
Understanding the Side Effects of Common Pain Medications
In the last decade, there has been an increase in the use of prescription drugs to manage chronic pain among individuals who do not have a thorough awareness of the side effects of common pain medications. Although each of these medications may help manage pain, it is not widely recognized that combining a wide range of medications might cause undesirable side effects.
There may be well-documented and ongoing studies into the adverse effects of pain medications, but what about the impact of these side effects on our daily lives? This article aims to highlight the prevalent physical and behavioral adverse effects of commonly used pain medicines, even though we may use them to understand the risks.
| Medication Class | Common Medications | Description | Common Side Effects |
| NSAIDs | Ibuprofen, Naproxen | Nonsteroidal anti-inflammatory drugs | Gastric irritation, ulcers, bleeding |
| Acetaminophen (Tylenol) | Acetaminophen | Pain reliever and fever reducer | Liver damage (with excessive use) |
| Opioid Analgesics | Oxycodone, Hydrocodone | Powerful pain relievers | Nausea, constipation, addiction risk |
| Muscle Relaxants | Cyclobenzaprine, Baclofen | Relax muscles and reduce spasms | Drowsiness, dizziness |
| Corticosteroids | Prednisone, Dexamethasone | Anti-inflammatory and immune system suppressant | Osteoporosis, weight gain, infections |
| Local Anesthetics | Lidocaine, Bupivacaine | Block pain signals in specific areas of the body | Localized numbness, skin irritation |
| Anticonvulsants | Gabapentin, Pregabalin | Stabilize nerve activity, used for neuropathic pain | Drowsiness, dizziness, weight gain |
| Antidepressants | Amitriptyline, Duloxetine | Alters neurotransmitter levels, used for pain and mood | Drowsiness, dry mouth, changes in mood |
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are used to treat pain, inflammation, and fever. They are essential for controlling headaches, muscle aches, and chronic inflammatory disorders like arthritis.
Anti-inflammatory drugs suppress cyclooxygenases (COX-1 and COX-2) enzymes. In reaction to injury or illness, these enzymes produce prostaglandins, which cause inflammation, pain, and fever.
Common Uses
There are several OTC and prescription NSAIDs. Common NSAIDs include Ibuprofen, Naproxen, Aspirin, and Celecoxib.
Multiple conditions can be treated with NSAIDs, including:
- Inflammatory Conditions: Anti-inflammatory NSAIDs help treat osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis.
- Fever reduction: NSAIDs reduce hypothalamic prostaglandin levels, which regulate body temperature.
Potential Side Effects
While NSAIDs are typically safe when used as indicated, they have risks.
- Gastrointestinal Effects: NSAIDs can cause stomach ulcers, bleeding, and perforation.
- Cardiovascular Risks: High doses or long-term usage of some NSAIDs may raise heart attack and stroke risk.
- Kidney Function: NSAIDs can impair kidney function, especially in people with kidney problems.
- Allergies: Although rare, NSAIDs can induce allergic responses such as hives, edema, or difficulty breathing.
- Interactions: NSAIDs can interact with blood thinners, steroids, and blood pressure medications.
- Pregnancy and Lactation: NSAIDs may affect developing fetuses and nursing infants.
2. Acetaminophen (Tylenol)
Acetaminophen, sold as Tylenol, is a popular OTC painkiller and fever reliever. Acetaminophen works differently from NSAIDs like ibuprofen and aspirin.
The mechanism is unknown, although it is thought to affect the central nervous system, notably the hypothalamus, which regulates body temperature and pain. Acetaminophen decreases brain prostaglandins, which cause fever and pain.
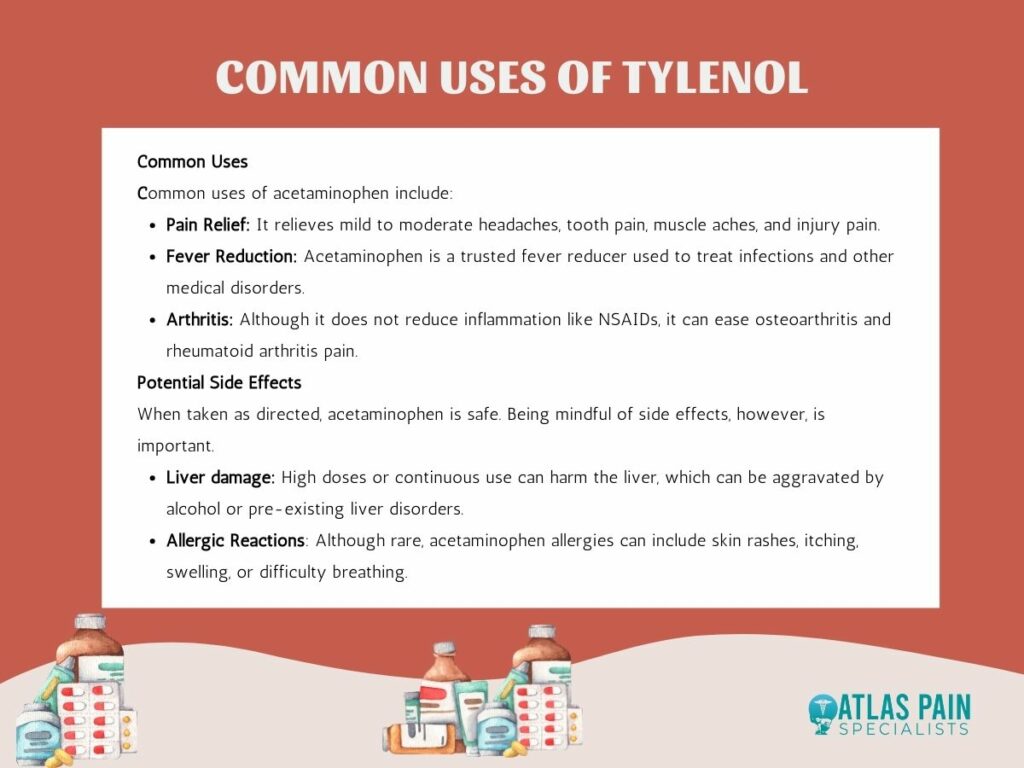
Common Uses
Common uses of acetaminophen include:
- Pain Relief: It relieves mild to moderate headaches, tooth pain, muscle aches, and injury pain.
- Fever Reduction: Acetaminophen is a trusted fever reducer used to treat infections and other medical disorders.
- Arthritis: Although it does not reduce inflammation like NSAIDs, it can ease osteoarthritis and rheumatoid arthritis pain.
Potential Side Effects
When taken as directed, acetaminophen is safe. Being mindful of side effects, however, is important.
- Liver damage: High doses or continuous use can harm the liver, which can be aggravated by alcohol or pre-existing liver disorders.
- Allergic Reactions: Although rare, acetaminophen allergies can include skin rashes, itching, swelling, or difficulty breathing.
3. Opioid Analgesics
Opioids are strong painkillers derived from or chemically related to opium poppies. By attaching to opioid receptors in the brain, spinal cord, and gastrointestinal tract, they help the body control pain.
Opioids relieve pain by blocking pain signals at these receptors.
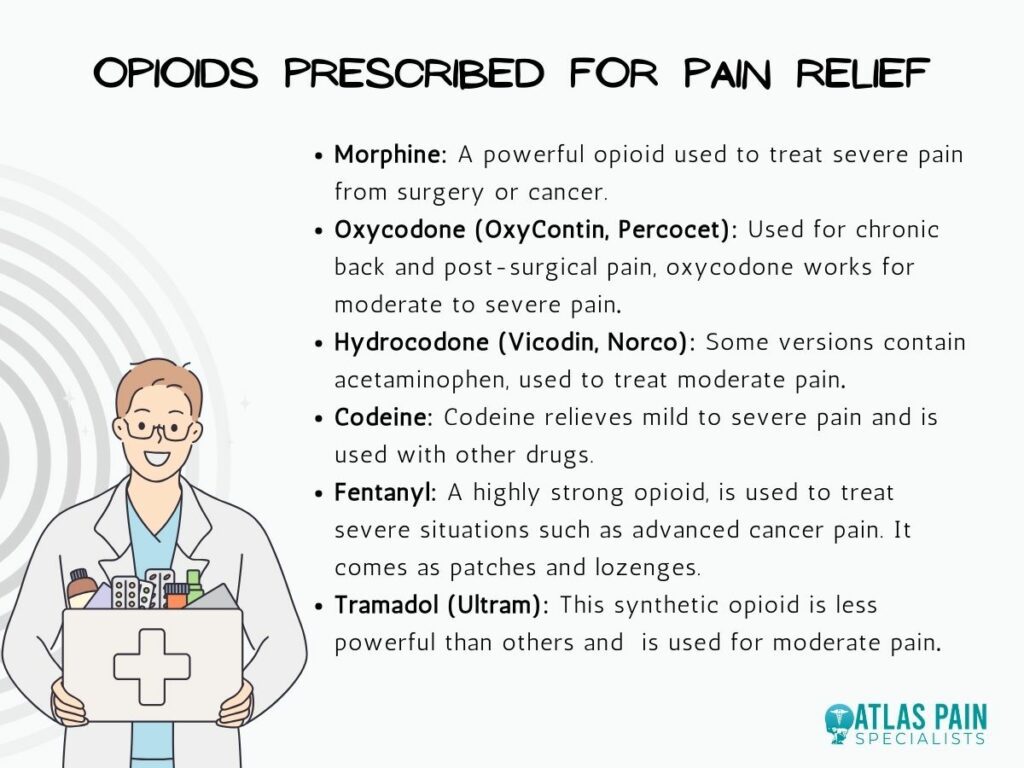
Common Uses
Several opioids are prescribed for pain relief. Common examples are:
- Morphine: A powerful opioid used to treat severe pain from surgery or cancer.
- Oxycodone (OxyContin, Percocet): Used for chronic back and post-surgical pain, oxycodone works for moderate to severe pain.
- Hydrocodone (Vicodin, Norco): Some versions contain acetaminophen, used to treat moderate pain.
- Codeine: Codeine relieves mild to severe pain and is used with other drugs.
- Fentanyl: a highly strong opioid, is used to treat severe situations such as advanced cancer pain. It comes as patches and lozenges.
- Tramadol (Ultram): This synthetic opioid is less powerful than others and is used for moderate pain.
Many pain disorders are treated with opioid analgesics:
- Acute pain: They manage acute pain well after surgery, injuries, or medical procedures.
- Chronic Pain: Used to treat cancer, severe back, and neuropathic pain.
- End-of-Life Care: They help terminally sick patients feel better.
Potential Side Effects
Opioids can effectively treat pain, but they have risks and must be used carefully:
- Addiction: Opioids have a high potency for addiction, leading to overuse, which can cause physical and mental dependence.
- Respiratory Depression: Opioids can delay or shallow breath, which can be fatal.
- Drowsiness and Impaired Coordination: Opioids can impair coordination and put drivers at risk.
- Constipation: Opioids can cause constipation, which may require extra medicine.
- Tolerance: Opioids can build tolerance, requiring greater doses to relieve pain.
4. Muscle Relaxants
Prescription muscle relaxants relieve muscle spasms, tension, and pain. These medications can treat acute injuries and persistent musculoskeletal diseases.
They relieve muscle spasms and tension by targeting the CNS. Blockers and antispasmodics are the main muscle relaxants.
- Neuromuscular Blockers: These medications paralyze muscles by blocking nerve signals. We use them during surgeries and medical procedures that require muscular relaxation.
- Antispasmodic agents: They reduce motor neuron excitability and muscle tone inside the central nervous system. Their purpose is to ease muscle spasms and pain.
Common Uses
Healthcare providers commonly prescribe several antispasmodic agents. These include:
- Cyclobenzaprine (Flexeril): Used to relieve musculoskeletal muscular spasms temporarily.
- Methocarbamol (Robaxin): Treats muscle spasms and pain.
- Baclofen (Lioresal): Used to treat muscle stiffness in multiple sclerosis and spinal cord injury.
- Tizanidine (Zanaflex): Treats muscle stiffness from multiple sclerosis or spinal cord injury like Baclofen.
- Diazepam (Valium): A benzodiazepine, diazepam can calm muscles and treat muscle spasms.
Muscle relaxants are prescribed for various conditions, including:
- Muscle Spasms: They relieve acute muscle spasms and cramps from injuries or fibromyalgia.
- Musculoskeletal Disorders: They help relieve low back pain, herniated discs, and muscular strains.
- Neurological Disorders: Muscle relaxants may relieve stiffness and increase movement in multiple sclerosis.
Potential Side Effects
When using muscle relaxants, it's crucial to be aware of potential side effects and consider certain factors:
- Drowsiness and Dizziness: This makes it important to avoid activities like driving or operating heavy machinery while taking them.
- Dependency: Long-term or abused muscle relaxants can cause physical dependency.
- Tolerance: Over time, the body may develop tolerance to these medications, requiring higher doses for the same effect.
- Withdrawal: Abruptly discontinuing muscle relaxants might cause withdrawal symptoms.
- Interactions: Muscle relaxants can interact with other medications.
5. Topical Analgesics
Applying topical analgesics to the skin relieves regional pain. Topical pain therapies are non-invasive and effective, especially for localized conditions.
They work by putting pain-relieving drugs right through the skin to the place that hurts. These drugs come in creams, gels, lotions, patches, and sprays.
Common Uses
There are many over-the-counter and prescription topical analgesics with different formulations and mechanisms of action. Common examples include:
- Lidocaine: Numbs skin and lowers pain signals and is often found in creams, gels, and patches.
- Capsaicin: Capsaicin creams and patches, made from chili peppers, deplete substance P, a pain-perception neurotransmitter relieving pain.
- Diclofenac: It is an NSAID available in gel or patch form and provides relief by reducing inflammation.
- Menthol and Camphor: These compounds provide a heating or cooling effect on the skin, diverting attention away from the area of pain.
Common uses of topical analgesics include:
- Muscle and Joint Pain: Topical analgesics can target arthritis, sprains, and strains.
- Neuropathy: Topical analgesics can relieve pain from diabetic neuropathy and post-herpetic neuralgia.
- Localized Pain: Topical treatments ease pain from small injuries, post-surgery, and chronic diseases without systemic effects.
Potential Side Effects and Considerations
Though safe and well-tolerated, topical analgesics have several drawbacks:
- Skin Irritation: Some individuals may experience skin irritation, redness, or burning at the application site.
- Allergic Reactions: Special compounds can cause allergic reactions, but they are rare.
- Interaction with Other Medications: Topical analgesics can interfere with other drugs.
6. Antidepressants
In general, antidepressants treat depression and mood disorders. These medications are multipurpose, including pain management.
Antidepressants alter certain brain neurotransmitters like serotonin and norepinephrine. These neurotransmitters regulate mood and pain perception. Thus, antidepressants can affect both.

Common Uses
Several classes of antidepressants are used in pain management:
- Tricyclic Antidepressants (TCAs): Among the earliest antidepressants, TCAs like amitriptyline and nortriptyline are commonly used in diabetic neuropathy, post-herpetic neuralgia, and fibromyalgia.
- Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs): Medications like duloxetine (Cymbalta) and venlafaxine (Effexor) are SNRIs that can treat depression and chronic pain.
- Selective Serotonin Reuptake Inhibitors (SSRIs): SSRIs like fluoxetine (Prozac) and sertraline (Zoloft) are mostly used for mood disorders, although they can also aid with pain and sadness in fibromyalgia.
- Atypical Antidepressants: Bupropion (Wellbutrin) is sometimes used to treat chronic pain, particularly neuropathic pain.
Treatments for pain with antidepressants include:
- Neuropathic Pain: These drugs work well for nerve injury or dysfunction-related pain.
- Fibromyalgia: Antidepressants can reduce pain and improve sleep.
- Chronic Pain: Antidepressants can treat both physical and emotional pain in chronic pain problems with mood changes.
Potential Side Effects
Consider the following negative effects when using antidepressants for pain management:
- Side Effects: Antidepressants can induce drowsiness, dizziness, dry mouth, constipation, and mood or behavior changes depending on the medicine.
- Drug Interactions
7. Anticonvulsants
Anticonvulsants, sometimes called antiepileptic medicines (AEDs), treat seizures and epilepsy. However, these medicines are flexible and increasingly used to manage pain.
Anticonvulsants stabilize brain nerve cell activity, lowering seizure-causing electrical activity. By increasing inhibitory or inhibiting excitatory brain neuron signals, they can reduce chronic pain.
Common Uses
Certain anticonvulsants can help manage chronic pain:
- Gabapentin (Neurontin): Affects neuronal calcium channels and is used to treat neuropathic pain, including diabetic neuropathy and post-herpetic neuralgia.
- Pregabalin (Lyrica): Like gabapentin, pregabalin treats neuropathic pain and fibromyalgia by acting on central nervous system calcium channels.
- Carbamazepine (Tegretol): In addition to treating epilepsy, carbamazepine treats trigeminal neuralgia.
- Phenytoin (Dilantin): Stabilizes neuronal membranes and treats neuropathic pain.
Anticonvulsants are used to treat pain in numerous situations:
- Neuropathic Pain: They treat nerve injury or dysfunction-related pain well.
- Fibromyalgia: Gabapentin and pregabalin relieve broad musculoskeletal pain.
- Trigeminal Neuralgia: Carbamazepine is the main treatment for this facial pain.
- Chronic migraine prevention: Anticonvulsants like Topamax and Depakote are used.
Potential Side Effects
When using anticonvulsants for pain management, it's crucial to be aware of potential side effects and consider the following:
- Side Effects: Common side effects include dizziness, sleepiness, coordination issues, and gastrointestinal symptoms that differ per prescription.
- Drug Interactions
8. Local anesthetics
Local anesthetics inhibit pain in a specific location, allowing medical treatments to be performed without pain. Drugs like this are useful in dentistry and surgery.
Local anesthetics temporarily blocked nerve signals in a specific area. They block pain signals to the brain by interfering with nerve cell sodium channels. This causes transient numbness and loss of sensation in the treated area, making medical treatments painless.
Common Uses
Common local anesthetics include:
- Lidocaine is a popular local anesthetic found in creams, gels, injections, and patches.
- Bupivacaine: Injections of bupivacaine relieve pain longer.
- Procaine: It is used in dentistry and minor surgery.
- Tetracaine: Mostly used in ophthalmology for eye surgeries.
Local anesthetics are used in many medical procedures:
- Dentistry: Local anesthetics are used for fillings, extractions, and root canals by dentists.
- Surgery: Local anesthetics reduce the requirement for general anesthetic in minor surgeries and procedures.
- Maternal: Local anesthetic nerve blocks or epidurals can ease labor, childbirth, and persistent pain.
- Dermatology: These drugs are used for biopsies and mole removal.
Potential Side Effects
When using local anesthetics, consider these negative side effects:
- Allergic Reactions: Although rare, local anesthetics can cause irritation, redness, or swelling.
- Localized Reactions: Injection site redness, swelling, or numbness is typical and usually goes away.
- Overdose: Local anesthetic overdose or bloodstream absorption can cause toxicity and side effects.
- Duration of Action: The duration of pain relief varies depending on the specific local anesthetic used.
Are Alternative Pain Management Techniques Effective?
Pain intervention entails understanding common painkillers and their side effects. Following medical advice, we must use these drugs safely and monitor their effects.
However, alternative pain management approaches can relieve pain and reduce drug side effects. Acupuncture, mindfulness meditation, and physical treatment provide holistic relief.
Understanding drug side effects and using alternative approaches helps us make informed pain relief decisions. Learn whether alternative pain management techniques are as effective in reducing pain medication side effects and dependency.
About Dr. Sean Ormond