The Role of Cognitive-Behavioral Therapy in Multidisciplinary Pain Management
Millions of individuals worldwide are impacted by the all-encompassing burden of chronic pain. Beyond only being uncomfortable physically, it affects all aspects of a person's life, including relationships, everyday activities, and mental and emotional health.
A comprehensive and multidisciplinary approach is frequently required to manage chronic pain effectively, and cognitive-behavioral therapy (CBT) is the cornerstone of this approach. The role of Cognitive-Behavioral Therapy in Multidisciplinary Pain Management is pivotal. Through the development of abilities to alter pain-related thoughts, feelings, and behaviors, cognitive behavioral therapy (CBT) plays an important part in pain management.
This article highlights the substantial impact of cognitive behavioral therapy (CBT) in multidisciplinary pain management, a therapeutic technique with several principles and practical applications. It seeks to provide people with the tools they need to take control of their pain and enhance their general quality of life.
Understanding Cognitive-Behavioral Therapy (CBT)
The psychotherapy approach of cognitive-behavioral therapy, or CBT, emphasizes the connection between thoughts, emotions, and behaviors. Since its development in the 1960s, cognitive behavioral therapy (CBT) has grown in popularity and is recognized for its effectiveness in treating various behavioral and mental health conditions.
Key Points:
- The foundation of CBT is the idea that our thoughts have an impact on our emotions and actions. Individuals can discover and alter faulty thought patterns to alter their emotional and behavioral reactions.
- It's a goal-oriented, brief therapy that works effectively for a variety of problems, such as anxiety, depression, and—most importantly—chronic pain.
Core Principles of CBT
When it comes to treating people with chronic pain disorders like headaches, fibromyalgia, arthritis, low back pain, orofacial pain, and even pain related to cancer treatment, CBT is currently the most widely used psychological intervention. Combining physical and psychological therapies seems to offer substantial benefits, even though there are instances where there are no known treatments for pain, as is the situation with chronic pain conditions.
When in pain, especially when moving, a person will usually opt to rest rather than conduct activities that aggravate their symptoms. However, resting does not help with symptoms because it could worsen them by generating secondary stiffness and weakness.
As other issues like financial difficulty and damaged relationships gradually seep in, the inability to function results in a loss of identity and self-esteem.
Instead of trying to uncover a biological cause for the presumed disease, CBT treatments enhance an individual's ability to control and cope with their pain. The foundation for CBT's success in assisting people in managing their chronic pain is a set of basic ideas that serve as its guidelines:
- Cognitive Restructuring: This is the process of identifying and challenging negative or irrational thoughts associated with pain. Patients can change their emotional responses by replacing these thoughts with more rational and constructive ones.
- Behavioral Activation: It encourages individuals to engage in positive and enjoyable activities, even in the presence of pain, to break the cycle of inactivity and isolation.
- Skills Development: Equipping patients with a toolbox of practical skills and strategies to manage pain, reduce distress, and enhance their quality of life.
Why Does CBT Stand Out?
Although CBT is often addressed by psychologists, other practitioners, including physiotherapists, occupational therapists, nurses, and physicians, must advance their psychological knowledge and expertise in order to support CBT. With a heavy focus on behavior, it uses visual feedback to explore various movement alternatives and help people restore their body schema and rediscover the fundamentals of relaxed, normal movement.
CBT stands out in the field of pain management because of its distinctive qualities:
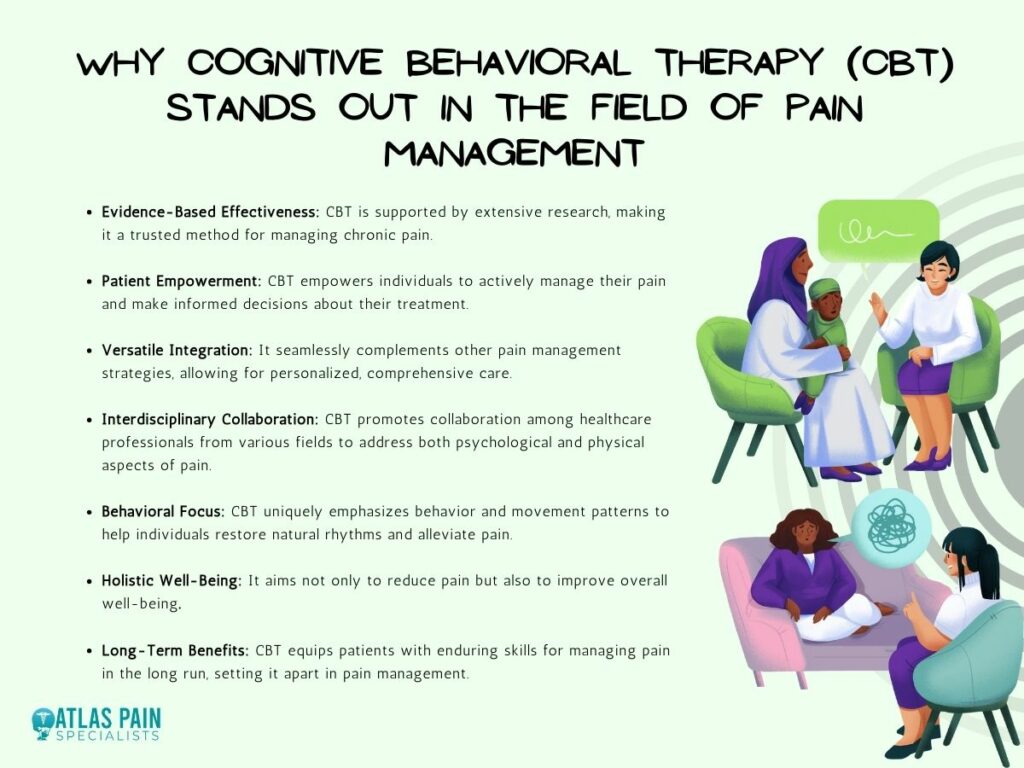
- Evidence-Based Approach: There is a large body of research that shows cognitive behavioral therapy (CBT) is beneficial in treating chronic pain. Several studies have shown that it can lessen the severity of pain, promote general well-being, and improve physical function.
- Patient Empowerment: Cognitive Behavioral Therapy (CBT) gives people the ability to actively manage their pain. It gives people the abilities and information needed to face obstacles brought on by suffering and take back control of their lives.
- Complementary Nature: The complementary nature of CBT allows it to work in harmony with other pain management techniques. It can be combined with physical therapy, medicinal therapies, and other modalities in a multidisciplinary approach.
The Complex Nature of Chronic Pain
Beyond just physical sensations, chronic pain exists on a deeper level. It encompasses mental and emotional domains as well, resulting in a complex web of interactions.
- Psychological Impact: Stress, anxiety, and despair are often brought on by chronic pain. Chronic pain might weaken a person's ability to bounce back mentally and emotionally.
| Psychological Issue | Description |
| Anxiety | Chronic pain can trigger constant worry and fear about the future. |
| Depression | Prolonged pain often leads to feelings of sadness and despair. |
| Stress | Chronic pain can generate significant stress and tension. |
| Sleep Disturbances | Pain-related discomfort can disrupt sleep, leading to exhaustion. |
Emotional Distress: Having chronic pain frequently leads to psychological pain, which can take the form of annoyance, rage, despair, or hopelessness. These feelings make the pain even more intense.- Social and Interpersonal Challenges: People with chronic pain may become withdrawn or irritated, which can strain relationships. Isolation from others and a lower standard of living may follow.
The Synergy of CBT in Multidisciplinary Pain Management
Cognitive-behavioral therapy (CBT) works best when combined with other pain management strategies; it is not a stand-alone treatment. Its capacity to deal with the psychological effects of pain enhances other forms of therapy, making it an important element:
- Psychological Resilience: CBT equips individuals with tools to manage the emotional and psychological distress associated with pain, helping them build resilience.
- Behavioral Adaptation: CBT encourages individuals to engage in activities that improve their quality of life, even in the presence of pain, which aligns with the goals of physical therapy and other treatments.
Real-World Examples
To illustrate the practical benefits of integrating CBT into multidisciplinary pain management, let's consider a few real-world examples:
- Case 1: Pain Medication and CBT: A patient undergoing pain medication treatment may experience side effects or fears about dependency. CBT can help address these concerns, making medication more effective.
- Case 2: Physical Therapy and CBT: A patient participating in physical therapy may encounter challenges with motivation due to pain. CBT can provide strategies to overcome these barriers, ensuring that physical therapy is more successful.
Complementary Aspects of CBT in Pain Management Strategies
Combining CBT with these interdisciplinary elements creates a complete pain management strategy that takes into account both the psychological and physical aspects of chronic pain. Healthcare professionals can ensure that patients receive a comprehensive treatment plan that maximizes the advantages of each intervention while minimizing its drawbacks by working together and coordinating care.
| Pain Management Strategy | Complementary Aspects of CBT |
| Medication | Addressing medication-related concerns and side effects. |
| Physical Therapy | Overcoming motivational and behavioral barriers. |
| Psychological Interventions | Reinforcing psychological resilience and coping strategies. |
1. Medication
Medication is one of the pillars of pain management, especially when dealing with moderate to severe chronic pain. It can take various forms, including:
- Analgesics
- Antidepressants and Anticonvulsants
- Muscle Relaxants
- Topical Medications
- Antianxiety Medications
Patients frequently express worries regarding painkillers, including worries about possible combinations, side effects, and dependence. CBT gives patients a platform to communicate their anxieties and gives them the behavioral and cognitive tools they need to control them.
The emotional and psychological components of pain can influence how well a drug is thought to work. CBT can assist patients in controlling their anxiety connected to pain, which can intensify their pain perception.
2. Physical Therapy
Physical therapy is a crucial part of pain management, especially for diseases involving neurological or musculoskeletal problems. Physical therapists are skilled at relieving pain, increasing strength, promoting mobility, and preventing additional damage.
Physical therapy can include a range of techniques, such as:
- Exercise Programs
- Manual Therapy
- Education
- Modalities, i.e., ultrasound, electrical stimulation, or hot/cold therapy to alleviate pain and promote healing.
Keeping up motivation for physical therapy is one of the biggest obstacles for people with chronic pain. Pain can be demoralizing and can contribute to hopelessness, which makes it hard for patients to stick with their treatment plans.
This is where cognitive behavioral therapy (CBT) can help, as it gives patients the skills they need to get over behavioral and motivational obstacles. Cognitive behavioral therapy (CBT) assists patients in altering their negative thought patterns and motivates them to participate in physical treatment with grit and hope.
Physical therapy can also be uncomfortable and physically taxing at times. Even though it's essential for healing, some patients may find it to be a major obstacle.
Cognitive Behavioral Therapy (CBT) provides pain management skills to patients, such as mindfulness, relaxation methods, and behavioral modifications that improve their ability to participate in physical therapy. By teaching people to live with pain and use useful coping strategies, cognitive behavioral therapy (CBT) makes physical treatment more tolerable and efficient.
3. Psychological Interventions
Pain management requires the application of psychological therapy. They include a range of methods and therapies aimed at treating the psychological and emotional components of pain.
These interventions, which are provided by mental health specialists, can include:
- Individual Counseling
- Group Therapy
- Relaxation Techniques
- Coping Strategies
- Reinforcing Psychological Resilience
- Behavioral Adaptation and Emotional Regulation
Chronic pain patients may experience both severe emotional distress and physical pain. CBT complements these therapies by giving patients the behavioral and cognitive skills they need to control their emotional pain better.
CBT also emphasizes behavioral adaptation and emotional regulation, which is a complement to other psychological therapy. People learn how to incorporate the cognitive skills they learn via CBT into their daily lives in group therapy or support sessions.
Are Alternative Pain Management Techniques Effective?
By treating the psychological and emotional elements that frequently accompany pain, CBT gives patients the tools they need to comprehend, deal with, and control their condition.
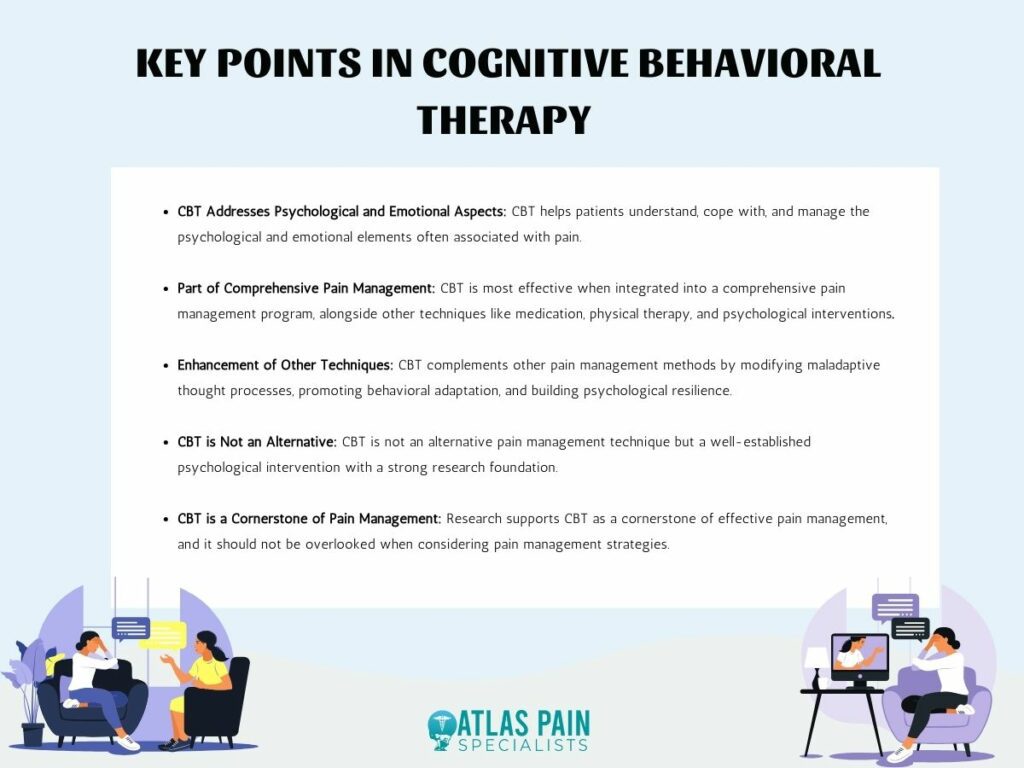
However, it's critical to understand that CBT works best when included in a comprehensive pain management program, as is the case with any therapy strategy.
Providing comprehensive care calls for CBT work in conjunction with other pain management techniques such as medicine, physical therapy, and psychological interventions. Through the modification of maladaptive thought processes, the encouragement of behavioral adaptation, and the promotion of psychological resilience, CBT enhances these techniques.As we've seen, cognitive behavioral therapy (CBT) is a common psychological intervention—not an alternative. Remember that CBT is a cornerstone of good pain management, as evidenced by research, and should not be overlooked when considering alternative pain management strategies.
About Dr. Sean Ormond