Acute vs. Chronic Pain: What Are The Differences?
What is the difference between acute vs. chronic pain? Understanding the concept of pain, a ubiquitous phenomenon experienced by all, is integral in the medical field and equally significant for individuals. Pain can be classified into two broad categories: acute and chronic.
The difference between these two forms of pain is far from just semantics; it affects how the pain is understood, managed, and treated. This article will delve into the complexities of acute and chronic pain, elucidating their characteristics, causes, and treatment strategies.
Table of Contents
Defining Acute and Chronic Pain
Acute and chronic pain, while similar in causing discomfort, possess distinct differences. Acute pain is short-term, signaling the body about potential harm and prompting immediate action. For example, the pain experienced when touching a hot stove instigates an instant withdrawal response, protecting from a burn.
In contrast, chronic pain, persisting beyond the typical healing time, becomes a debilitating condition itself. It may arise from initial injuries or medical conditions like arthritis or cancer, sometimes without a clear cause. This enduring pain affects overall quality of life, functionality, and mental health.
With its variable intensity and frequency, chronic pain's unpredictability increases psychological distress and complicates diagnosis and treatment. It necessitates a multi-dimensional and personalized approach to manage effectively.
While both acute and chronic pain contributes to discomfort, they differ fundamentally in their mechanisms, duration, psychological impact, and treatment strategies. Understanding these differences is crucial for healthcare professionals and individuals experiencing these types of pain, aiding in better management and improved well-being.
Understanding Acute Pain
Acute pain is a short-term type of pain that arises directly from tissue damage due to injuries, surgical procedures, or certain diseases. It can vary in intensity, from mild to severe, and in duration, from a few seconds to several weeks.
Its primary function is to act as a biological alarm, signaling the body of a possible threat and promoting defensive behaviors to aid healing. This pain is typically associated with observable body reactions like increased heart rate, high blood pressure, and increased breathing rate.
The nature and perception of acute pain can be influenced by numerous factors, including a person's overall health, psychological state, and cultural influences. Effective management of acute pain is crucial in preventing its progression to chronic pain, a persistent pain that can significantly impact a person's quality of life.
Understanding Chronic Pain
Chronic pain is a complex and persistent type of pain that lasts beyond the normal healing time of about three to six months. Unlike acute pain, which serves as a warning signal for the body, chronic pain often serves no biological purpose and may persist even after an injury has healed.
It can arise from various conditions such as arthritis, fibromyalgia, migraines, or back problems, and in some cases, its cause may be difficult to determine. Chronic pain can vary in intensity and can be constant or intermittent. It can significantly impact a person's ability to perform daily activities, and it is often accompanied by emotional and psychological distress, such as depression or anxiety.
Managing chronic pain can be challenging due to its persistent nature and the multifaceted factors that contribute to it. Due to the complex nature of chronic pain, successful management often requires a personalized approach that addresses the specific needs of each individual.
Acute Pain vs. Chronic Pain: Causes
Indeed, the difference between acute and chronic pain doesn't just lie in their duration but also in their underlying mechanisms and impacts on an individual's health and quality of life.
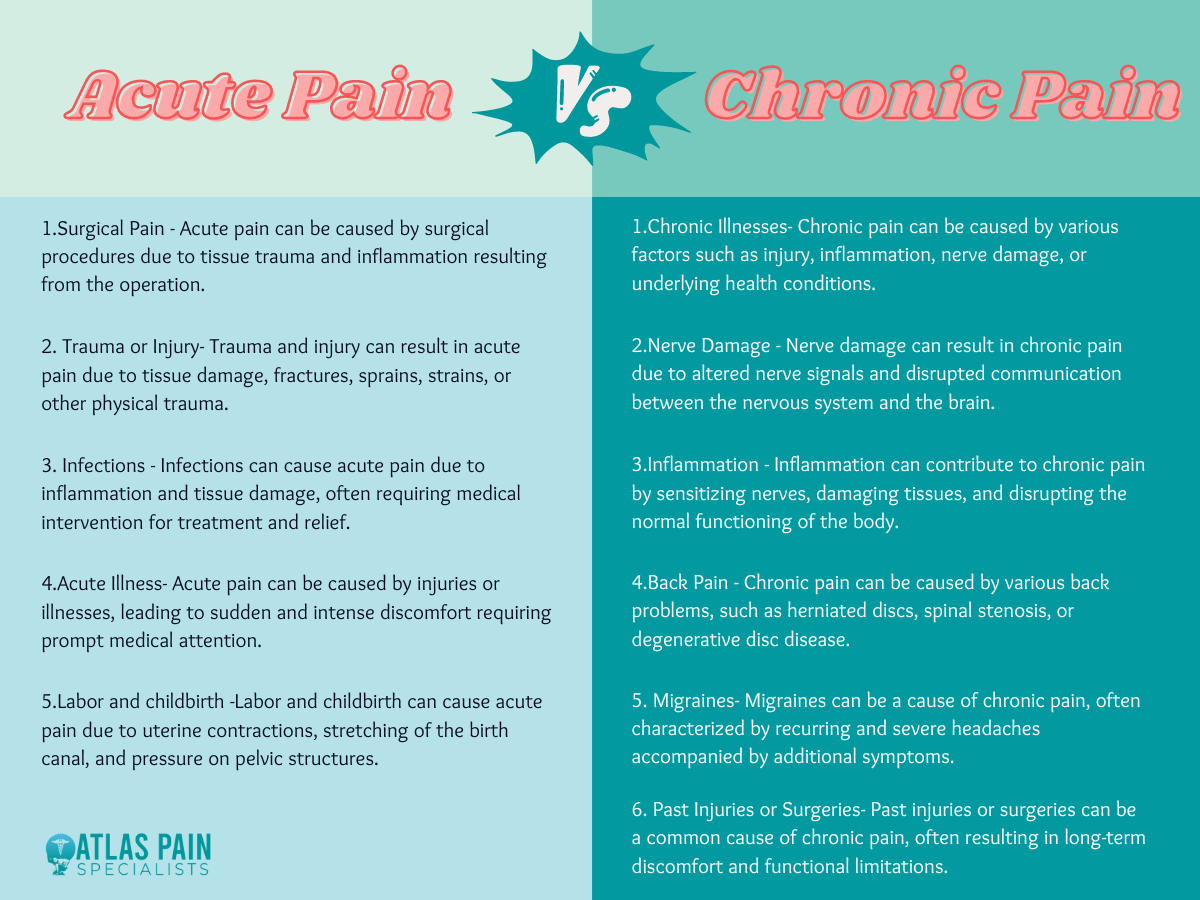
Acute Pain Causes
- Surgical Pain: This pain is common after going through surgical procedures and usually diminishes over time as the body heals.
- Trauma or Injury: Acute pain can result from falls, accidents, sports injuries, cuts, burns, or any situation that causes damage to the body's tissues.
- Infections: Acute pain can be associated with bacterial, viral, or other types of infection, often accompanying the inflammatory response triggered by the presence of the invading organisms.
- Acute Illness: Certain diseases or conditions like appendicitis, kidney stones, or gallstones can cause severe, acute pain.
- Labor and childbirth: This is a natural process that involves acute pain, which is often intense but resolves after delivery.
Chronic Pain Causes
- Chronic Illnesses: Conditions such as arthritis, cancer, fibromyalgia, multiple sclerosis, and neuropathic conditions can lead to chronic pain.
- Nerve Damage: Injuries or conditions that result in damage to the nervous system (neuropathy) can often result in chronic pain.
- Inflammation: Conditions characterized by inflammation, such as rheumatoid arthritis or other types of autoimmune diseases, can lead to prolonged pain.
- Back Problems: Chronic back pain can result from conditions like herniated discs, spinal stenosis, or spondylosis. In some cases, the exact cause of chronic back pain might be hard to determine.
- Migraines: Chronic headaches and migraines can cause ongoing pain.
- Past Injuries or Surgeries: Sometimes, pain can persist long after the tissues have healed from an injury or surgical procedure.
It's important to note that sometimes, chronic pain can occur without an identifiable physical cause, or it may be related to mental health conditions like depression and anxiety. The line between physical and psychological pain can be blurred in chronic pain conditions, and both aspects often need to be addressed in treatment.
Preventing Transition from Acute to Chronic Pain
Transitioning from acute to chronic pain can be a complex process that involves various factors, such as genetic predisposition, psychological factors, environmental influences, and the nature of the initial injury or disease.
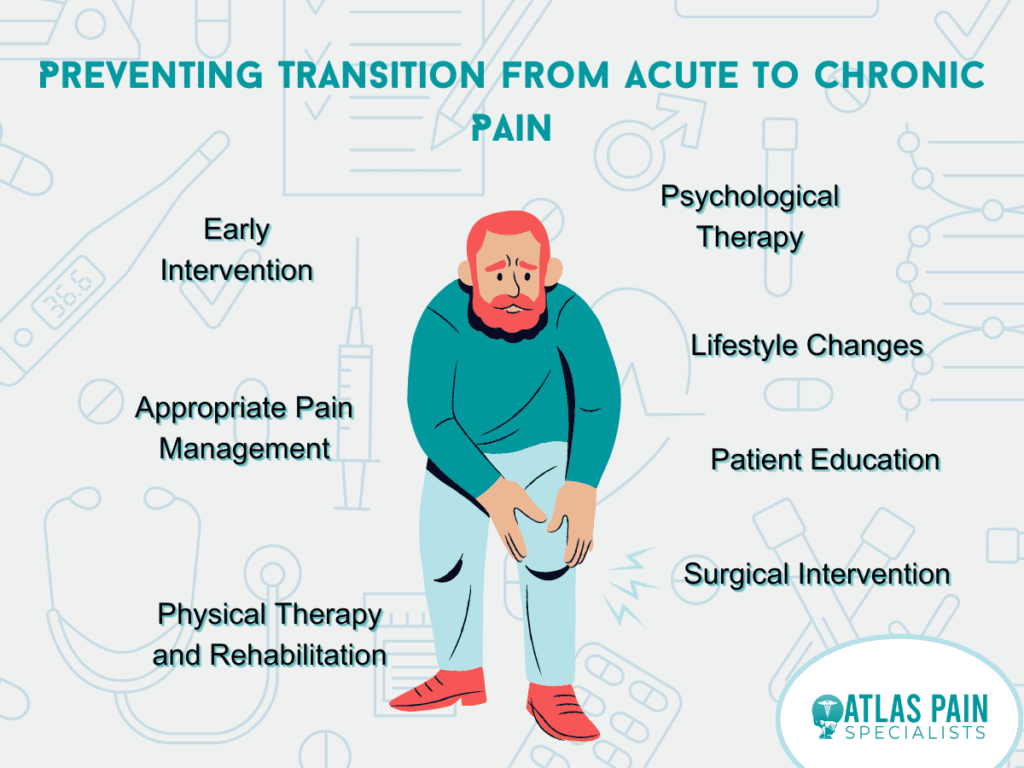
However, there are several strategies that can be implemented to prevent this transition. These include:
- Early Intervention:
The sooner pain is addressed, the less likely it is to become chronic. This means seeking treatment as soon as possible after an injury or onset of disease.
- Appropriate Pain Management:
This includes medications that specifically target the source of the pain, such as nonsteroidal anti-inflammatory drugs (NSAIDs) for inflammation, opioids for severe pain, and adjunctive medications such as antidepressants or anticonvulsants for neuropathic pain. It's important to note, however, that long-term use of certain pain medications, especially opioids, can actually contribute to the development of chronic pain, so they must be used judiciously.
- Physical Therapy and Rehabilitation:
Physical therapy exercises can reduce pain and improve function, preventing the disuse and muscle weakness that can contribute to chronic pain. A good physical therapy regimen often includes strength training, stretching, and aerobic exercise.
- Psychological Therapy:
Cognitive behavioral therapy (CBT) has been shown to be effective in managing chronic pain. It helps patients understand and change thought patterns that lead to harmful behaviors or distressing feelings, which can help break the cycle of pain.
- Lifestyle Changes:
Regular exercise, a healthy diet, sufficient sleep, stress management, and cessation of smoking and excessive alcohol consumption can all help manage pain and prevent it from becoming chronic.
- Patient Education:
Understanding the nature of pain, its causes, and management strategies can empower patients to take an active role in their treatment, which can lead to better outcomes.
- Surgical Intervention:
In certain cases, surgical intervention might be required to address the root cause of the pain and prevent it from becoming chronic.
It's important to remember that everyone is unique, and what works for one person may not work for another. Therefore, a multimodal, individualized approach to pain management is often the most effective. Always consult with a healthcare professional for the best course of action based on your specific circumstances.
Conclusion
Understanding the distinction between acute and chronic pain is crucial for adequate pain management and improving quality of life. It allows healthcare providers to customize treatment strategies and aids individuals in comprehending their symptoms.
While we have made significant strides in pain understanding and management, much remains to be explored. As we continue to delve into this complex subject, it's clear that a personalized, comprehensive approach is vital in treating acute and chronic pain.
About Dr. Sean Ormond



