike. Both injuries, though distinct in nature, share commonalities in terms of causes, symptoms, prevention, and treatment.
By recognizing the signs early, implementing preventive measures, and seeking timely intervention, individuals can mitigate the risk of these debilitating conditions and facilitate optimal recovery. To sustain participation in sports and activities while safeguarding overall well-being, it is imperative to prioritize long-term musculoskeletal health through proper training techniques, adequate rest, and injury prevention strategies.
With a proactive approach to injury management and a focus on comprehensive rehabilitation, athletes can continue pursuing their passions with confidence and resilience, maximizing their potential and enjoyment in sports and physical endeavors.
Multiple Sclerosis (MS) is a complex neurological condition that affects millions of people worldwide. Beyond the physical symptoms, MS can have profound impacts on various aspects of life, including cognitive function, mental health, employment, relationships, and financial stability.
Understanding these challenges is essential for individuals living with MS, their caregivers, healthcare providers, and society as a whole. In this blog, we will delve into the various dimensions of living with MS, exploring its emotional toll, social dynamics, physical limitations, cognitive changes, and the crucial role of advocacy in raising awareness and promoting research for better treatments. Let's now look at the impact of multiple sclerosis.
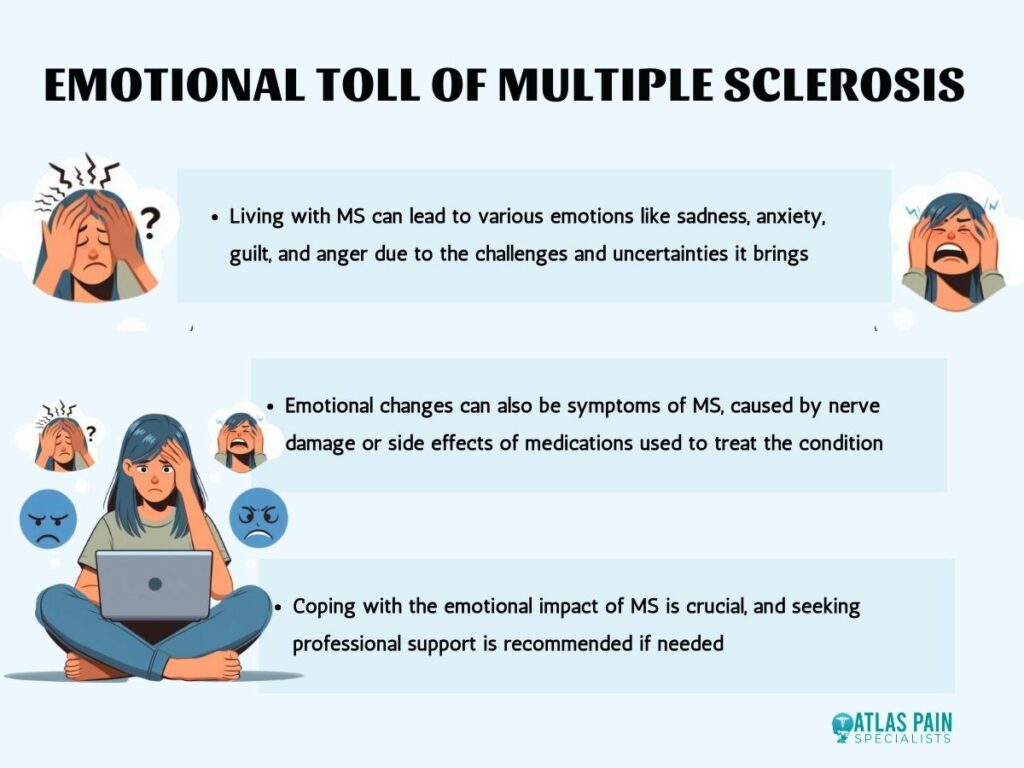
Emotional Toll of Multiple Sclerosis
Living with MS can bring about a rollercoaster of emotions. Anxiety and depression are common companions for many individuals grappling with this condition. The uncertainty of the disease progression, unpredictable symptoms, and the potential for disability can fuel anxiety.
Depression may stem from the challenges of adjusting to life with a chronic illness, as well as the physical limitations and changes in lifestyle.
Coping mechanisms become essential tools for navigating the emotional landscape of MS. Engaging in activities that bring joy and fulfillment, such as hobbies, creative outlets, or spending time with loved ones, can provide moments of respite from the challenges.
Seeking support from mental health professionals, support groups, or online communities can offer validation, understanding, and coping strategies tailored to the unique experiences of living with MS.
Social Impact and Relationships
MS doesn't just affect the individual diagnosed; it reverberates through their social circles, influencing relationships with family, friends, and colleagues.
Family Dynamics
MS can strain family dynamics as roles may shift due to the changing needs of the individual with MS. Family members may grapple with feelings of helplessness or guilt, while the person with MS may struggle with feelings of dependence or inadequacy.
Open communication, mutual support, and adaptability are vital for maintaining healthy familial relationships amidst the challenges of MS.
Friendships
Friendships may evolve as the dynamics of social interactions change. Some friends may step up to provide unwavering support, while others may struggle to understand or cope with the realities of MS.
It's common for individuals with MS to experience feelings of isolation or abandonment as friendships shift. Honest communication about needs and boundaries can help foster understanding and maintain meaningful connections.
Workplace Relationships
MS can also impact relationships in the workplace. Colleagues may struggle to comprehend the fluctuating nature of MS symptoms, leading to misconceptions or stigmatization.
Individuals with MS may face challenges in disclosing their condition due to fears of discrimination or lack of understanding. Open dialogue and workplace accommodations can facilitate a supportive environment where individuals with MS can thrive professionally.
Employment and Financial Challenges
MS can significantly impact employment opportunities and financial stability due to its unpredictable nature and the potential for physical and cognitive limitations.
Career Choices
Individuals with MS may face difficult decisions regarding their careers. The fluctuating nature of MS symptoms can make it challenging to maintain consistent employment, leading some to reconsider their career paths or make adjustments to accommodate their health needs.
This may involve transitioning to less physically demanding roles, seeking flexible work arrangements, or exploring alternative career options that align with their abilities and limitations.
Employment Opportunities
Discrimination and stigma surrounding disabilities, including MS, can pose barriers to securing and maintaining employment. Some employers may be unwilling or unable to provide necessary accommodations, leading to challenges in finding suitable work environments.
Individuals with MS may experience gaps in their employment history due to periods of illness or disability, which can further hinder their job prospects.
Financial Stability
The impact of MS on employment can have ripple effects on financial stability. Reduced earning potential, increased medical expenses, and potential reliance on disability benefits can strain financial resources.
Managing finances becomes crucial for individuals with MS and their families, necessitating careful budgeting, financial planning, and exploring resources for assistance.
Physical Limitations and Lifestyle Adjustments
MS can impose various physical limitations that require individuals to make significant lifestyle adjustments to manage their symptoms and maintain their well-being.

- Mobility Issues: Issues such as muscle weakness, balance problems, and coordination issues can affect mobility, making tasks like walking, climbing stairs, or driving more challenging. Mobility aids such as canes, walkers, or wheelchairs may be necessary to navigate daily life effectively.
- Fatigue: Unlike ordinary tiredness, MS-related fatigue may not improve with rest and can occur suddenly or persistently. Managing fatigue often involves balancing activities, prioritizing tasks, pacing oneself, and incorporating rest breaks into daily routines.
- Pain: Chronic pain is another common symptom of MS, affecting various parts of the body, such as the back, limbs, or face. Pain management strategies may include medications, physical therapy, relaxation techniques, or alternative therapies to alleviate discomfort and improve overall well-being.
- Lifestyle Adjustments: Living with MS often requires individuals to adapt their lifestyles to accommodate their changing needs and abilities. This may involve making modifications to the home environment to enhance accessibility and safety, seeking assistance with daily tasks, and prioritizing self-care activities such as exercise, nutrition, and stress management.
Cognitive Function and Mental Health
Living with Multiple Sclerosis (MS) not only affects physical health but also cognitive function and mental health. Understanding the cognitive changes, memory issues, and the importance of advocacy is crucial for individuals with MS and their support networks.
Cognitive Function and Memory Issues
MS can impact cognitive function, leading to difficulties with memory, concentration, information processing, and problem-solving.
- Memory Issues: Many individuals with MS experience memory difficulties, such as short-term memory loss or problems with retrieving information. These memory issues can affect daily tasks, work performance, and interpersonal relationships. Strategies such as using calendars, reminders, and organization techniques can help mitigate memory challenges and improve daily functioning.
- Attention and Concentration: MS can also affect attention and concentration, making it challenging to stay focused on tasks or conversations. Individuals may find themselves easily distracted or struggling to maintain attention for prolonged periods. Breaking tasks into smaller, manageable steps and minimizing distractions can support attention and concentration.
- Information Processing: Processing information may become slower or less efficient in individuals with MS. This can manifest as delays in understanding and responding to verbal or written communication. Strategies such as taking breaks, using visual aids, and practicing mindfulness techniques can aid in processing information more effectively.
- Problem-Solving Skills: MS can impact problem-solving abilities, making it harder to navigate complex situations or make decisions. Individuals may find it helpful to break problems down into smaller components, seek input from others, and utilize problem-solving techniques such as brainstorming or decision-making frameworks.
Mental Health
Mental health is a critical aspect of living with MS, as individuals may experience a range of emotional challenges, including depression, anxiety, and adjustment disorders.
Depression
Depression is common among individuals with MS and can stem from factors such as the impact of the disease on daily life, changes in roles and relationships, and neurological changes affecting mood regulation.
Symptoms of depression may include persistent sadness, loss of interest in activities, changes in appetite or sleep, and feelings of hopelessness. Seeking support from mental health professionals and engaging in therapy or support groups can help manage depression symptoms.
Anxiety
Anxiety is another prevalent mental health issue in individuals with MS, often fueled by uncertainty about the future, fear of symptom progression, and worries about managing daily challenges.
Symptoms of anxiety may include excessive worry, restlessness, irritability, and physical symptoms such as palpitations or muscle tension. Learning relaxation techniques, practicing mindfulness, and seeking therapy can assist in managing anxiety symptoms.
Advocacy and Community Engagement
Advocacy plays a vital role in raising awareness about MS, promoting research for better treatments, and advocating for the needs of individuals affected by the disease.
- Raising Awareness: Advocacy efforts aim to increase understanding of MS among the general public, healthcare professionals, policymakers, and the media. By raising awareness about the impact of MS on cognitive function, mental health, and overall well-being, advocates can reduce stigma, foster empathy, and promote inclusivity.
- Promoting Research: Advocacy efforts also advocate for increased funding and support for MS research, including studies focused on cognitive function, mental health interventions, and symptom management. By advocating for research initiatives, individuals and organizations can contribute to the development of more effective treatments, improved quality of life, and ultimately, a cure for MS.
- Community Engagement: Engaging with the MS community through support groups, online forums, and advocacy organizations provides a sense of belonging, validation, and mutual support. By connecting with others who understand their experiences, individuals with MS can access valuable resources, share coping strategies, and advocate for their needs collectively.
Conclusion
Living with Multiple Sclerosis presents a myriad of challenges that extend far beyond the realm of physical health. From navigating the emotional rollercoaster of anxiety and depression to managing the social dynamics of relationships and employment, individuals with MS face unique hurdles on a daily basis.
Coping with cognitive changes, memory issues, and mental health concerns adds further complexity to the MS journey. However, through advocacy, community support, and a deeper understanding of the multifaceted impacts of MS, we can strive to create a more inclusive and supportive environment for those affected by the condition.
By fostering empathy, raising awareness, and advocating for research, we can work towards a future where individuals with MS can lead fulfilling lives with dignity, resilience, and hope.
Fibromyalgia is a chronic disorder characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties. It affects millions of people worldwide, predominantly women, and can significantly impact their quality of life.
While there is no known cure for fibromyalgia, a multidisciplinary approach that integrates conventional medical treatments with complementary and alternative therapies offers a promising avenue for managing symptoms and improving overall well-being.
This article explores various integrative approaches to fibromyalgia pain management, highlighting their benefits and potential effectiveness.
Understanding Fibromyalgia
Before delving into integrative approaches to fibromyalgia pain management, it's crucial to understand the condition itself. Fibromyalgia is characterized by widespread pain, typically accompanied by fatigue, sleep disturbances, cognitive difficulties, and mood disorders such as depression and anxiety.
While the exact cause of fibromyalgia remains unknown, it is believed to involve abnormalities in the way the brain and nervous system process pain signals. Factors such as genetics, physical trauma, infections, and psychological stress may contribute to the development of fibromyalgia. Despite ongoing research efforts, fibromyalgia remains a complex and challenging condition to diagnose and treat.
Conventional Treatments for Fibromyalgia
Fibromyalgia, a chronic condition characterized by widespread pain and various accompanying symptoms, is managed through several conventional treatment methods:

1. Medication
Pain management often involves prescription medications such as analgesics, antidepressants, and anti-seizure drugs to alleviate pain, improve sleep, and address mood disturbances.
2. Exercise
Incorporating regular, low-impact exercises like walking, swimming, or yoga can improve muscle strength, flexibility, and overall well-being while reducing pain levels.
3. Cognitive-Behavioral Therapy (CBT)
CBT helps individuals develop coping mechanisms, manage stress, and address negative thought patterns associated with fibromyalgia, leading to improved symptom management and overall quality of life.
4. Lifestyle Adjustments
Implementing lifestyle changes like stress reduction techniques, optimizing sleep hygiene, and maintaining a balanced diet can complement conventional treatments and alleviate fibromyalgia symptoms.
By combining these conventional approaches, individuals with fibromyalgia can effectively manage their condition and enhance their daily functioning and quality of life. Working closely with healthcare professionals to tailor treatment plans to individual needs is crucial for optimal outcomes.
Pain Management Strategies for Fibromyalgia Using Integrative Approaches
Integrative medicine takes a holistic approach to healthcare, emphasizing the integration of conventional and complementary therapies to address the physical, emotional, and spiritual aspects of health. Several complementary and alternative therapies have shown promise in managing fibromyalgia symptoms and improving overall well-being.
Here are some integrative approaches that individuals with fibromyalgia may consider incorporating into their treatment plans:
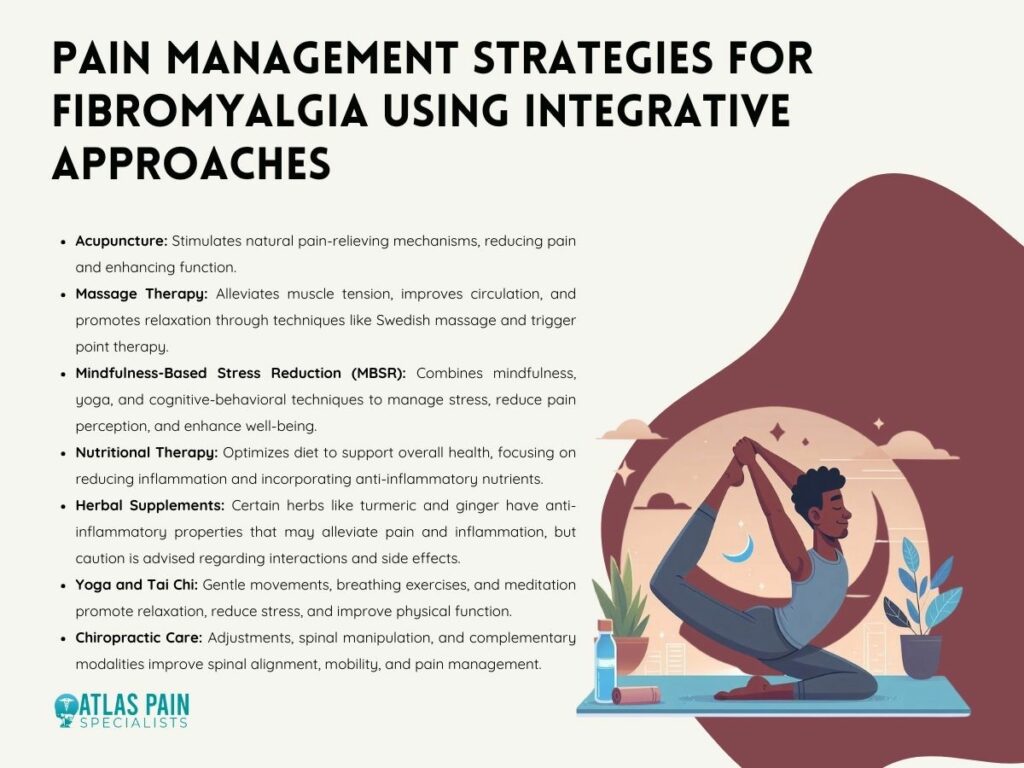
1. Acupuncture
Acupuncture, an ancient Chinese practice involving the insertion of thin needles into specific points on the body, has been shown to help reduce pain and improve function in individuals with fibromyalgia. It is believed to stimulate the body's natural pain-relieving mechanisms and promote relaxation.
2. Massage Therapy
Massage therapy can help alleviate muscle tension, improve circulation, and reduce pain in individuals with fibromyalgia. Techniques such as Swedish massage, myofascial release, and trigger point therapy may be particularly beneficial for targeting areas of discomfort and promoting relaxation.
3. Mindfulness-Based Stress Reduction (MBSR)
MBSR is a structured program that combines mindfulness meditation, yoga, and cognitive-behavioral techniques to help individuals manage stress, reduce pain perception, and improve overall well-being. Studies have shown that MBSR can be effective in reducing fibromyalgia symptoms and enhancing quality of life.
4. Nutritional Therapy
Nutritional therapy focuses on optimizing diet and nutritional status to support overall health and well-being. Some individuals with fibromyalgia may benefit from dietary modifications, such as reducing inflammatory foods and incorporating anti-inflammatory nutrients like omega-3 fatty acids and antioxidants.
5. Herbal Supplements
Certain herbal supplements, such as turmeric, ginger, and Boswellia, have anti-inflammatory and analgesic properties that may help reduce pain and inflammation in individuals with fibromyalgia. However, it's essential to consult with a qualified healthcare provider before using herbal supplements, as they may interact with medications or have side effects.
6. Yoga and Tai Chi
Yoga and tai chi are mind-body practices that combine gentle movements, breathing exercises, and meditation to promote relaxation, reduce stress, and improve physical function. Both yoga and tai chi have been shown to be beneficial for individuals with fibromyalgia, helping to reduce pain levels and improve overall quality of life.
7. Chiropractic Care
Chiropractic adjustments and spinal manipulation may help improve spinal alignment, reduce pain, and enhance mobility in individuals with fibromyalgia. Chiropractors may also incorporate other modalities such as massage therapy, stretching exercises, and lifestyle counseling to support holistic pain management.
Integrative approaches to fibromyalgia pain management offer a holistic and personalized approach to addressing the complex array of symptoms associated with this condition. It's essential for individuals with fibromyalgia to work closely with a healthcare provider who can tailor a treatment plan to meet their unique needs and preferences, integrating various therapies to achieve optimal symptom relief and functional improvement.
Benefits of Integrative Approaches to Fibromyalgia Pain Management
Managing fibromyalgia pain requires a multifaceted approach that addresses the physical, emotional, and psychological aspects of the condition. Integrative approaches to fibromyalgia pain management offer a range of benefits that encompass physical, emotional, and psychological well-being.
Here are some key advantages of integrating complementary and alternative therapies with conventional treatments:

1. Comprehensive Pain Relief
Integrative approaches employ various modalities such as acupuncture, massage therapy, and mind-body practices to target pain from multiple angles, leading to more effective pain relief compared to relying solely on conventional medications.
2. Reduced Side Effects
Conventional medications for fibromyalgia pain management may cause undesirable side effects. Integrative therapies, like acupuncture and herbal remedies, typically have fewer side effects, making them appealing options for those seeking alternatives with fewer adverse reactions.
3. Improved Physical Functioning
Integrative therapies such as exercise, chiropractic care, and physical therapy can enhance muscle strength, flexibility, and overall physical functioning. By addressing musculoskeletal issues and promoting mobility, these therapies improve daily activities and quality of life.
4. Enhanced Emotional Well-Being
Fibromyalgia often coexists with mood disorders. Mind-body practices like meditation and yoga can reduce stress, improve mood, and foster emotional well-being, providing relief from emotional symptoms.
5. Personalized Treatment Plans
Integrative medicine emphasizes individualized care, allowing healthcare providers to tailor treatment plans to each patient's unique needs and preferences. This approach ensures that patients receive the most appropriate and effective interventions.
6. Empowerment and Self-Management
Integrative approaches empower individuals to take an active role in managing their condition through self-care practices such as dietary changes and stress management techniques. This fosters greater control over symptoms and overall health outcomes.
7. Sustainability
Integrative therapies focus on promoting overall health and wellness, not just symptom management. By addressing underlying imbalances and promoting lifestyle changes, these approaches provide sustainable, long-term relief from fibromyalgia symptoms.
8. Enhanced Quality of Life
The ultimate goal of integrative fibromyalgia pain management is to improve overall quality of life. By addressing physical discomfort, emotional distress, and functional limitations, integrative approaches help patients lead more fulfilling, active, and enjoyable lives despite their chronic pain.
Integrative approaches offer a holistic and patient-centered approach to fibromyalgia pain management, addressing the complex interplay of physical, emotional, and psychological factors associated with the condition.
By combining conventional treatments with complementary and alternative therapies, individuals with fibromyalgia can experience comprehensive pain relief, improved functioning, and enhanced overall well-being.
Additional Considerations
Integrative approaches to fibromyalgia pain management encompass a broad spectrum of strategies beyond those discussed. Here are some additional considerations:
1. Patient Education and Empowerment
Integrative medicine places significant emphasis on educating patients about their condition and empowering them to actively participate in their care. By understanding the underlying mechanisms of fibromyalgia and learning self-management techniques, patients can take control of their symptoms and make informed decisions about their health.
2. Supportive Therapies
Integrative approaches may incorporate supportive therapies such as heat therapy, hydrotherapy, or transcutaneous electrical nerve stimulation (TENS). These modalities can help alleviate pain, reduce muscle tension, and improve circulation, providing additional relief for individuals with fibromyalgia.
3. Biofeedback and Neurofeedback
Biofeedback and neurofeedback techniques enable individuals to learn how to control physiological processes such as heart rate, muscle tension, and brainwave activity. By harnessing the mind-body connection, these therapies can help individuals manage pain and stress more effectively.
4. Environmental Modifications
Integrative medicine considers the impact of the environment on health and well-being. Simple modifications to the home or work environment, such as ergonomic adjustments or noise reduction measures, can help minimize triggers and improve comfort for individuals with fibromyalgia.
5. Peer Support and Group Therapy
Connecting with others who share similar experiences can provide valuable emotional support and validation for individuals with fibromyalgia. Group therapy sessions or peer support groups facilitated by healthcare professionals can offer a sense of community and camaraderie, reducing feelings of isolation and enhancing coping mechanisms.
6. Spiritual and Mindfulness Practices
For some individuals, incorporating spiritual or mindfulness practices into their daily routine can provide a sense of purpose, meaning, and connection. Activities such as prayer, meditation, or spending time in nature may complement other treatment modalities and contribute to overall well-being.
7. Continued Research and Innovation
Integrative medicine is a dynamic field that continues to evolve with ongoing research and innovation. As scientists uncover new insights into the mechanisms of fibromyalgia and explore novel treatment modalities, integrative approaches will continue to adapt and expand, offering new avenues for relief and healing.
By incorporating these additional considerations into fibromyalgia management plans, healthcare providers and individuals with fibromyalgia can explore a broader range of treatment options and tailor interventions to meet individual needs.
Integrative approaches aim to address the complexity of fibromyalgia by considering the interconnectedness of physical, emotional, and environmental factors, ultimately promoting holistic healing and improved quality of life.
Conclusion
In the landscape of fibromyalgia management, the integration of diverse treatment modalities emerges as a transformative approach. By recognizing the multifaceted nature of this condition, integrative methodologies offer a nuanced and comprehensive framework for addressing its myriad challenges.
Through the fusion of conventional interventions like medication and therapy with complementary practices such as acupuncture and massage therapy, integrative approaches provide a rich tapestry of care. This multifaceted strategy not only targets the physical symptoms of fibromyalgia but also attends to the emotional and psychological dimensions of pain and distress.
Moreover, integrative approaches offer more than just symptom management; they cultivate resilience and promote holistic well-being. As research continues to evolve and practitioners explore new avenues of treatment, integrative medicine remains a beacon of hope for individuals navigating the complex terrain of fibromyalgia. Its holistic ethos and patient-centered care approach ensure that individuals receive comprehensive support as they embark on their path to healing and wellness.
Have you ever felt like your mind and body are tangled in a mysterious dance of discomfort and distress? It's a journey many people silently navigate every day, yet its significance often remains overlooked or underestimated.
Today, we're delving into the intricate relationship between mental health and chronic pain. It's a link that's not always apparent at first glance, but once understood, it sheds light on the complexities of human experience and opens doors to holistic approaches in healthcare.
The Impact of Chronic Pain on Mental Health
Chronic pain, characterized by persistent discomfort lasting for more than three months, not only affects physical well-being but also takes a toll on mental health. The relentless presence of pain can lead to various psychological challenges, exacerbating existing conditions or even giving rise to new ones.
Understanding the profound impact of chronic pain on mental health is crucial for effective management and holistic care. Here are some key ways chronic pain affects mental well-being:

- Increased Stress Levels: Chronic pain triggers a heightened stress response in the body, leading to increased levels of cortisol, the stress hormone. This ongoing stress contributes to a vicious cycle, exacerbating both physical pain and mental distress.
- Depression and Anxiety Disorders: Living with chronic pain significantly increases the risk of developing depression and anxiety disorders. The relentless nature of pain, coupled with limitations in daily activities, social isolation, and fear of the future, can erode mental resilience and lead to profound feelings of sadness and apprehension.
- Substance Use Disorders: Individuals experiencing chronic pain may turn to substances like alcohol or opioids in an attempt to alleviate their symptoms or cope with the emotional distress caused by pain. However, reliance on such substances can quickly spiral into addiction, further complicating both the pain management process and mental health.
- Sleep Disturbances and Fatigue: Persistent pain often disrupts sleep patterns, leading to insomnia or fragmented sleep. Sleep disturbances not only exacerbate physical discomfort but also contribute to mental fatigue, irritability, and impaired cognitive function, perpetuating the cycle of pain and mental distress.
- Difficulty Concentrating and Decreased Appetite: The cognitive impact of chronic pain can manifest as difficulty concentrating, memory problems, and decreased mental clarity. Additionally, the emotional toll of pain may result in a loss of interest in food or decreased appetite, further compromising nutritional intake and overall well-being.
- Mood Changes and Frustration: Living with chronic pain can lead to frequent mood swings, irritability, and feelings of frustration or hopelessness. The inability to engage in activities once enjoyed, and the constant struggle to manage pain can erode emotional resilience and exacerbate feelings of helplessness.
Managing the Impact: Strategies and Support
Acknowledging the profound interplay between chronic pain and mental health is the first step towards effective management and support. Integrated approaches that address both physical and psychological aspects of pain management are essential. These may include:
- Multidisciplinary Treatment Plans: Collaborative efforts involving healthcare professionals from various disciplines, including pain specialists, psychologists, and physical therapists, can provide comprehensive care tailored to individual needs.
- Cognitive Behavioral Therapy (CBT): CBT techniques help individuals develop coping strategies, challenge negative thought patterns, and improve emotional regulation, enhancing resilience in the face of chronic pain.
- Support Groups and Peer Counseling: Connecting with others facing similar challenges can provide invaluable support, validation, and coping strategies.
- Medication Management: Judicious use of medications, including pain relievers, antidepressants, and anti-anxiety medications, under the guidance of healthcare professionals can help alleviate symptoms and improve overall well-being.
- Lifestyle Modifications: Incorporating stress-reduction techniques, regular exercise, adequate sleep hygiene, and healthy dietary habits can complement medical interventions and promote holistic well-being.
Prevalence of Mental Health Conditions in Those with Chronic Pain
Chronic pain affects millions of people worldwide, significantly impacting not only physical health but also mental well-being. The co-occurrence of mental health conditions in individuals with chronic pain is a well-documented phenomenon, shedding light on the complex interplay between physical and psychological factors.
Understanding the prevalence of these mental health conditions is crucial for providing comprehensive care and support to those living with chronic pain. Here's an overview of the prevalence of mental health conditions in individuals with chronic pain:
Depression and Anxiety in People with Chronic Pain
Depression and anxiety are among the most prevalent mental health conditions experienced by individuals with chronic pain.
Research suggests that the prevalence of depression and anxiety disorders is substantially higher in individuals with chronic pain compared to the general population. For example, a study by the University of Arizona Health Sciences found that nearly 1 in 20 adults in the United States experience the co-occurrence of chronic pain and anxiety or depression, affecting over 12 million adults.
The constant experience of pain, coupled with functional limitations and social isolation, can contribute to the development or exacerbation of these mood disorders.
Impact of Chronic Pain on Quality of Life
Chronic pain exerts a profound impact on the overall quality of life for individuals affected by it. Beyond the physical discomfort, chronic pain can lead to diminished satisfaction with life, impaired social relationships, and compromised emotional well-being.
The persistent struggle to manage pain and engage in daily activities can erode one's sense of purpose and fulfillment, further exacerbating mental health challenges.
Specific Conditions and Their Association with Mental Health Issues
Certain chronic pain conditions are particularly associated with heightened mental health issues. For example, fibromyalgia, characterized by widespread musculoskeletal pain, is often accompanied by significant psychological distress, including depression, anxiety, and decreased quality of life.
Similarly, chronic low back pain and neuropathic pain syndromes have been linked to an increased prevalence of mental health conditions, highlighting the importance of addressing both physical and psychological aspects of pain management.
Table: Prevalence of Mental Health Conditions in Chronic Pain
| Mental Health Condition | Prevalence in Chronic Pain Patients |
| Depression | Higher prevalence compared to the general population |
| Anxiety | Elevated rates, often co-occurring with depression |
| Decreased Quality of Life | Universally reported across various chronic pain conditions |
Treatment and Therapies for Chronic Pain and Mental Health
Effective management of chronic pain requires a comprehensive approach that addresses both physical discomfort and associated mental health challenges. Integrating treatments and therapies targeting mental well-being alongside traditional pain management strategies can significantly improve outcomes and enhance the overall quality of life for individuals living with chronic pain. Here are key treatment modalities for chronic pain and mental health:
A. Antidepressant Medications
Antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs), are commonly prescribed to individuals with chronic pain, particularly those experiencing co-occurring depression or anxiety.
These medications not only alleviate mood symptoms but also have analgesic properties, helping to reduce pain intensity and improve overall functioning.
B. Talk Therapy (Psychotherapy)
Talk therapy, also known as psychotherapy, is a valuable treatment modality for addressing both chronic pain and mental health issues. Cognitive-behavioral therapy (CBT) is particularly effective in helping individuals develop coping strategies, challenge negative thought patterns, and improve pain management skills.
Through regular sessions with a trained therapist, individuals can gain insight into the interplay between their thoughts, emotions, and pain experiences, leading to enhanced resilience and improved overall well-being.
C. Stress-Reduction Techniques, Physical Activity, Exercise, Meditation, Journaling, and Coping Skills
Incorporating stress-reduction techniques, physical activity, exercise, meditation, journaling, and coping skills into daily life can significantly improve both physical and mental well-being for individuals with chronic pain. These self-care practices promote relaxation, improve mood, and enhance overall quality of life.
Engaging in regular physical activity and exercise not only helps to strengthen muscles and improve flexibility but also releases endorphins, natural pain-relieving chemicals in the brain, leading to reduced pain perception and improved mood.
Similarly, mindfulness-based practices such as meditation and journaling can help individuals cultivate greater awareness of their thoughts and emotions, leading to reduced stress and enhanced emotional regulation.
D. Pain Rehabilitation Programs
Pain rehabilitation programs offer comprehensive, interdisciplinary approaches to chronic pain management, addressing both physical and psychological aspects of the condition. These programs typically involve a combination of medical interventions, physical therapy, occupational therapy, and psychological support. Through structured, goal-oriented interventions, individuals participating in pain rehabilitation programs learn to improve functional abilities, develop effective coping strategies, and optimize overall quality of life.
E. Importance of Mental Health Screening in Chronic Pain Treatment
Routine mental health screening is essential in the management of chronic pain to identify and address underlying psychological issues effectively. Early detection and intervention for depression, anxiety, and other mental health conditions can significantly improve treatment outcomes and promote holistic well-being.
By incorporating mental health screening into routine clinical assessments, healthcare providers can better understand the individual needs of patients with chronic pain and tailor treatment plans accordingly.
Table: Treatment and Therapies for Chronic Pain and Mental Health
| Treatment/Therapy | Description |
| Antidepressant Medications | SSRIs and TCAs alleviate mood symptoms and have analgesic properties, reducing pain intensity and improving functioning. |
| Talk Therapy (Psychotherapy) | CBT helps individuals develop coping strategies, challenge negative thought patterns, and improve pain management skills. |
| Stress-Reduction Techniques | Techniques such as meditation, exercise, and journaling promote relaxation, improve mood, and enhance overall well-being. |
| Pain Rehabilitation Programs | Interdisciplinary programs combine medical interventions, physical therapy, occupational therapy, and psychological support. |
| Mental Health Screening | Routine screening identifies underlying psychological issues, enabling early intervention and improved treatment outcomes. |
Integrated Solutions for Chronic Pain and Mental Health
Addressing the complex interplay between chronic pain and mental health requires integrated solutions that recognize the multifaceted nature of these conditions. Drawing insights from global mental health, transdiagnostic approaches, cultural idioms of distress, and person-centered care can enhance chronic pain management and promote holistic well-being. Here are key components of integrated solutions for chronic pain and mental health:
A. Lessons from Global Mental Health for Chronic Pain Management
Global mental health initiatives offer valuable lessons for chronic pain management, emphasizing the importance of contextually relevant, community-based interventions. Collaborative models involving healthcare providers, community leaders, and individuals affected by chronic pain can help identify culturally sensitive approaches to pain management and mental health support.
By leveraging existing infrastructure and resources, global mental health frameworks provide insights into enhancing access to care and reducing disparities in chronic pain management.
B. Transdiagnostic Approaches and Social Determinants
Transdiagnostic approaches recognize common underlying mechanisms across various mental health conditions and chronic pain, emphasizing shared vulnerability factors and treatment strategies.
Addressing social determinants of health, such as socioeconomic status, access to healthcare, and environmental factors, is crucial for improving outcomes in chronic pain and mental health. By adopting transdiagnostic frameworks and addressing social determinants, healthcare providers can better tailor interventions to individual needs and promote equitable care.
C. Cultural Idioms of Distress and Traditional Healing Practices
Acknowledging cultural idioms of distress and traditional healing practices is essential for providing culturally competent care to individuals with chronic pain and mental health concerns. Cultural beliefs and practices surrounding pain and illness influence help-seeking behaviors and treatment preferences.
Integrating traditional healing modalities, such as acupuncture, herbal medicine, and spiritual rituals, alongside evidence-based treatments can enhance treatment engagement and effectiveness. By fostering trust and collaboration, healthcare providers can honor diverse cultural perspectives and promote healing within communities.
D. Person-Centered Care and Shared Decision-Making
Person-centered care emphasizes collaboration between healthcare providers and individuals with chronic pain, prioritizing individual preferences, values, and goals. Shared decision-making empowers individuals to actively participate in treatment decisions, leading to greater satisfaction and improved outcomes.
By fostering open communication, mutual respect, and trust, healthcare providers can co-create personalized care plans that address both physical and psychological aspects of chronic pain. Person-centered approaches promote autonomy, dignity, and empowerment, fostering resilience and promoting recovery.
Conclusion
Understanding the deep connection between chronic pain and mental health unveils a pathway to holistic care. By recognizing how pain affects emotions and vice versa, we pave the way for integrated treatments that address both physical discomfort and psychological distress. With collaborative efforts and personalized approaches, we can improve the well-being of individuals living with chronic pain, enhancing their quality of life and promoting resilience.
A small but considerable segment of the population suffers from the confusing and sometimes misdiagnosed chronic pain disease known as Complex Regional Pain Syndrome (CRPS). It typically manifests as severe, prolonged pain in one or more limbs, accompanied by sensory, motor, and autonomic abnormalities.
Despite its relatively low prevalence, CRPS can have profound and far-reaching effects on the physical, emotional, and social well-being of those afflicted, often leading to disability, reduced quality of life, and significant healthcare costs. Understanding CRPS is essential for healthcare professionals, patients, caregivers, and the broader community.
The condition's complex nature, varied presentations, and lack of definitive diagnostic tests pose challenges to accurate diagnosis and effective management. Moreover, the unpredictable course of CRPS and its potential to worsen over time underscore the need for comprehensive, multidisciplinary approaches to treatment and care.
What is CRPS?
Complex Regional Pain Syndrome (CRPS) is a multifaceted chronic pain condition that presents with a wide array of symptoms, often affecting one or more extremities. This condition is characterized by disproportionate and continuous pain that is typically more severe than expected based on the initial injury or inciting event.
CRPS is often divided into two subtypes, each with its own distinct characteristics and diagnostic criteria, which we will explore in detail.
1. CRPS Type I (formerly known as Reflex Sympathetic Dystrophy, RSD)
CRPS Type I is the most common form of the condition, accounting for approximately 90% of cases. It typically occurs following an injury or trauma, such as a fracture, sprain, or surgical procedure, although the severity of the initial injury may not correlate with the intensity of the subsequent pain.
This subtype of CRPS is characterized by the absence of detectable nerve damage or injury on diagnostic tests, making its diagnosis primarily based on clinical findings. Despite the lack of identifiable nerve damage, CRPS Type I is associated with dysregulation of the ANS (autonomic nervous system), leading to symptoms such as changes in skin color, temperature, texture, and abnormal sweating and swelling.
Additionally, individuals with CRPS Type I may experience sensory disturbances, including hyperalgesia (increased sensitivity to pain), allodynia (pain in response to non-painful stimuli), motor dysfunction, and muscle weakness in the affected limb.
2. CRPS Type II (formerly known as causalgia)
CRPS Type II, also referred to as causalgia, differs from Type I in that it is characterized by identifiable nerve damage or injury. This subtype typically occurs following a nerve injury, such as laceration, crush injury, or nerve entrapment, and is often associated with more severe and persistent pain compared to Type I.
Despite the presence of nerve damage, the pain experienced in CRPS Type II may still be disproportionate to the extent of the initial injury. In addition to the hallmark features of CRPS, individuals with Type II may exhibit signs of nerve injury, such as sensory loss, weakness, and abnormal nerve conduction studies.
The presence of demonstrable nerve damage in CRPS Type II underscores the involvement of both peripheral and central nervous system mechanisms in the pathophysiology of the condition.
Who Does CRPS Affect?
Complex Regional Pain Syndrome (CRPS) can affect individuals of any age, gender, or ethnicity, although certain demographic and clinical factors may influence the likelihood of developing the condition.
A risk factor is an attribute or pattern of behavior that is more common in people with an illness or in people who are more likely to have a disease than in those without risk factor. A person does not automatically develop a condition because they do not have a risk factor, and vice versa.
1. Demographics of CRPS
CRPS affects both genders, although it is more commonly observed in females than males, with some studies suggesting a female-to-male ratio of approximately 3:1. The condition can occur at any age. Still, it is most frequently diagnosed in individuals between 20 and 55.
However, CRPS can also affect children and adolescents, albeit less frequently, presenting unique challenges in diagnosis and management in pediatric populations.
2. Prevalence and Incidence
The exact prevalence and incidence of CRPS are difficult to ascertain due to variations in diagnostic criteria, healthcare utilization patterns, and underreporting of cases. However, estimates suggest that CRPS affects anywhere from 5 to 26 individuals per 100,000 person-years, with higher rates reported in certain populations, such as those with prior trauma or surgery.
Despite its relatively low prevalence, CRPS can have a significant socioeconomic burden, with implications for healthcare costs, disability, and loss of productivity.
3. Risk Factors for CRPS
Although the exact etiology of CRPS is still unknown, several risk factors have been found to raise the chance of developing the condition. Trauma or injury, such as fractures, sprains, or surgical procedures, is a well-established trigger for CRPS, particularly in cases of CRPS Type I.
Other predisposing factors include peripheral nerve injury, vascular disorders, and psychological stressors, although the exact mechanisms by which these factors contribute to the development of CRPS are not fully understood. Additionally, certain genetic predispositions and susceptibility factors may influence an individual's risk of developing CRPS, highlighting the complex interplay between genetic, environmental, and psychosocial factors in the pathogenesis of the condition.
Symptoms of CRPS
Complex Regional Pain Syndrome (CRPS) is characterized by a diverse array of symptoms that can vary in severity and presentation among affected individuals. The quality of life and outcomes for patients with this difficult chronic pain syndrome can be enhanced by healthcare teams by treating the complex and complex nature of CRPS symptoms with a thorough and multidisciplinary approach.
It is important to note that the symptoms of CRPS can vary widely among individuals and may change over time. Some individuals may experience fluctuations in symptom severity, while others may develop progressive worsening of symptoms. Additionally, the presentation of CRPS may differ depending on the subtype (Type I or Type II) and other factors such as age, comorbidities, and response to treatment.

1. Chronic Pain
Chronic, persistent pain is the hallmark symptom of CRPS, often described as burning, throbbing, or shooting in nature. The pain is typically localized to the affected limb but may spread to adjacent areas over time.
Individuals with CRPS often report that the pain is disproportionate to the inciting event or injury and may worsen with movement or touch.
2. Sensory Disturbances
CRPS can cause a range of sensory abnormalities, including hyperalgesia, which is an increased sensitivity to painful stimuli, and allodynia, which is a pain in response to normally non-painful stimuli, such as light touch or gentle pressure.
Other sensory disturbances may include tingling, numbness, or a feeling of pins and needles in the affected limb.
3. Motor Dysfunction
Motor dysfunction is common in CRPS and may manifest as weakness, tremors, or involuntary muscle contractions (dystonia). Individuals with CRPS may experience difficulty moving the affected limb, as well as limitations in coordination and fine motor skills.
Muscle atrophy and weakness may occur due to disuse or immobilization of the limb secondary to pain. Simple tasks such as dressing, grooming, and household chores may become challenging or impossible, leading to dependency on caregivers and reduced independence.
4. Autonomic Symptoms
Dysregulation of the autonomic nervous system is a hallmark feature of CRPS and can manifest in various ways. Changes in skin temperature, color, and texture are commonly observed, with the affected limb appearing either warmer or cooler than the unaffected limb.
Additionally, individuals with CRPS may experience abnormal sweating (either excessive sweating or absence of sweating) and swelling (edema) in the affected limb.x
Causes and Triggers of CRPS
Complex Regional Pain Syndrome (CRPS) can be triggered by a variety of factors, ranging from traumatic injuries to medical procedures. It is important to recognize that not all individuals who experience trauma or injury will develop CRPS, highlighting the role of individual susceptibility factors in the pathogenesis of the condition.
1. Traumatic Injuries
Trauma or injury is one of the most common triggers for CRPS, particularly in cases of CRPS Type I. Fractures, sprains, contusions, and surgical procedures can all precipitate the onset of CRPS, although the severity of the initial injury may not always correlate with the subsequent development or severity of symptoms.
The exact mechanisms by which trauma leads to CRPS are not fully understood but may involve neurogenic inflammation, peripheral sensitization, and dysregulation of the sympathetic nervous system.
2. Surgical Procedures
Surgeries, particularly those involving orthopedic or peripheral nerve procedures, carry a risk of triggering CRPS, either as a complication of the surgery itself or as a result of postoperative pain and inflammation.
CRPS can develop following relatively minor surgical interventions, such as carpal tunnel release or arthroscopic procedures, highlighting the importance of vigilant monitoring and early intervention in high-risk individuals.
3. Peripheral Nerve Injury
Injuries to peripheral nerves, either from trauma or compression, can predispose individuals to developing CRPS, particularly in cases of CRPS Type II. Nerve injuries disrupt normal nerve signaling and can lead to aberrant pain processing, sensory disturbances, and motor dysfunction characteristic of CRPS.
Identifying and addressing nerve injuries promptly through surgical decompression or neurolysis may help prevent or mitigate the development of CRPS in susceptible individuals.
4. Vascular Disorders
Vascular abnormalities, such as vasospasm, ischemia-reperfusion injury, and endothelial dysfunction, have been implicated as potential triggers for CRPS. Changes in blood flow and microcirculation observed in CRPS may result from sympathetic nervous system dysregulation, leading to tissue hypoxia, inflammation, and neuropathic pain.
Individuals with pre-existing vascular conditions, such as Raynaud's phenomenon or peripheral vascular disease, may be at increased risk for developing CRPS following vascular insults or procedures.
Diagnosis and Treatment
Accurate diagnosis and effective treatment of Complex Regional Pain Syndrome (CRPS) require a multidisciplinary approach that addresses the complex interplay of neurologic, inflammatory, and psychosocial factors underlying the condition. Timely recognition of CRPS and prompt initiation of appropriate interventions are essential for improving outcomes and quality of life for affected individuals.
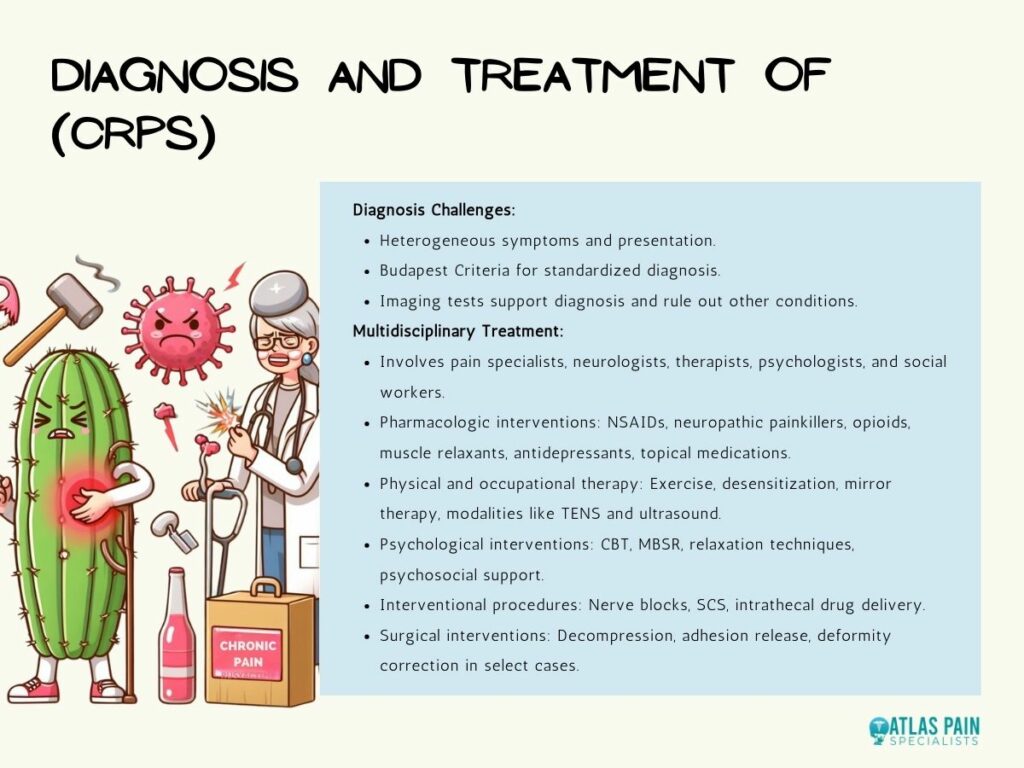
1. Challenges in Diagnosis
Diagnosing CRPS can be challenging due to the heterogeneity of symptoms, variability in presentation, and lack of definitive diagnostic tests. The Budapest Criteria, established by the International Association for the Study of Pain (IASP), provides a standardized framework for diagnosing CRPS based on clinical signs and symptoms, including pain, sensory disturbances, motor dysfunction, and autonomic changes.
Although results from imaging tests, such as MRIs, bone scans, and X-rays, are frequently nonspecific, they can be used to support the diagnosis of CRPS and rule out other illnesses.
2. Multidisciplinary Treatment Approaches
The management of CRPS typically involves a multidisciplinary team of healthcare professionals, including pain specialists, neurologists, physical therapists, occupational therapists, psychologists, and social workers. Treatment approaches for CRPS are aimed at addressing pain, improving function, and enhancing quality of life through a combination of pharmacologic, physical, psychological, and interventional modalities.
- Pharmacologic Interventions: Pharmacologic therapies for CRPS aim to relieve pain, reduce inflammation, and improve function. Nonsteroidal anti-inflammatory drugs (NSAIDs), neuropathic painkillers (pregabalin, gabapentin, etc.), opioid analgesics, muscle relaxants, and antidepressants are among the most often utilized pharmaceuticals. Topical medications like capsaicin cream or lidocaine patches may also relieve regional pain.
- Physical and Occupational Therapy: Physical and occupational therapy play a critical role in managing CRPS by addressing motor dysfunction, restoring function, and promoting independence. Therapeutic interventions may include gentle exercise, stretching, desensitization techniques, mirror therapy, and graded motor imagery. Modalities such as transcutaneous electrical nerve stimulation (TENS), ultrasound, and hydrotherapy may also be used to alleviate pain and improve mobility.
- Psychological Interventions: Psychological interventions, such as cognitive-behavioral therapy (CBT), mindfulness-based stress reduction (MBSR), and relaxation techniques, can help individuals with CRPS cope with pain, manage stress, and improve psychological well-being. Psychosocial support, education, and counseling are essential components of comprehensive CRPS management and may address underlying emotional distress, maladaptive coping strategies, and social isolation.
- Interventional Procedures: Interventional procedures, such as nerve blocks, sympathetic ganglion blocks, intrathecal drug delivery, and spinal cord stimulation (SCS), may be considered for individuals with refractory CRPS who have not responded to conservative therapies. These minimally invasive procedures aim to modulate pain signals, interrupt sympathetic nervous system activity, and improve function.
- Surgical Interventions: In select cases of CRPS with significant nerve compression or structural abnormalities, surgical interventions may be considered to decompress nerves, release adhesions, or correct deformities. Surgical procedures should be approached cautiously and reserved for individuals who have failed conservative treatments and have identifiable anatomical lesions amenable to surgical correction.
New Treatment for CRPS
Ongoing research into the pathophysiology of CRPS and the development of novel treatment modalities hold promise for improving outcomes and expanding therapeutic options for affected individuals. Participating in clinical trials and staying informed about advances in CRPS research may offer new hope for individuals living with this challenging condition.
Read on on New Treatment for CPRS to find out more about emerging therapies. These include monoclonal antibodies targeting inflammatory cytokines, gene therapy, regenerative medicine approaches, and neuromodulation techniques, which are being investigated in preclinical and clinical studies.
A comprehensive and cooperative approach that tackles the wide range of symptoms and underlying mechanisms causing the condition is necessary for the comprehensive management of CRPS. Through the integration of customized care plans, evidence-based treatments, and continuous support, medical professionals can improve patient outcomes and quality of life for those with CRPS.
