The Role of Physical Therapy in Managing Chronic Pelvic Pain
Chronic pelvic pain (CPP) is a debilitating condition characterized by persistent discomfort in the pelvic region lasting for six months or longer. It affects individuals of all ages and genders, significantly impairing their quality of life and daily functioning.
The cause or origin of CPP is complex and multifaceted, often involving a combination of gynecological, gastrointestinal, urological, and musculoskeletal factors.
This article explores the multifaceted role of physical therapy in managing chronic pelvic pain, highlighting its effectiveness in reducing pain, improving function, and enhancing the overall well-being of individuals living with this challenging condition.
Understanding Chronic Pelvic Pain
Chronic pelvic pain encompasses a wide range of symptoms, including but not limited to deep pelvic pain, dyspareunia (painful intercourse), urinary urgency and frequency, bowel dysfunction, and musculoskeletal impairments. This heterogeneous nature makes CPP challenging to diagnose and treat effectively. Moreover, the complex interplay between various physiological systems in the pelvis necessitates a comprehensive approach to management.
Symptoms include pelvic, lower abdominal, or lower back pain and can impact daily activities like intercourse, urination, or bowel movements. Despite complexities in diagnosis, physical therapy has emerged as a crucial treatment approach, addressing musculoskeletal imbalances and pelvic floor dysfunction to alleviate pain and improve function.
The Multifaceted Role of Physical Therapy in Managing Chronic Pelvic Pain
Chronic pelvic pain (CPP) is a complex and challenging condition that significantly impacts the lives of millions of individuals worldwide. CPP can be caused by a myriad of factors.
In the multidisciplinary approach to managing CPP, physical therapy emerges as a cornerstone, offering a multifaceted array of interventions aimed at addressing the diverse underlying causes and symptoms associated with this condition.

Comprehensive Assessment
Physical therapists specializing in pelvic health conduct thorough assessments to identify the various factors contributing to a patient's CPP. These assessments typically include detailed evaluations of pelvic floor muscle function, musculoskeletal alignment, posture, movement patterns, and functional limitations.
By gaining a comprehensive understanding of the individual's condition, physical therapists can tailor treatment plans to target specific impairments and optimize outcomes.
Pelvic Floor Rehabilitation
Dysfunction of the pelvic floor muscles is a common contributor to CPP. Physical therapists trained in pelvic floor rehabilitation employ a variety of techniques to address muscular imbalances, hypertonicity, weakness, and coordination issues within the pelvic floor musculature.
Manual therapy techniques such as myofascial release, trigger point therapy, and joint mobilizations are utilized to alleviate muscle tension and improve tissue mobility. Additionally, therapeutic exercises targeting pelvic floor muscle strength, endurance, and coordination are prescribed to optimize function and reduce pain.
Musculoskeletal Rehabilitation
In addition to pelvic floor dysfunction, musculoskeletal factors often play a significant role in CPP. Poor posture, muscle imbalances, and biomechanical dysfunctions can contribute to pelvic pain and discomfort. Physical therapists utilize manual therapy techniques, therapeutic exercise programs, and ergonomic education to address these musculoskeletal issues.
By restoring optimal alignment, improving muscle strength and flexibility, and promoting proper movement patterns, physical therapy aims to reduce pain and improve overall function.
Education and Self-Management Strategies
Patient education is a fundamental component of physical therapy for CPP. Physical therapists provide patients with valuable information about pelvic anatomy, pain mechanisms, and strategies for symptom management. Patients learn techniques for relaxation, stress management, and self-care, empowering them to take an active role in their recovery process.
By promoting self-awareness and teaching self-management strategies, physical therapists help patients regain control over their symptoms and improve their quality of life.
Collaborative Care
Physical therapists work collaboratively with other healthcare professionals involved in the management of CPP, including physicians, psychologists, and pelvic health specialists. This multidisciplinary approach ensures that patients receive comprehensive care addressing all aspects of their condition.
By fostering open communication and coordination among team members, physical therapists optimize treatment outcomes and provide patients with holistic care that addresses their unique needs.
While medications and surgical interventions may be necessary in certain cases, physical therapy has emerged as a cornerstone in the comprehensive management of CPP.
Overall, physical therapy for CPP is tailored to the individual's specific needs and may involve a combination of these interventions to address the complex nature of the condition and improve overall pelvic health and function.
The Goals of Physical Therapy in Managing Chronic Pelvic Pain
Through targeted interventions and personalized care plans, physical therapists aim to achieve several key goals in addressing the multifaceted nature of CPP. Here are the primary goals of physical therapy in managing chronic pelvic pain:
- Pain Reduction
- Muscle Rehabilitation
- Postural Correction
- Biofeedback and Neuromuscular Reeducation
- Education and Lifestyle Modifications
- Collaboration with Other Healthcare Providers
Through individualized treatment plans, education, and collaboration with other healthcare providers, physical therapists empower patients to regain control over their pelvic health and enhance their overall quality of life.
As awareness of the role of physical therapy in managing chronic pelvic pain continues to grow, more individuals can access effective, evidence-based care to alleviate their symptoms and restore function.
Additional Tips on How to Effectively Manage Chronic Pelvic Pain
Managing chronic pelvic pain (CPP) effectively requires a multifaceted approach that addresses the diverse factors contributing to the condition. Here are some additional strategies for effectively managing chronic pelvic pain:
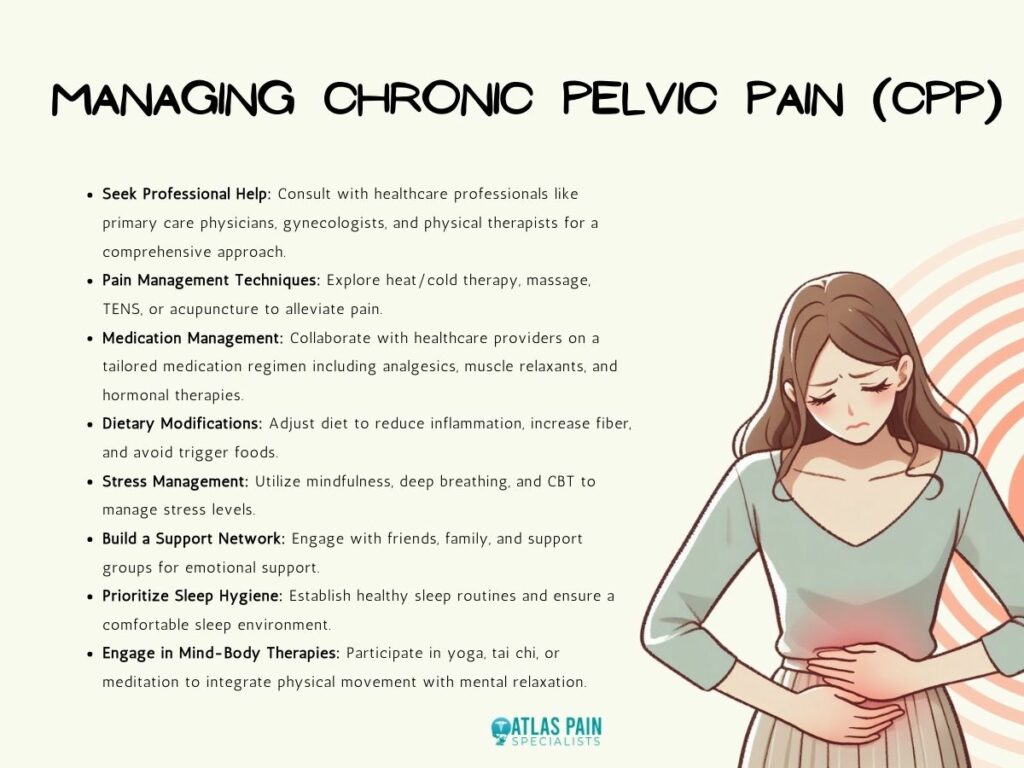
- Seek Professional Help
Consult with healthcare professionals, including primary care physicians, gynecologists, urologists, pain specialists, and physical therapists, for comprehensive evaluation and guidance tailored to your individual needs.
- Pain Management Techniques
Explore various pain management techniques such as heat/cold therapy, massage, transcutaneous electrical nerve stimulation (TENS), or acupuncture to help alleviate pain and promote relaxation.
- Medication Management
Work with your healthcare provider to develop a medication regimen tailored to your specific symptoms and underlying conditions contributing to chronic pelvic pain. This may include analgesics, muscle relaxants, hormonal therapies, or antidepressants to manage pain and associated symptoms.
- Dietary Modifications
Make dietary adjustments to support pelvic health and reduce inflammation, such as increasing fiber intake, staying hydrated, and avoiding trigger foods that may exacerbate symptoms.
- Stress Management
Practice stress-reduction techniques such as mindfulness, deep breathing exercises, progressive muscle relaxation, or cognitive-behavioral therapy (CBT) to reduce stress levels, which can contribute to pain perception and exacerbate symptoms of chronic pelvic pain.
- Build a Support Network
Surround yourself with a supportive network of friends, family, or support groups who can provide emotional support, understanding, and encouragement throughout your journey in managing chronic pelvic pain.
- Prioritize Sleep Hygiene
Establish healthy sleep habits and routines to ensure adequate rest and recovery, as poor sleep quality can exacerbate pain and impact overall well-being. Create a comfortable sleep environment, practice relaxation techniques before bedtime, and limit screen time and caffeine intake close to bedtime.
- Engage in Mind-Body Therapies
Explore mind-body therapies such as yoga, tai chi, meditation, or guided imagery, which integrate physical movements with mental focus and relaxation to reduce pain, improve coping mechanisms, and enhance overall well-being.
It's essential to remember that managing chronic pelvic pain may require patience, persistence, and a multidisciplinary approach involving various healthcare providers. By incorporating these strategies into your daily routine and working closely with your healthcare team, you can take steps toward effectively managing chronic pelvic pain and improving your quality of life.
Conclusion
Chronic pelvic pain is a challenging condition that can significantly impair an individual's physical, emotional, and social well-being. Physical therapy plays a pivotal role in the holistic management of CPP by addressing musculoskeletal dysfunction, promoting pain relief, and improving functional outcomes.
Through individualized treatment plans, education, and collaboration with other healthcare providers, physical therapists empower patients to regain control over their pelvic health and enhance their overall quality of life.
As awareness of the role of physical therapy in managing chronic pelvic pain continues to grow, more individuals can access effective, evidence-based care to alleviate their symptoms and restore function.
About Dr. Sean Ormond