
Effective Strategies to Manage Pain After Surgery
You may be wondering what are some effective strategies to manage pain after surgery. Recovering from surgery can be challenging, especially when dealing with post-operative pain.
Surgery is an important medical intervention that can bring relief and improve quality of life. However, it is often accompanied by post-operative pain, which can be distressing and hinder recovery..
In this blog post, we'll explore proven strategies to effectively manage pain, enabling you to heal faster and improve your overall well-being. Learn how to navigate this critical phase of your recovery with confidence and comfort.
Table of Contents
Strategies to Manage Pain After Surgery
Effectively managing pain after surgery is essential not only for patient comfort but also for promoting faster healing and preventing complications.
We will delve into the importance of postoperative pain management and explore various strategies to help patients navigate this critical phase of their recovery journey.
What Causes Pain After Surgery
Post-operative pain arises due to a complex interplay of physiological and psychological factors. During surgery, tissue damage occurs, leading to the activation of pain receptors in the affected area.
Inflammation and the release of biochemical signals also contribute to pain sensation. The extent and nature of pain vary depending on factors such as the type of surgery, individual pain tolerance, and overall health condition.
Types of Postoperative Pain
a. Acute Pain
Acute pain is the most common type experienced after surgery and is usually of short duration. It is a direct result of tissue trauma during the procedure and is typically well-managed with medications prescribed by the surgical team.
b. Chronic Pain
In some cases, post-operative pain may persist beyond the expected healing period, becoming chronic. This type of pain can significantly impact a patient's quality of life, requiring specialized pain management approaches.
c. Referred pain
Referred pain occurs when pain is felt in an area distant from the surgical site. For instance, abdominal surgery may lead to pain perception in the shoulder due to shared nerve pathways.
Understanding referred pain is crucial in accurately diagnosing and managing post-operative discomfort.
d. Neuropathic Pain
Neuropathic pain results from nerve damage during surgery, leading to abnormal signaling and sensations. It is often described as burning, tingling, or shooting pain and requires targeted treatment modalities.
e. Phantom Limb Pain
Patients who undergo amputations may experience phantom limb pain, a pain sensation in the missing limb. This phenomenon is complex and involves both physical and psychological components.
The Role of Medications in Post-Operative Pain Management
After surgery, medications play a pivotal role in alleviating pain and enhancing patient comfort during recovery. Medical professionals utilize various types of medications to address different aspects of postoperative pain.
Let's explore some common medications used in pain management:
Opioids
Opioids are potent pain relievers that work by binding to specific receptors in the brain and spinal cord. They are often prescribed for managing moderate to severe postoperative pain.
While effective, opioids come with potential side effects, including drowsiness, constipation, nausea, and the risk of addiction or dependence. Due to these concerns, healthcare providers aim to use opioids judiciously and for the shortest duration possible.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs, such as ibuprofen and naproxen, are commonly prescribed to control post-operative pain and reduce inflammation. They work by inhibiting the production of prostaglandins, which are responsible for pain and inflammation.
While NSAIDs are generally well-tolerated, they can lead to stomach irritation, bleeding, and kidney problems, especially with prolonged use or in patients with certain medical conditions.
Acetaminophen
Acetaminophen is an analgesic and antipyretic medication that helps reduce pain and fever. It is often used in combination with other pain medications for comprehensive pain management.
Acetaminophen is generally considered safe when taken as directed, but excessive use can cause liver damage.
Local Anesthetics
Local anesthetics are administered to block pain signals in specific areas, providing targeted pain relief. They may be used during surgery or in post-operative wound care to alleviate discomfort without affecting the entire body. Common examples include lidocaine and bupivacaine.
Nerve Blocks
Nerve blocks involve injecting anesthetic medication near specific nerves to block pain signals from reaching the brain. These blocks can provide extended pain relief and may benefit certain surgical procedures or chronic pain conditions.
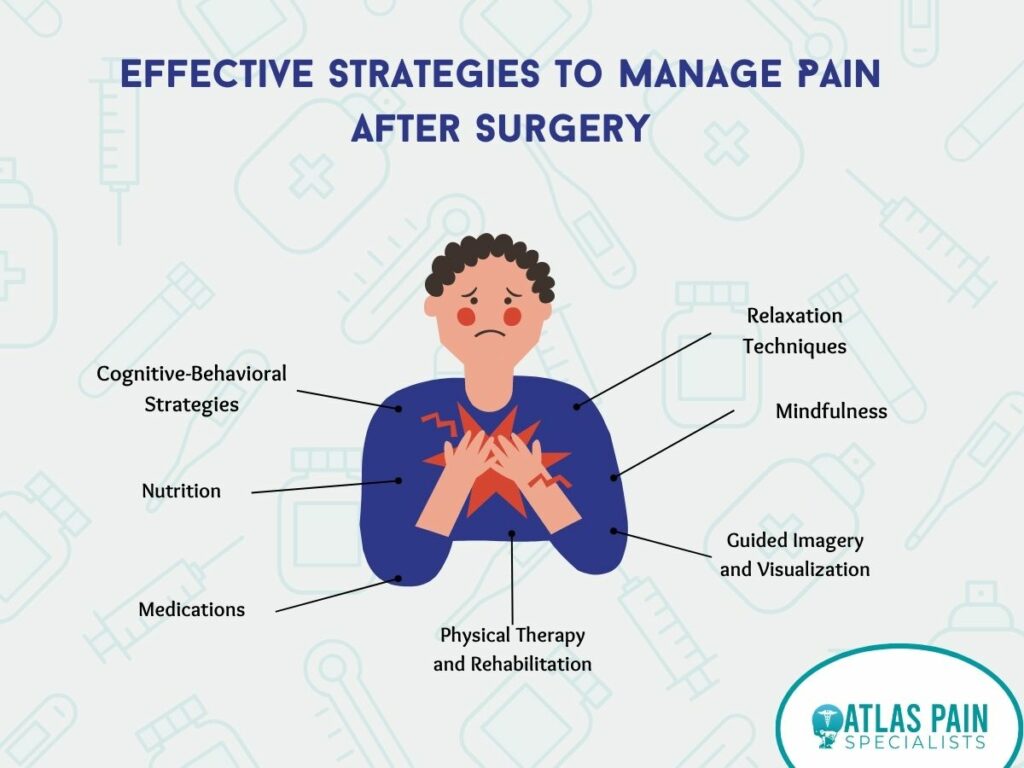
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation play a multidisciplinary approach that aims to improve mobility, strength, and function while reducing pain and minimizing the risk of complications.
- Reducing Pain and Inflammation
Physical therapists use various techniques to alleviate pain and inflammation, such as manual therapy, ice or heat applications, and transcutaneous electrical nerve stimulation (TENS).
These interventions can promote healing, reduce muscle tension, and improve blood circulation, reducing post-operative discomfort.
- Restoring Range of Motion and Strength
Post-surgery, patients may experience stiffness and weakness in the affected area. Physical therapy involves targeted exercises and stretches to restore the range of motion and strength gradually.
By strengthening the surrounding muscles, patients can better support the healing tissues and reduce strain on the surgical site.
- Functional Rehabilitation
Physical therapists focus on restoring functional abilities to help patients regain independence in daily activities. For example, a patient recovering from knee surgery may undergo exercises to improve walking, climbing stairs, and squatting.
- Preventing Complications
Physical therapy can help prevent postoperative complications, such as blood clots and pressure ulcers, by encouraging proper body positioning, movement, and circulation.
Non-Pharmacological Pain Management Techniques
In addition to medications and physical therapy, non-pharmacological pain management techniques offer alternative ways to alleviate post-operative discomfort. These approaches focus on harnessing the body's natural healing abilities and promoting relaxation.
Let's explore some effective non-pharmacological techniques commonly used for postoperative pain management:

- Acupuncture
Acupuncture is an ancient Chinese therapy that involves inserting thin needles into specific points on the body to stimulate energy flow and promote pain relief.
Several studies have demonstrated its effectiveness in managing various types of pain, including postoperative pain. Acupuncture is considered safe when performed by trained practitioners.
2. Biofeedback
Biofeedback is a technique that helps individuals gain control over physiological processes, such as heart rate and muscle tension, by providing real-time feedback. By learning to regulate these bodily functions, patients can reduce stress and manage pain more effectively.
Biofeedback has shown promise in post-operative pain management and is often used as a complementary therapy.
3. Transcutaneous Electrical Nerve Stimulation (TENS)
TENS involves using a small battery-operated device that delivers low-level electrical currents to the skin through electrodes. These electrical impulses help disrupt pain signals and stimulate the release of endorphins, the body's natural painkillers.
TENS has been found to relieve various types of acute and chronic pain, making it a valuable option for postoperative pain management.
4. Mindfulness and Meditation
Mindfulness and meditation encourage focused awareness and relaxation, reducing stress and enhancing pain coping mechanisms. Studies have shown that mindfulness-based interventions can significantly reduce post-operative pain and improve overall well-being.
5. Guided Imagery
Guided imagery involves using visualizations and mental imagery to create a calming and positive experience. This technique helps divert attention away from pain and promotes relaxation, leading to pain relief and reduced anxiety.
6. Heat and Cold Therapy
Applying heat or cold to the affected area can effectively manage post-operative pain and inflammation. Heat therapy helps increase blood flow, relax muscles, and ease pain, while cold therapy can reduce swelling and numb the area.
7. Music Therapy
Listening to soothing music can trigger the release of endorphins and distract from the pain, offering emotional comfort during recovery.
Role of Nutrition in Post-Operative Recovery and Pain Management
Nutrition plays a crucial role in post-operative recovery, supporting the body's healing processes and aiding in pain management. A well-balanced diet provides essential nutrients for tissue repair, immune function, and overall well-being during healing.
a. Reducing inflammation
Inflammation is a natural response to surgery, but excessive inflammation can prolong recovery and exacerbate pain. Incorporating anti-inflammatory foods into the diet, such as fatty fish (rich in omega-3 fatty acids), colorful fruits and vegetables (high in antioxidants), and nuts, can help control inflammation and ease post-operative discomfort.
b. Protein for Tissue Repair
Protein is a critical nutrient for tissue healing and repair. Including lean sources of protein, like poultry,
fish, tofu, and beans, can support wound healing and muscle recovery after surgery.
c. Vitamin C for Collagen Formation
Vitamin C is essential for collagen formation, a structural protein that aids in wound healing. Citrus fruits, strawberries, broccoli, and bell peppers are excellent sources of vitamin C.
d. Vitamin A for Immune Function
Vitamin A supports the immune system and helps maintain the integrity of mucous membranes, which play a role in wound healing. Foods like sweet potatoes, carrots, and spinach are rich in vitamin A.
e. Zinc for Tissue Growth and Repair
Zinc is involved in various enzymatic reactions that facilitate tissue growth and repair. Foods like lean meats, whole grains, nuts, and seeds are good sources of zinc.
f. Hydration
Adequate hydration is essential for overall health and healing. Staying hydrated can help prevent complications, improve blood flow, and facilitate the elimination of toxins from the body.
Psychological Strategies for Managing Post-Operative Pain
Psychological approaches are valuable tools in managing post-operative pain, as they address the emotional and cognitive aspects of pain perception. Integrating these strategies into the recovery process can significantly enhance pain management and overall well-being.
- Cognitive-Behavioral Strategies
Cognitive-behavioral techniques focus on identifying and challenging negative thought patterns and behaviors that contribute to pain perception. By learning coping skills and adopting healthier thought processes, patients can modify their response to pain and reduce its impact on their daily lives.
Cognitive-behavioral therapy (CBT) has been proven effective in managing various types of pain, including postoperative pain.
2. Mindfulness
Mindfulness practices involve cultivating present-moment awareness without judgment. By staying attuned to their sensations and emotions, patients can develop a non-reactive attitude toward pain, effectively reducing suffering.
Mindfulness-based interventions have shown promising results in reducing post-operative pain intensity and improving pain-related outcomes.
3. Relaxation Techniques
Relaxation techniques, such as progressive muscle relaxation and deep breathing exercises, help reduce muscle tension and promote a sense of calmness. Engaging in relaxation practices can alleviate anxiety and stress, which can contribute to heightened pain perception.
4. Guided Imagery and Visualization
Guided imagery involves using mental images to create a soothing and positive experience. By
visualizing pleasant scenes or sensations, patients can distract their minds from pain, increasing relaxation and comfort.
Key Takeaway
Effective postoperative pain management is crucial for a smooth recovery. Atlas Pain Specialists excel in implementing comprehensive strategies to manage pain after surgery.
From personalized medication plans to non-pharmacological techniques like acupuncture and mindfulness, they prioritize patient comfort and well-being.
By integrating medical expertise with holistic approaches, Atlas Pain Specialists empower patients to heal faster, minimize discomfort, and improve overall quality of life during the critical post-surgery phase.
About Dr. Sean Ormond