Non-Pharmacological Pain Management Techniques
Pain management is an important component of healthcare to relieve pain and improve the quality of life for individuals experiencing it. While pharmacological interventions such as pain medications play a crucial role in pain relief, there is growing recognition of the importance of non-pharmacological techniques in managing pain effectively.
These non-pharmacological approaches encompass a diverse range of strategies that address pain through methods other than medication, offering alternative or complementary options for pain relief.
In recent years, there has been a shift towards a more holistic approach to pain management, recognizing that pain is a complex and multifaceted experience influenced by biological, psychological, and social factors. In this article we will talk on non-pharmacological pain management techniques.
Understanding Pain
Pain is a complex and multifaceted sensation experienced by individuals in response to various stimuli. It serves as a crucial physiological mechanism that alerts the body to potential harm or injury.
However, pain is not solely a physical phenomenon; psychological, social, and emotional factors also influence it. Understanding the nature of pain involves examining its different dimensions and how they interact to shape an individual's experience.
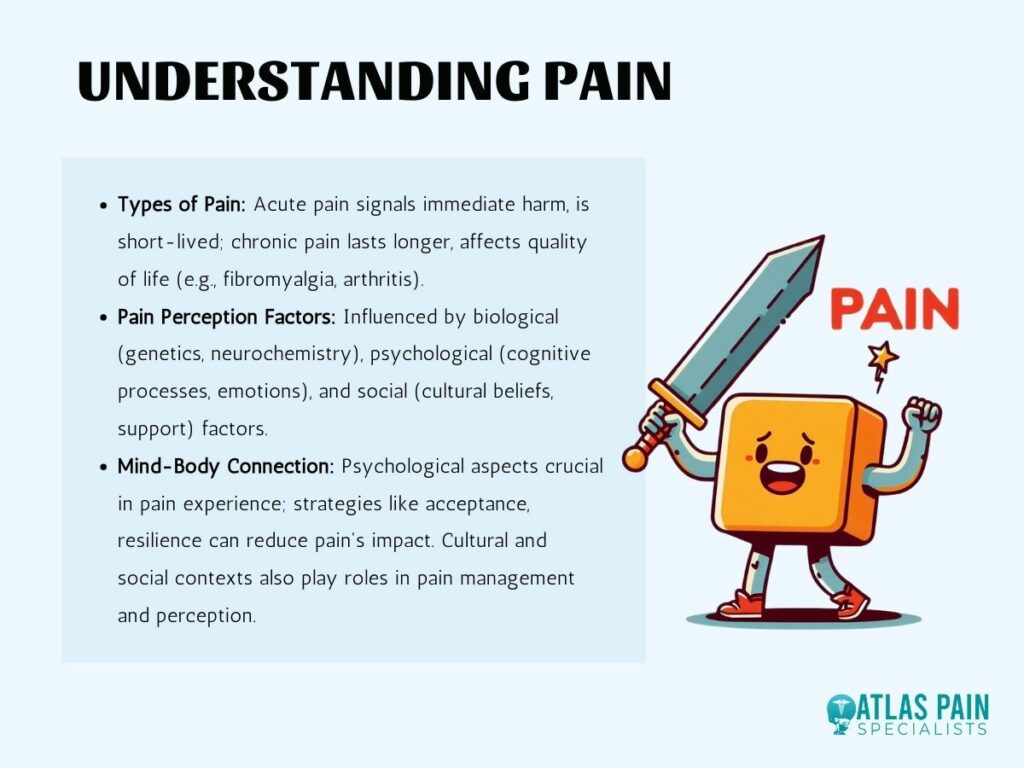
1. Types of Pain
There are two primary kinds of pain that can be broadly differentiated: acute and chronic. Acute pain is the body's warning signal and usually appears rapidly in response to injury or tissue damage.
Acute pain is sharp, intense quality often characterizes it and is usually short-lived, resolving once the underlying cause is treated or healed. Common examples of acute pain include a stubbed toe, a paper cut, or a muscle strain during physical activity.
Chronic pain persists over an extended period, typically lasting for three months or more. Conditions such as fibromyalgia, arthritis, and neuropathy are examples of chronic pain disorders that can have a profound impact on those affected.
2. Factors Influencing Pain Perception
Pain perception is not solely determined by the severity of tissue damage or injury; rather, it is influenced by many factors that modulate how pain signals are processed and interpreted by the brain. These factors can be broadly categorized into biological, psychological, and social determinants.
Biological factors encompass physiological processes that contribute to pain perception, including genetics, neurochemistry, and the functioning of the nervous system. For instance, individual differences in pain sensitivity can be partially attributed to genetic variations in pain-related genes and neurotransmitter systems.
3. The mind-body connection in pain management
Psychological factors play a significant role in shaping an individual's experience of pain. These include cognitive processes, emotional states, and past experiences that influence how pain is perceived and managed.
For example, catastrophizing, or magnifying the threat of pain, can exacerbate pain intensity and disability, while positive coping strategies such as acceptance and resilience can mitigate the impact of pain.
Social determinants such as cultural beliefs, social support, and socioeconomic status also influence pain perception and management. Cultural norms and beliefs about pain can shape individuals' attitudes toward seeking treatment and expressing pain-related behaviors.
Non-Pharmacological Pain Management Techniques
Non-pharmacological pain management techniques offer a diverse array of strategies that aim to alleviate pain and improve overall well-being without relying on medication. These approaches recognize the complex nature of pain and address it from various angles, including psychological, physical, and emotional dimensions.
Cognitive-Behavioral Strategies
Cognitive-behavioral strategies form a cornerstone of non-pharmacological pain management, focusing on the interplay between thoughts, emotions, and behaviors in shaping the pain experience. These techniques are rooted in the understanding that maladaptive cognitive patterns and negative emotions can exacerbate pain perception and interfere with daily functioning.
- Relaxation Techniques
Relaxation techniques aim to reduce muscle tension, stress, and arousal levels, thereby promoting a sense of calm and relaxation throughout the body. Deep breathing exercises involve slow, diaphragmatic breathing patterns that help activate the body's relaxation response, counteracting the physiological effects of stress and tension.
Progressive muscle relaxation is a technique that helps people become more mindful of their muscle tension and learn to release it voluntarily. It involves gradually tensing and relaxing different muscle groups. Guided imagery and visualization techniques use mental imagery to evoke calming and pleasant sensations, redirecting attention away from pain and towards positive experiences.
- Cognitive Restructuring
Cognitive restructuring involves identifying and challenging negative or distorted thoughts and beliefs about pain. Common cognitive distortions include catastrophizing (exaggerating the severity or consequences of pain), overgeneralization (assuming that one painful experience predicts future outcomes), and all-or-nothing thinking (viewing situations in black-and-white terms).
Through cognitive restructuring, individuals learn to examine the evidence for and against their negative thoughts, reframe them in more balanced and realistic ways, and develop more adaptive coping strategies. This process helps individuals regain a sense of control over their thoughts and emotions, reducing anxiety and fear related to pain and enhancing their ability to cope effectively.
- Cognitive-behavioral therapy (CBT)
Cognitive-behavioral therapy (CBT) is a structured, evidence-based psychological intervention that combines cognitive restructuring with behavioral techniques to address pain-related distress and disability. In CBT, individuals work collaboratively with a therapist to identify specific goals, develop coping skills, and implement behavior change strategies.
These may include activity pacing, goal setting, problem-solving, and assertiveness training. Patients can make positive adjustments and enhance their overall quality of life by using CBT to help them understand the relationship between their ideas, emotions, and behaviors.
Physical Therapies
Physical therapies encompass a wide range of non-pharmacological interventions to improve physical function, reduce pain, and enhance overall mobility and flexibility. These therapies address musculoskeletal imbalances, improve biomechanics, and promote tissue healing, all contributing to pain relief and functional restoration.
Physical therapists are central in designing individualized treatment plans that target specific impairments and functional limitations, incorporating evidence-based interventions to optimize outcomes.
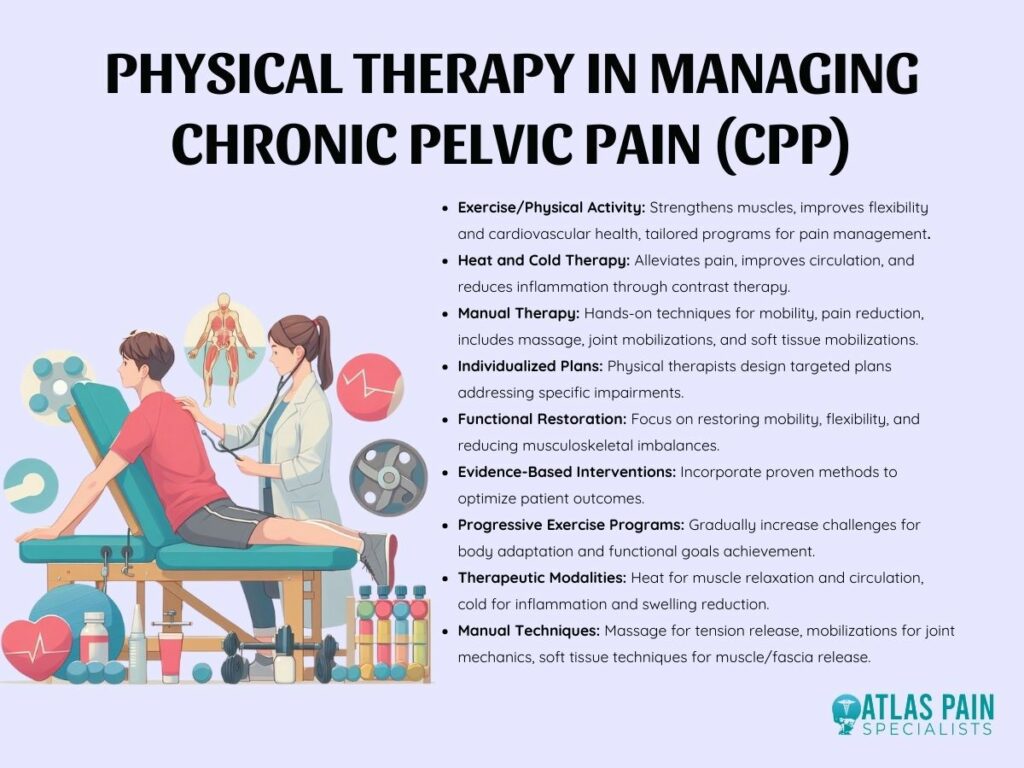
- Exercise and Physical Activity
Regular exercise is an important part of physical therapy interventions for pain management. Continuous physical activity has been shown to strengthen muscles, improve joint flexibility, and enhance cardiovascular fitness, all contributing to improved pain tolerance and overall well-being.
Physical therapists prescribe tailored exercise programs based on individual needs and preferences, incorporating aerobic, strength training, and flexibility exercises. Exercise programs gradually progress over time to challenge the body and promote adaptation, focusing on achieving functional goals and optimizing long-term outcomes.
- Heat and Cold Therapy
Heat and cold therapy are commonly used physical modalities for pain management, offering therapeutic benefits through their effects on tissue temperature and blood flow. Switching between heat and cold therapy, known as contrast therapy, can relieve pain and promote tissue healing by alternating vasoconstriction and vasodilation responses.
Heat therapy, such as hot packs, warm baths, or heating pads, helps relax muscles, improve circulation, and alleviate stiffness and soreness. Heat can also help reduce muscle spasms and increase tissue extensibility, making it particularly beneficial for chronic conditions characterized by muscle tightness and stiffness.
Cold therapy, using ice packs, cold compresses, or cryotherapy modalities, helps reduce inflammation, numb pain, and decrease swelling associated with acute injuries or inflammatory conditions.
- Manual Therapy
Manual therapy techniques involve hands-on manipulation of soft tissues and joints to improve mobility, reduce pain, and restore function. Physical therapists may use a variety of manual therapy approaches, including massage therapy, joint mobilizations, and soft tissue mobilizations, to address musculoskeletal dysfunction and alleviate pain.
Massage therapy involves applying pressure and kneading techniques to muscles and soft tissues, helping release tension, improve circulation, and promote relaxation. Joint mobilizations focus on restoring normal joint mechanics and range of motion by applying graded oscillatory or sustained forces to specific joint surfaces.
Soft tissue mobilizations target tight or restricted muscles, fascia, and connective tissues, using techniques such as myofascial release, trigger point therapy, and instrument-assisted soft tissue mobilization (IASTM). Manual therapy interventions are often combined with exercise and other modalities to optimize outcomes and promote long-term recovery.
Alternative Therapies
Alternative therapies encompass a diverse range of non-pharmacological interventions that offer alternative approaches to traditional medical treatments for pain management. These therapies draw upon various holistic modalities and complementary practices, often rooted in traditional healing systems and philosophies.
While the scientific evidence supporting some alternative therapies may vary, many individuals find relief and benefit from these approaches, either as standalone treatments or as complementary additions to conventional medical care. Integrating alternative therapies into a comprehensive pain management plan can provide additional options for individuals seeking natural and holistic approaches to improve their quality of life and well-being.
- Acupuncture
Tiny needles inserted on certain body points to promote energy flow and reestablish equilibrium are known as acupuncture, an ancient Chinese medical practice. Based on the concepts of traditional Chinese medicine, pain, and sickness stem from disruptions or imbalances in the meridians, the body's energy lines.
Acupuncture aims to regulate the flow of qi (vital energy) and promote healing by stimulating acupuncture points along these meridians. From a biomedical perspective, acupuncture may trigger the release of endorphins and other neurotransmitters, modulate pain signaling pathways, and promote anti-inflammatory effects.
- Chiropractic Care
Chiropractic care is a hands-on, manual therapy approach focused on diagnosing and treating musculoskeletal disorders, especially those affecting the spine and nervous system. Chiropractors use spinal adjustments, manipulations, and other manual techniques to restore normal function and alignment of the spine, joints, and surrounding tissues.
Chiropractic care aims to alleviate pain, improve mobility, and enhance overall health and well-being by correcting spinal misalignments (subluxations) and addressing biomechanical imbalances. Chiropractic adjustments may stimulate the nervous system, promote natural healing, and release muscle tension.
Chiropractic care is commonly sought for pain conditions such as lower back pain, neck pain, headaches, and sciatica, with many individuals reporting significant pain relief and functional improvement following treatment.
- Biofeedback
Biofeedback is a mind-body therapy that utilizes electronic monitoring devices to measure and provide feedback on physiological processes such as heart rate, muscle tension, and skin temperature. Patients can gain greater awareness and voluntary control over their bodily functions, including those related to pain perception and stress management by learning to control these physiological responses.
Biofeedback techniques may include relaxation training, guided imagery, and mindfulness practices combined with real-time feedback from monitoring devices. Through regular practice and feedback, individuals can develop self-regulation skills and reduce pain intensity, muscle tension, and other stress-related symptoms.
Mind-Body Practices
Mind-body practices include diverse techniques and therapies that focus on the interconnectedness of the mind, body, and spirit to promote good health and well-being. These practices recognize the powerful influence of mental and emotional states on physical health, including pain perception and management.
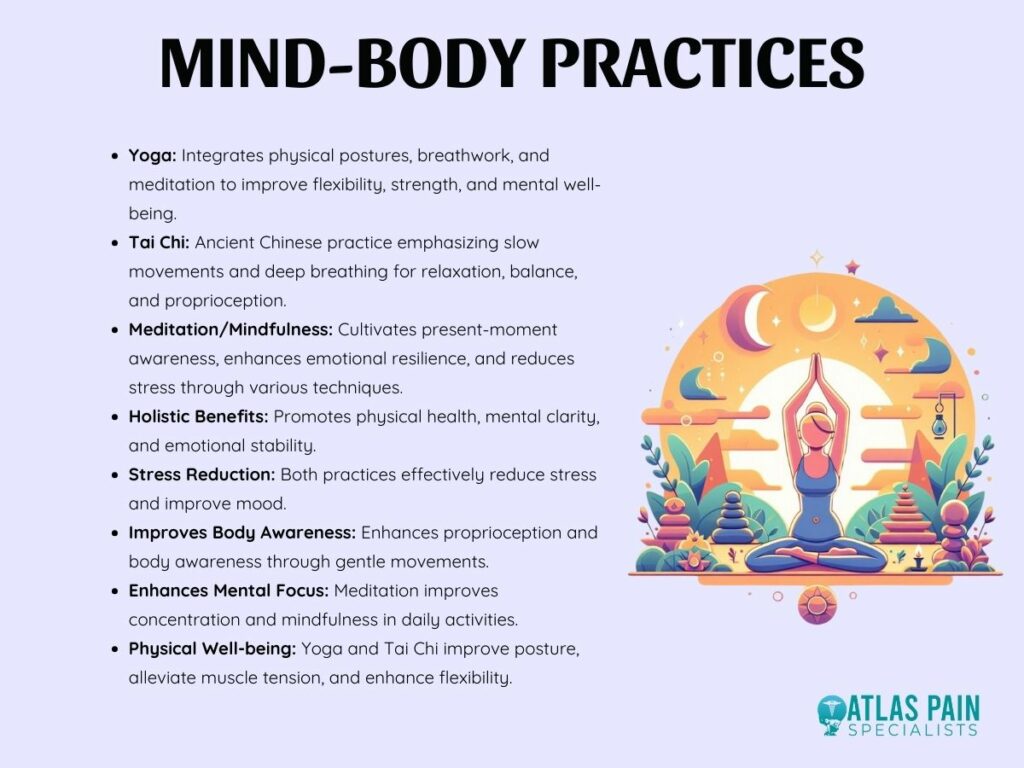
- Yoga
Yoga is a holistic mind-body practice originating from ancient Indian philosophy and tradition. It combines physical postures (asanas), breathwork (pranayama), meditation, and relaxation techniques to promote physical, mental, and spiritual well-being. The practice of yoga emphasizes the integration of movement, breath, and mindfulness, fostering a sense of inner balance, harmony, and self-awareness.
From a physical perspective, yoga can improve flexibility, strength, and posture, alleviate muscle tension, and enhance body awareness. Psychologically, yoga promotes relaxation, reduces stress, and enhances mood and emotional resilience.
- Tai Chi
Tai Chi, also known as Tai Chi Chuan or Taiji, is a mind-body practice originating from ancient Chinese martial arts traditions. It consists of slow, flowing movements, coordinated with deep breathing and mindful awareness, designed to promote relaxation, balance, and internal energy flow (qi).
Tai Chi emphasizes gentle, low-impact movements performed with focused attention and intention, fostering a state of inner calm, presence, and centeredness. From a physical perspective, Tai Chi can improve balance, coordination, and flexibility, reduce muscle tension, and enhance proprioception (awareness of body position in space).
- Meditation and Mindfulness
Meditation and mindfulness practices involve cultivating present-moment awareness and nonjudgmental acceptance of one's thoughts, feelings, and bodily sensations. These practices draw upon contemplative traditions from various spiritual and cultural backgrounds, including Buddhism, Hinduism, and secular mindfulness-based approaches.
Meditation techniques may include focused attention (such as breath awareness or mantra repetition), open monitoring (observing thoughts and sensations without attachment), loving-kindness (cultivating compassion towards oneself and others), and body scan (bringing awareness to different parts of the body). Mindfulness practices involve bringing mindful awareness to everyday activities, such as eating, walking, or listening, to promote greater presence, intentionality, and well-being.
Benefits of Personalized Pain Management Plans
Personalized pain management plans are tailored approaches that take into account an individual's unique needs, preferences, and circumstances in addressing their pain. Unlike a one-size-fits-all approach, a personalized plan takes into account your unique needs and preferences, ensuring a more targeted and practical approach to alleviating your pain.
When discussing non-pharmacological pain management techniques, it's crucial to create personalized plans that consider various factors such as the type and severity of pain, underlying medical conditions, lifestyle factors, and treatment goals.
With the help of a multidisciplinary team of healthcare professionals, you can receive enhanced support and education on pain management techniques, medication management, and lifestyle modifications.
About Dr. Sean Ormond