Ever had that annoying pain right across your collarbone, making everything from reaching for your coffee cup to putting on a jacket feel like a struggle? You’re not alone. Clavicle pain can creep in at the most inconvenient times, and when it does, it’s hard to ignore.
It can manifest as a sharp ache or a dull throb, making even the simplest tasks feel like you’re carrying a suitcase full of bricks. Your clavicle, or collarbone, might not get the attention that other parts of your body do, but when it starts acting up, it demands attention.
This small but mighty bone connects your arm to the rest of your body, and when it's not functional, your entire upper body can feel off balance. So, why does this happen? What causes clavicle pain, and more importantly, what can you do about it?
The Anatomy Of The Clavicle
The clavicle, or collarbone, is a long, slender bone that connects your arm to the rest of your body. Its main job is to act as a support structure, keeping everything in alignment while allowing your arms and shoulders to move freely.
It also helps absorb shock to protect your body from impacts, like when taking a fall or playing a sport. But because of its exposed position, it’s more prone to injuries than other bones, making it a common site for fractures, stress, and strain.
When your clavicle is out of sorts, it doesn’t just affect your arm movement. Since the clavicle is attached to important muscles and ligaments, issues here can ripple out and cause discomfort in your shoulders, neck, and chest.
Common Causes of Clavicle Pain
The source of clavicle pain can, sometimes have an obvious answer—a sudden fall or awkward movement. Other times, the pain starts slowly and can be from a dramatic injury or more subtle wear and tear.
Your clavicle is a hardworking bone, and it takes a lot of hits throughout your day-to-day life. Between supporting your arm movements and absorbing impacts, it’s constantly working behind the scenes.
But just like any overworked part, things can start to break down or malfunction, and when they do, it’s important to know what’s going on.
1. Injuries
One of the biggest reasons for clavicle pain is injury—plain and simple. You might have taken a nasty fall or had an awkward landing while playing sports.
These cause fractures or dislocations, which are common issues that can lead to immediate and intense pain.
Fractures
Clavicle fractures are some of the most common injuries around this bone, often resulting from falls, sports, or accidents. Fractures usually happen in the middle of the clavicle and may leave you with a visible bump or even a “tenting” effect, where the bone pushes against the skin.
The pain from a fractured clavicle is typically intense, especially when moving your arm or shoulder. You may also notice bruising and swelling in the area.
Dislocations
While dislocations are often associated with shoulders, they can also involve the clavicle, especially where it meets the sternum (breastbone) or shoulder blade. Dislocations occur when these joints are forced out of alignment, often due to a sudden impact or fall.
With clavicle dislocations, the pain might feel deep and intense, especially when you try to move the shoulder. You may also notice swelling or an unusual shape in the affected area.
Sprains and Ligament Damage
Sprains happen when the ligaments around the clavicle—essentially the bone’s support ropes—get overstretched or torn. This can happen in accidents, falls, or even from lifting something too heavy.
Ligament injuries may not be as obvious as fractures or dislocations, but they can still cause persistent pain and make your shoulder feel weak or unstable.
2. Overuse and Stress
Sometimes, it’s not about one big accident but rather a series of small, repetitive motions that add up over time. Activities like lifting, throwing, or even typing can cause strain on your clavicle and the surrounding muscles.
The constant wear and tear can leave your collarbone feeling sore and tired, even if you can’t pinpoint a specific moment when the pain began.
Less Obvious Reasons You Might Be Hurting
Sometimes, clavicle pain can come out of nowhere, making you wonder if you slept funny or tweaked something you didn’t even know you had. While obvious injuries are often the first thing people think of, there are plenty of sneaky causes for that pain across your collarbone.
Pain isn’t always straightforward—it doesn’t always hit where the problem starts. Sometimes, it radiates from other parts of your body, or there’s an underlying condition you haven’t connected to your collarbone pain.
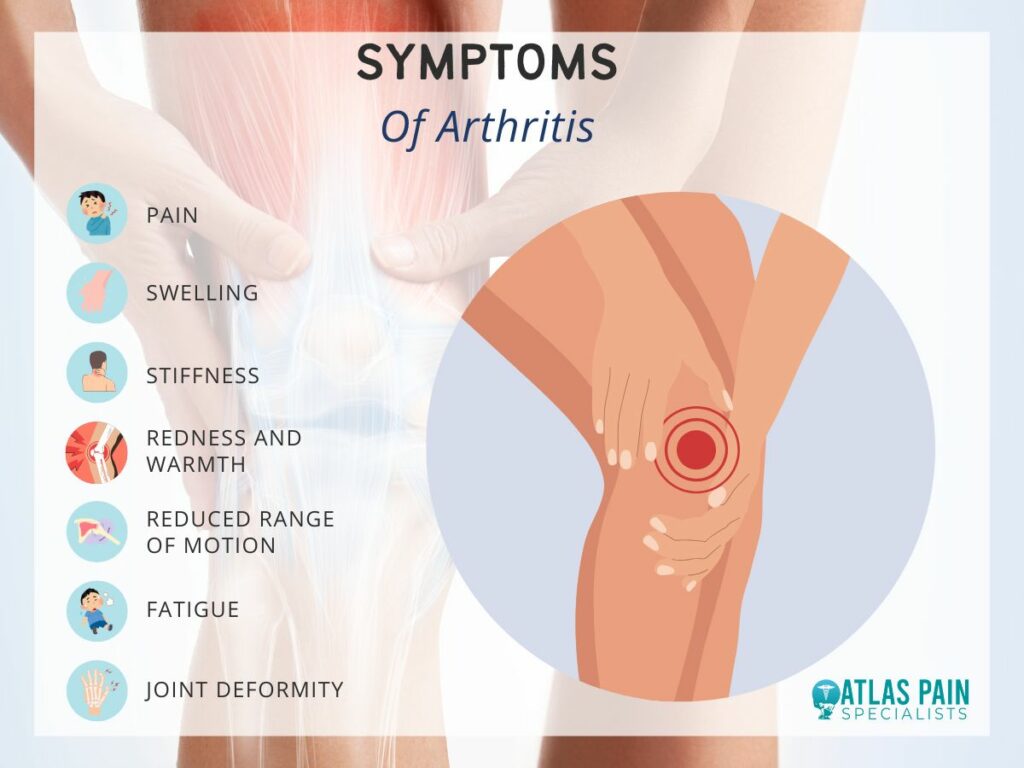
1. Arthritis
While you might think of arthritis as something that sticks to your knees or fingers, it can actually affect the clavicle and surrounding, joints too. Arthritis in the sternoclavicular or acromioclavicular joints can cause inflammation and stiffness, making your clavicle feel achy and sore.
This is one of those slow-burning causes where you notice the pain more over time rather than from a specific event.
2. Nerve Pain
Sometimes, clavicle pain has nothing to do with the bone itself but rather the nerves that run through the area. Issues like a pinched nerve in your neck or shoulder can send sharp pain shooting through your clavicle, tricking you into thinking the problem is in your collarbone.
Nerve-related pain can be especially tricky because it often feels worse when you move, but rest doesn’t seem to make it go away either.
3. Bone Infections and Rare Causes
Bone infections aren’t often the first thing that comes to mind when dealing with clavicle pain, but they do happen. When bacteria or fungi find their way into the bone, they can trigger a condition called osteomyelitis.
Infections like these often travel through the bloodstream or enter the body through an open wound, making certain people more susceptible, especially if they have weakened immune systems. With an infection, the pain can be persistent and often accompanied by other symptoms, such as warmth, redness, or even fever.
When Should You Worry About Clavicle Pain?
Let’s be honest—aches and pains are a normal part of life, especially if you’re active or even just getting through a tough day at work. But when clavicle pain starts to become more than a temporary nuisance, it’s worth paying attention.
It can be hard to know when to brush it off and when to take it seriously, but your body usually gives you a few clear signs when something’s not right. If your collarbone pain seems to be overstaying its welcome, it might be time to dig a little deeper.
So, how do you know when it’s time to get a second opinion or take action?
Minor vs. Serious Pain
If your clavicle pain is mild, comes and goes, and seems to get better with rest, it’s probably nothing to worry about. However, if the pain is sharp, persistent, or gets worse over time, it could be a sign of something more serious, like a fracture or joint issue.
Any pain that limits your movement feels intense with pressure or is accompanied by swelling should be checked out sooner rather than later.
Other Symptoms That Shouldn't Be Ignored
Clavicle pain that comes with other symptoms like numbness, tingling, or weakness in your arm or hand could point to nerve involvement or a more complex issue. If you notice any of these along with your collarbone pain, it’s a good idea to consult a healthcare professional.
If you’ve recently had a fall or trauma to the area and your pain hasn’t improved, it’s better to err on the side of caution and get it looked at.
What You Can Do at Home For Relief?
When clavicle pain strikes, the good news is that you can often manage it at home with a few simple strategies. While resting might sound like common advice, how you rest and the things you do around it can make a big difference in speeding up your recovery and reducing pain.
If you're looking for ways to feel better without making an extra trip to the doctor, there are some tried-and-true methods you can try from the comfort of your own space.
1. Rest and Ice
The first step is to take it easy on your clavicle. Rest is key, but it doesn’t mean doing absolutely nothing. Avoid movements that aggravate the pain, and give your shoulder and arm time to recover.
Applying ice to the sore area for 15-20 minutes every few hours can also help reduce inflammation and numb the pain. You might feel like a human popsicle for a while, but your clavicle will thank you.
2. Stretches and Exercises
While rest is important, keeping your shoulder completely immobile for too long can stiffen things up. Gentle stretches and movements can actually help relieve some of the tension around your clavicle.
Focus on slow, controlled exercises that don’t strain your shoulder but keep it flexible. This can help you maintain your range of motion while your body heals.
What to Do When Home Remedies Aren’t Enough
Sometimes, no matter how many ice packs or gentle stretches you try, the pain just won’t quit. It can be frustrating when home remedies don’t seem to be doing the trick, especially when you're doing everything right.
But don’t worry—it’s not a sign of failure. Sometimes, your clavicle pain might need a bit more attention, and that’s when turning to a professional can make all the difference.
There’s nothing wrong with reaching out for help when the pain refuses to back down. If your clavicle pain has persisted or worsened despite your best efforts, it’s a signal that something else might be going on under the surface.
Maybe it’s a deeper injury, or perhaps there’s an issue that can’t be resolved with at-home care alone.
1. Medical Treatments
When home remedies aren’t cutting it, a visit to your doctor can offer more specialized solutions. Depending on the cause of your clavicle pain, they might recommend physical therapy to strengthen and stabilize the area.
For more severe issues, such as a fracture or dislocation, treatments can range from bracing or slings to surgical intervention in extreme cases. The goal here is to provide relief and correct any underlying problems that at-home care just can’t fix.
2. Injections, Medications, and Other Options
In some cases, your doctor might suggest injections to help reduce inflammation and manage pain. Corticosteroid injections can offer quick relief, particularly if arthritis or another inflammatory condition is contributing to your discomfort.
Pain medications, both over-the-counter and prescription, can also play a role in managing the symptoms while you focus on healing. Whatever the case, your doctor will help tailor a plan that addresses your specific needs and helps you get back to feeling better.
Preventing and Managing Pain from Sports Injuries
Pain is a signal that something needs attention, be it an injury, overuse, or something less obvious. You can prevent your pain from disrupting your everyday life by understanding the root cause and giving yourself the right care.
One thing to keep in mind is how closely your clavicle pain can tie into sports injuries or other physical activities. Just like with any part of your body, preventing and managing pain from sports injuries goes hand in hand with maintaining a healthy clavicle.
When you’re active, especially in sports that involve your shoulders and arms, the risk of overuse or sudden injury increases. Strengthening the muscles around your clavicle and paying attention to proper form during physical activities can go a long way in keeping that pain at bay.
And if you do push things too far, knowing how to manage the aftermath with the right mix of rest, treatment, and care becomes essential.
Knee pain whether acute or chronic can make simple daily movements a huge task. This can be anything from hindering your morning jog to walking up or down the stairs.
Knowing where your knee pain is centered gives you an idea of what could have caused it. It can start acute acting only when triggered or chronic which means it's always there.
The knee is complex so pinpointing the exact location of the pain can set you on a good treatment plan or help you understand the cause. The nature of the pain can be unique so understanding these differences can bring some clarity to it. Let's delve into knee pain location chart explained.
Getting to Know Your Knee Pain
The anatomy of the knee is important when looking into what could be causing the pain. The knee does a lot more than just bend and straighten to help you move.
It is a complex amalgamation of bones, muscles, tendons and ligaments that work together to facilitate this bending and straightening. Each time you walk, squat, or twist, your knee is working to keep you steady, balanced, and mobile.
The Anatomy of The Knee
Knowing a bit about the structure of your knee can offer a clearer view of why pain might show up in one area rather than another. The knee’s anatomy includes four main components: bones, cartilage, ligaments, and tendons.
- The bones
The knee connects the thigh bone (femur) to the shin bone (tibia), with the kneecap (patella) offering added protection and support. The femur, tibia, and patella form the foundation, creating the structure that allows you to move with control and stability.
- Cartilage
The cartilage, a smooth, rubbery tissue, lines the surfaces where bones meet, allowing them to glide without grinding against each other. The menisci, two crescent-shaped pieces of cartilage between the bones, act like shock absorbers, reducing strain and helping you stay agile.
- Ligaments
Ligaments, which are like strong bands, keep everything stable. The ACL (anterior cruciate ligament) and PCL (posterior cruciate ligament) stabilize the knee by holding the bones together, preventing them from moving too far in one direction.
- Tendons
The tendons attach muscles to bones, helping the knee extend and flex. The largest of these, the patellar tendon, connects the kneecap to the tibia, playing an important role in supporting movements like jumping or climbing stairs.
Pain Above the Knee
Pain above the knee can often feel like an ache at first especially after an intense workout or a long day of physical activity. Most of the time it signals stress in the muscles and tendons that surround and support your knee.
- Quadriceps Tendonitis
Quadriceps tendonitis, also known as quadriceps tendinopathy, is an inflammation or degeneration of the tendon that connects the quadriceps muscles to the kneecap (patella). This pain develops from repetitive stress or overexertion in activities like running, jumping, or heavy lifting.
The condition can make the area feel tender and sore, especially when you press on it or try to bend the knee.
- Minor Tear Or Strain In The Quadriceps Muscle
When pain strikes above the knee, it usually involves the quadriceps muscles or the patellar tendon. The quadriceps, or "quads," are a group of four powerful muscles in the front of your thigh that help with straightening the knee and stabilizing your body when you move.
These muscles attach to the kneecap via the quadriceps tendon, which then continues as the patellar tendon, linking the kneecap to the shinbone. The strain can create a deep, aching sensation that feels especially intense when you move the knee.
- Misalignment Of The Knee Cap
Misalignment of the kneecap can stem from several factors, including muscle imbalances and physical activity. Weak quadriceps, tight hamstrings, or overuse from sports can pull the knee cap out of place.
Other causes might include structural irregularities or previous injuries, making some people more prone to this condition. If you’re noticing stiffness, swelling, or pain that persists beyond a few days, it might be time to consider a visit to a specialist.
Pain Below the Knee
Pain below the knee can also be frustrating, especially when it starts to interfere with daily activities or exercises you once enjoyed. This type of pain often centers around the patellar tendon, a critical connector that runs from your kneecap to your shinbone.
Pain below the knee can hint at issues with how the knee joint is handling movement and stress, and it may point to a specific condition that’s relatively common among active individuals.
- Patellar Tendonitis
The patellar tendon is important in supporting knee stability, like during activities that involve jumping, squatting, or bending. When this tendon is under too much strain, it can become inflamed—a condition often referred to as patellar tendonitis or "jumper’s knee."
People who engage in sports that require repetitive knee bending, such as basketball or volleyball, may be familiar with this type of pain. The pain can range from a dull ache to a sharp, stabbing sensation, noticeable when you're active or put weight on the knee.
- Osgood-Schlatter Disease
Osgood-Schlatter disease occurs when the tendon pulls on a growth plate at the top of the shinbone, causing inflammation and sometimes a bony bump. It is a condition more common in adolescents and young athletes.
Although this condition often improves with age, the pain can be intense, especially after physical activity, and may require rest and targeted exercises to relieve the discomfort.
- Patellar Tendon Degeneration
For adults, persistent pain below the knee can sometimes point to early stages of patellar tendon degeneration, known as patellar tendinopathy. This condition, unlike tendonitis, involves tiny tears in the tendon that don’t heal easily, resulting in chronic pain.
This condition develops when the tendon connecting the kneecap to the shinbone undergoes tiny tears and gradual wear, leading to pain, stiffness, and limited mobility. Over time, without proper management, the degeneration can become more severe, affecting daily activities and overall knee function.
Outer Knee Pain and Its Causes
Outer knee pain can begin as a mild annoying pain and build into a more persistent ache that limits your movement. It affects the lateral (outer) side of the knee, and is common among runners, cyclists, and anyone engaging in repetitive knee motion.
It might feel sharp and localized or present as a dull ache, especially after long periods of activity.
- Iliotibial (IT) Band Syndrome
This is one of the most common causes of pain in the outer knee. It occurs when the IT band—a thick band of fibrous tissue running from your hip to your knee—becomes tight or irritated.
The IT band crosses over the knee joint and, when inflamed, can cause sharp pain on the outer knee, especially noticeable during activities like running or descending stairs. IT band syndrome is often aggravated by overuse, muscle imbalances, or insufficient stretching, and it can become a nagging issue if not managed properly.
- Lateral Meniscus Tear
The meniscus is a C-shaped piece of cartilage that cushions and stabilizes your knee joint. When the lateral meniscus is torn you may feel pain on the outer knee along with symptoms like swelling, stiffness, or a catching sensation when you move.
It mostly occurs due to twisting motions or sudden changes in direction. The injury is common in sports that require quick pivots, such as soccer or basketball.
- Ligament Issues
The lateral collateral ligament (LCL), which provides stability to the outer knee, is one of the most affected by outer knee pain. Sprains or tears in the LCL are typically caused by trauma, such as a blow to the inner knee, and can lead to pain, swelling, and instability on the outer side.
Inner Knee Pain
Inner knee pain can impact basic activities like walking, bending, or even getting up from a chair. The pain, focused on the medial (inner) side of the knee, is a common complaint among people who lead active lives as well as those dealing with age-related joint changes.
Inner knee pain can arise from various causes, each pointing to different aspects of knee health that may need your attention.
- A Strain Or Injury To The MCL
One frequent source of inner knee pain is a strain or injury to the medial collateral ligament, which stabilizes the inner knee. The MCL can become overstretched or torn during sports or activities that involve sudden twisting motions or impact to the outer knee.
When the MCL is affected, you may feel a sharp, localized pain along with possible swelling or stiffness. Mild strains may heal on their own with rest, but more severe injuries can benefit from physical therapy to rebuild strength and stability in the knee.
- Medial Meniscus Tears
Medial meniscus tears are often seen in people who engage in high-impact activities or repetitive twisting motions. The meniscus acts as a shock absorber between the thigh bone and shinbone, and a tear can lead to pain, swelling, and sometimes a catching or locking sensation in the knee.
Meniscus injuries can vary in severity; some may improve with rest and gentle exercise, while others might require medical intervention for full recovery.
- Osteoarthritis In The Knee
Osteoarthritis in the knee can also present as inner knee pain, particularly as the cartilage wears down with age. This type of arthritis often brings a persistent ache or soreness on the inner knee, especially after prolonged activity or in cold weather.
Gentle movement, strength training, and targeted exercises can often help ease the discomfort and improve joint flexibility.
Pain Around the Knee Cap
Pain around your kneecap can be bothersome, making even simple tasks like climbing stairs or getting up from a chair feel challenging. Known as patellofemoral pain, this discomfort commonly affects people of all activity levels, from athletes to those with more sedentary routines.
Knee cap pain can be sharp or dull, and it often worsens with movements that put pressure on the knee, like squatting or jumping.
- Patellofemoral Pain Syndrome
This condition often stems from overuse, muscle imbalances, or improper alignment of the kneecap within the joint. When the kneecap doesn’t track smoothly, it can create friction against the femur (thigh bone), leading to inflammation and pain.
People with Patellofemoral pain syndrome may feel pain in the front of the knee, especially during activities that require bending or straightening the leg.
- Chondromalacia Patella
Chondromalacia patella is a condition where the cartilage under the kneecap softens and breaks down over time. This breakdown reduces the cartilage's ability to cushion the knee joint, causing discomfort when the knee bears weight.
Chondromalacia patella can affect people of various ages, though it’s more common in younger individuals who engage in high-impact sports or those with slight misalignment in the knee structure.
- Bursitis
Kneecap pain can also be linked to an inflammation of the small, fluid-filled sacs (bursae) around the knee that help reduce friction. Bursitis usually arises from prolonged kneeling or direct impact to the knee, causing swelling and pain around the kneecap.
It can be caused by an injury, repetitive stress, or joint alignment issues, addressing kneecap pain often involves a combination of rest, strengthening exercises, and possibly physical therapy.
Why Does My Knee Hurt When I Straighten It?
Knee pain can be frustrating, especially when it seems to limit your favorite activities or affect your day-to-day comfort. An understanding of where your pain is located can help you get the first step towards relief.
The knee is a powerful joint, yet it’s also vulnerable to wear and tear, strain, and injury. For many, knee pain is most noticeable during certain movements, like straightening the leg.
If you feel a sharp or persistent discomfort when straightening your knee, it can be a sign of issues related to alignment, overuse, or even the cartilage within the joint. This type of pain often overlaps with the topics we’ve explored, as it’s another way your knee responds to strain or structural imbalance.
The belief that cracking your back can lead to arthritis is a common myth that lacks scientific support. Many people enjoy the relief that comes from this action, often attributed to the release of gas from joints rather than any structural damage. While occasional cracking may not pose significant risks, it’s essential to be mindful of underlying conditions that could be aggravated by this habit.
Understanding the truth behind back cracking can help alleviate concerns and promote healthier practices for spinal care.
Understanding Back Cracking
Back cracking is something many people experience, either intentionally during stretches or unintentionally during daily movements. The sound it makes can be satisfying, but it also leads to questions about what’s happening in the body when it occurs. More importantly, some people worry that frequent back cracking can cause long-term problems like arthritis. Let’s break down the truth behind back-cracking and separate the myths from the facts.
So what Causes the Cracking Sound? The cracking sound you hear when you twist or stretch your back is not bones grinding against each other. Instead, it’s the release of gas bubbles in the fluid that surrounds your joints. This fluid, known as synovial fluid, acts as a lubricant, helping your joints move smoothly. When you stretch or apply pressure to a joint, the gas in the synovial fluid can be released, causing that familiar popping sound. It’s a completely normal occurrence and happens with many joints in the body, not just your back.
Is Cracking Your Back Safe? In general, occasional back cracking is considered safe, especially when it happens naturally as you stretch or move. However, forcing your back to crack or doing it excessively can potentially cause strain. It’s important to listen to your body and avoid putting too much pressure on your joints. If you’re constantly needing to crack your back to relieve discomfort, it may be a sign of an underlying issue that needs professional attention.
Myths Surrounding Back Cracking
Back cracking is often surrounded by myths that can lead to misconceptions about its effects on joint health. Understanding the truths behind these myths can help clarify the impact of back cracking on the body.
Myth 1: Back Cracking Causes Arthritis
One of the most common myths about back cracking is that it leads to arthritis. However, there’s no scientific evidence to support this claim. Cracking your back does not cause arthritis, and the sound has no connection to joint damage. Arthritis is a condition that involves inflammation of the joints, often caused by factors like genetics, injury, or wear and tear over time—not by cracking.
Myth 2: Cracking Joints Means Something Is Wrong
People sometimes associate cracking sounds with injury or joint problems, but this isn’t the case. As mentioned earlier, the sound is simply gas escaping from the joint fluid. Unless cracking is accompanied by pain or swelling, it’s generally nothing to worry about. In fact, many people experience joint cracking without any discomfort or negative effects.
Myth 3: Back Cracking Leads to Permanent Damage
Some believe that frequently cracking your back will lead to long-term damage or misalignment of the spine. While excessive back cracking could potentially cause strain if done incorrectly, the occasional, natural cracking that happens during movement is harmless. The key is moderation and avoiding putting too much force on your joints.
When Should You Be Concerned?
While occasional back cracking is normal, there are times when you should pay closer attention. If you experience pain, swelling, or a limited range of motion along with cracking, it could be a sign of a more serious issue. In these cases, it’s a good idea to consult a healthcare professional, such as a chiropractor or physical therapist. They can assess your condition and provide appropriate guidance.
If you’re worried about back discomfort or cracking, there are simple ways to maintain good back health. Regular exercise, stretching, and maintaining proper posture can go a long way in keeping your spine and joints in good shape.
Potential Risks of Cracking Your Back
While the occasional back crack is not harmful, there are potential risks if back cracking becomes a habit or is done incorrectly. Forcing your back to crack or doing it too often could lead to strain or even injury over time. If you’re constantly cracking your back to relieve discomfort, it could signal a deeper issue that requires attention.
- Overstretching and Strain: One of the risks of habitual back cracking is overstretching your muscles and ligaments. When you crack your back repeatedly, you may begin to rely on this action for temporary relief, but it doesn’t address the underlying cause of stiffness or discomfort. Over time, this can lead to strain in the muscles and ligaments around your spine.
- Risk of Misalignment: Another potential issue is spinal misalignment. If you’re using improper techniques to crack your back, especially if you’re applying too much force, you might risk shifting your spine out of its natural alignment. This can lead to pain and discomfort in the long run. If you feel the need to crack your back frequently, it’s a good idea to consult a healthcare professional, such as a chiropractor, who can assess your spinal health and provide safe techniques for relief.
Benefits of Professional Chiropractic Care
Cracking your back can feel satisfying, but it’s often a temporary solution that doesn’t address the root cause of discomfort. If you're dealing with frequent back pain or stiffness, professional chiropractic care offers a better, more effective long-term solution.
Chiropractic care focuses on improving the health of your spine and joints, providing relief, and preventing future issues. Here, we’ll explore the benefits of chiropractic care and why it might be a better option than self-cracking your back.
Natural and Non-Invasive Pain Relief
One of the most significant benefits of chiropractic care is that it offers natural, non-invasive pain relief. Chiropractors use manual adjustments to realign the spine and relieve pressure on nerves, muscles, and joints. This approach treats the root cause of pain rather than just masking the symptoms with medication. Chiropractic adjustments help improve the body’s overall function, reduce pain, and promote healing without the need for surgery or drugs.
Improved Flexibility and Mobility
Chiropractic care also improves your body’s flexibility and mobility by addressing misalignments in the spine and joints. When your spine is properly aligned, your range of motion increases, allowing you to move more freely.
This can be particularly beneficial for people who experience stiffness, limited mobility, or discomfort while performing everyday tasks. If you’re recovering from an injury or simply dealing with age-related wear and tear, chiropractic care can help restore flexibility and make it easier to stay active.
Preventative Care for Long-Term Health
Chiropractic care isn’t just about treating pain—it's also about preventing future problems. Regular chiropractic visits can help detect and correct spinal misalignments before they lead to more serious issues. Chiropractors also provide guidance on exercises, stretches, and lifestyle adjustments that support your spine health and overall wellness. This holistic approach can reduce the risk of injury, improve posture, and enhance your quality of life.
By addressing potential issues early, chiropractic care helps you avoid the need for more invasive treatments later on. It’s a proactive way to maintain your health and prevent chronic pain from becoming a problem.
Pain Management for Arthritis Sufferers
While cracking your back does not cause arthritis, it can provide temporary relief from discomfort. However, for those already suffering from arthritis, managing pain effectively is crucial. As we transition to our next topic on pain management for arthritis sufferers, it's essential to explore various strategies and treatments available.
Understanding these options can empower individuals to alleviate their symptoms and improve their quality of life, ensuring they can engage in daily activities with greater ease and comfort.
When to Seek Medical Advice
While chiropractic care can be an excellent option for many people, there are times when you should seek medical advice before continuing or starting treatment. If you’re experiencing severe or persistent pain, numbness, tingling, or weakness, it’s essential to consult a doctor. These symptoms could indicate a more serious condition, such as a herniated disc or nerve damage, that may require additional medical attention.
Your chiropractor will work with you to determine the best course of action, and if necessary, they may refer you to a specialist for further evaluation and treatment.
Alternatives to Cracking Your Back
If you often crack your back to relieve discomfort, it’s important to know that there are healthier alternatives that can provide longer-lasting relief. Stretching exercises, yoga, and low-impact activities like swimming or walking can help keep your back flexible and reduce tension. These activities not only relieve stiffness but also promote better posture and overall spine health.
Chiropractic care is another excellent alternative to self-cracking. Regular adjustments ensure that your spine is properly aligned, reducing the need to crack your back. This approach provides relief without the risk of strain or injury that can occur when you force your back to crack.
Experiencing knee pain when straightening your leg can be both frustrating and concerning. This discomfort may arise from various underlying issues, ranging from minor injuries to more serious conditions like arthritis or ligament damage.
Understanding the potential causes is crucial for effective management and treatment. Whether it's a result of overuse, inflammation, or structural damage, recognizing the symptoms associated with this pain can help you seek appropriate care and regain mobility. Let’s delve into the common reasons behind this painful experience and explore possible solutions.
Common Causes of Knee Pain When Straightening
Knee pain can be frustrating, especially when it limits your ability to move freely. If you’ve noticed pain when straightening your knee, you’re not alone. There are several common causes of knee pain that may be responsible for the discomfort.
- One of the most frequent causes is patellar tendonitis, often seen in athletes or individuals who put a lot of strain on their knees. This condition occurs when the patellar tendon becomes inflamed from overuse.
- Another common cause is osteoarthritis, which is characterized by the breakdown of cartilage in the knee, leading to stiffness and pain.
- Meniscus tears are also common, particularly after a sudden twisting movement. The meniscus is a piece of cartilage that helps cushion your knee joint, and a tear can cause sharp pain when you straighten your leg.
- Runner’s knee (patellofemoral pain syndrome) is another culprit, usually caused by misalignment of the kneecap, leading to discomfort when bending or straightening the knee.
Symptoms to Watch For
If you’re experiencing knee pain when straightening your leg, it's important to pay attention to the accompanying symptoms.
- Swelling around the knee joint is a clear indication that something may be wrong. Whether it’s inflammation or fluid buildup, swelling often points to an underlying issue that needs attention.
- Another symptom to watch for is a popping or clicking sound when you move your knee. This could signal a torn meniscus or ligament injury. If you experience sharp, stabbing pain in the knee, especially when trying to stand up or fully extend the leg, you may be dealing with a more serious condition like a ligament injury.
- Limited range of motion is also a symptom you shouldn’t ignore. If it becomes difficult to straighten your leg completely or bend it without pain, this could point to conditions like arthritis or a torn meniscus.
When to Seek Medical Attention
Knee pain is a common issue that most people will experience at some point, but not all cases require immediate medical attention. Understanding when to consult a healthcare professional can prevent more serious conditions from developing.

Swelling and Redness
If your knee is noticeably swollen or red, it may indicate a more serious underlying issue, such as a ligament tear, arthritis flare-up, or an infection. Swelling that does not subside after a day or two of rest and ice should be evaluated by a doctor.
Difficulty Bearing Weight
Struggling to stand or walk without pain is a clear sign that you need medical attention. The inability to bear weight could mean a severe ligament injury or fracture that requires immediate intervention. Ignoring this sign can worsen the injury and prolong recovery time.
Knee Instability
Experiencing instability, or the feeling that your knee might "give out," is often associated with ligament damage, such as an ACL or MCL tear. Knee instability can also lead to further injuries if left untreated, so seeing a doctor early can prevent long-term damage.
Locking or Catching Sensation
If your knee locks up or feels as if it's catching when you move, this could be due to a meniscus tear or another cartilage problem. These conditions often require prompt medical attention, as they may worsen without proper treatment. If your knee is locking or catching, it may indicate a meniscus tear or other cartilage problem that requires prompt medical attention.
Persistent Pain
Any knee pain that lasts longer than a few days, especially after rest and home care, should be checked by a healthcare provider. Chronic pain could be a sign of conditions like osteoarthritis or bursitis, which can progress if not properly managed.
Diagnostic Approaches
Once you’ve decided to visit a healthcare provider, understanding the diagnostic approaches they might use can help ease any uncertainty.
The first step in diagnosis is often a physical examination, where your doctor will assess your knee’s range of motion, stability, and areas of tenderness.
In many cases, imaging tests are necessary to get a clearer picture of what’s happening inside the knee. X-rays can show if there’s any bone damage, while MRI scans provide detailed images of soft tissues, including cartilage, ligaments, and tendons. Ultrasound is another option your doctor might use, especially to see how the soft tissues move as the knee bends and straightens.
Sometimes, blood tests are ordered to rule out conditions like gout or rheumatoid arthritis, which can also cause knee pain. If your doctor suspects fluid buildup, they may also perform joint aspiration, a procedure where fluid is drawn from the knee for analysis.
Treatment Options
If you’re experiencing knee pain, understanding your treatment options is crucial for effective recovery. The right approach depends on the underlying cause of your pain, so seeking medical advice is the first step. However, many treatments for knee pain are straightforward and focus on reducing discomfort while promoting healing.
One common approach is rest, ice, compression, and elevation (RICE). This method can help reduce swelling and pain, especially for minor injuries like sprains or strains. Over-the-counter anti-inflammatory medications like ibuprofen are also frequently recommended to manage pain and inflammation.
For more serious conditions, such as ligament tears or osteoarthritis, physical therapy is often suggested. Physical therapy strengthens the muscles around the knee, improving stability and reducing strain on the joint. In some cases, corticosteroid injections are used to manage inflammation in more severe cases.
Surgical options may be necessary if conservative treatments don’t provide relief. For example, a torn meniscus or ACL tear often requires surgical intervention to restore proper knee function. Knee replacement surgery is typically reserved for severe arthritis cases where the joint is significantly damaged.
Preventive Measures
Taking care of your knees before an injury happens is just as important as treating existing pain. Strengthening exercises that focus on the muscles around the knee—such as the quadriceps and hamstrings—are one of the best ways to prevent knee problems. These exercises help provide support to the knee joint and reduce the risk of injury.
Maintaining a healthy weight is another important preventive measure. Excess weight adds strain to your knee joints, which can accelerate wear and tear. By keeping your weight in a healthy range, you can alleviate unnecessary pressure on your knees.
Wearing proper footwear is also key to protecting your knees. Shoes with good arch support and cushioning can absorb shock, preventing excessive stress on your knees during physical activity.
Be mindful of your movements. Avoid sudden twists or overextension of the knee, especially during sports or physical activity. Warming up before exercise and stretching afterward can go a long way in preventing knee injuries.
Stabbing Or Sharp Knee Pain That Comes and Goes
As we explored the reasons behind knee pain when straightening, it's crucial to understand that persistent discomfort can signal underlying issues. If you're experiencing sharp, stabbing pain that comes and goes, it may be indicative of conditions such as a cartilage tear or arthritis. These intermittent pains can arise from various factors, including overuse or injury, and recognizing their patterns is essential for effective treatment.
For a deeper dive into the causes and management of this specific type of knee pain, stay tuned as we transition into discussing the nuances of sharp knee pain that fluctuates in intensity.
Deadlifting is a powerful exercise that builds strength and enhances athletic performance, but it can also lead to lower back pain if not performed correctly. This article explores the common causes of lower back pain from deadlifting, such as poor technique, weak supporting muscles, and overtraining. It highlights the importance of maintaining proper form and strengthening key muscle groups to prevent injury.
Additionally, the article provides practical recovery strategies to manage pain and guide a safe return to lifting. It also explains when it’s essential to seek medical attention for persistent or severe back issues, ensuring a comprehensive approach to avoiding and recovering from lower back pain related to deadlifting.
Causes of Lower Back Pain from Deadlifting
Lower back pain from deadlifting can be caused by several factors, often related to improper form, technique, or inadequate conditioning. Here are some of the primary causes:
1. Poor Lifting Form
Rounding your lower back during a deadlift puts excessive stress on your spine, especially the lumbar region. This can lead to muscle strains, disc injuries, or even herniation over time.
2. Weak Core Muscles
A weak core means your abdominal muscles aren't able to stabilize your spine properly during the lift. This forces your lower back to overcompensate, placing extra strain on the muscles and ligaments.
3. Insufficient Mobility
Limited flexibility in the hamstrings, hips, or upper back restricts your range of motion. This forces your lower back to do more work, increasing the risk of muscle fatigue, pain, or injury.
4. Overtraining or Lifting Too Heavy
Lifting too much weight too soon or not allowing enough recovery between sessions can overload your lower back muscles. This strain can lead to injuries like muscle pulls or disc issues.
5. Inadequate Warm-Up
Not warming up properly before deadlifting leaves your muscles stiff and unprepared for heavy lifting. This increases the risk of straining or overloading your lower back muscles during the exercise.
6. Muscle Imbalances
When your glutes and hamstrings are weak or underdeveloped, your lower back has to take on more of the lifting load. This imbalance causes extra stress on the lumbar region, which can lead to pain or injury.
7. Pre-existing Conditions
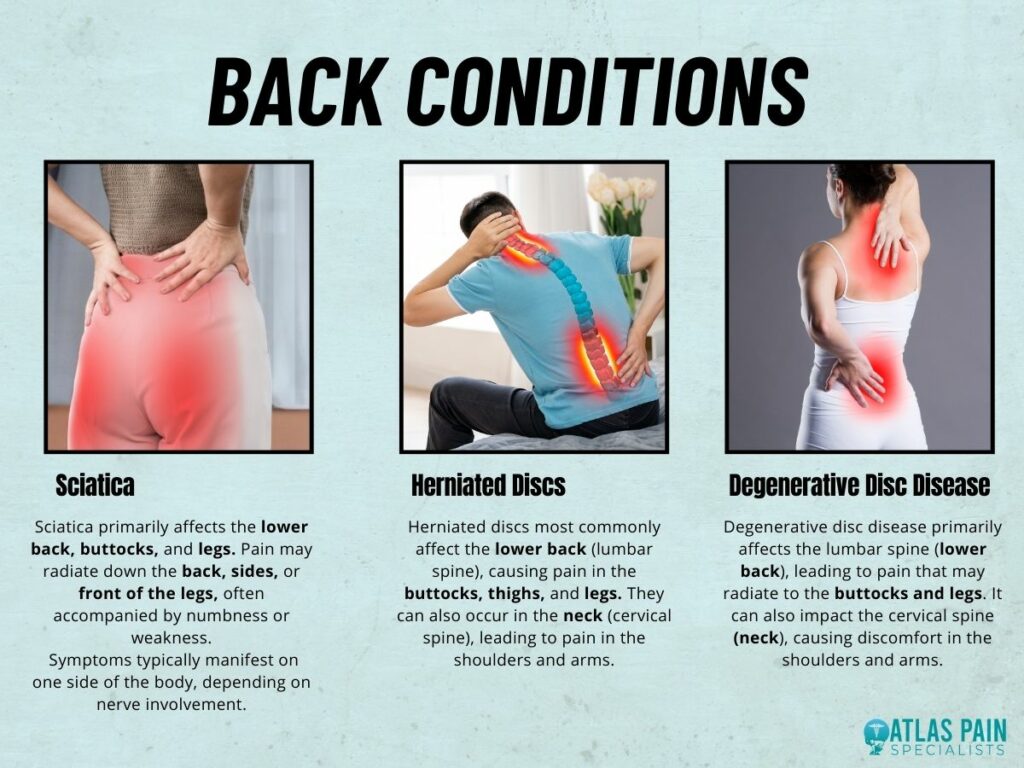
If you have pre-existing back conditions like herniated discs, sciatica, or degenerative disc disease, deadlifting can aggravate these issues. These conditions often cause chronic pain, which can worsen with improper lifting.
8. Poor Recovery or Insufficient Rest
Lack of proper rest between deadlifting sessions doesn’t give your muscles time to recover and repair. This can lead to fatigue, compromised form, and increased stress on the lower back, raising the risk of injury.
To avoid lower back pain, focus on using good form, strengthening your core, stretching regularly, and not pushing your body too hard too soon. Proper recovery and rest are just as important as the lifts themselves.
Prevention of Lower Back Pain from Deadlifting
Preventing lower back pain from deadlifting mostly comes down to a combination of good technique, proper preparation, and smart training habits. Here are some key ways to avoid injury and keep your lower back healthy:
1. Master Proper Form
Keep a neutral spine and avoid rounding your lower back during the lift to reduce strain on your spine. Engage your core and ensure the bar stays close to your body throughout the movement.
2. Strengthen Your Core
A strong core helps stabilize your spine and prevents overloading the lower back. Incorporate exercises like planks and leg raises to build abdominal strength and support your lifting form.
3. Build Up Your Posterior Chain
Focus on strengthening your glutes, hamstrings, and lower back to take pressure off your spine. Exercises like Romanian deadlifts and glute bridges can help develop these muscles.
4. Work on Flexibility and Mobility
Improving flexibility in your hamstrings, hips, and upper back allows for better movement and reduces stress on your lower back. Regular stretching and foam rolling can improve mobility and prevent injury.
5. Warm Up Properly
Always start with a dynamic warm-up to increase blood flow and prepare your muscles for the lift. Incorporate leg swings, bodyweight squats, and light cardio to loosen up your muscles before lifting.
6. Start Light and Progress Gradually
Begin with lighter weights to perfect your technique before increasing the load. Gradually add weight as your strength improves, ensuring your form stays, solid and your muscles adapt.
7. Listen to Your Body
Pay attention to any discomfort or pain during and after deadlifts, and adjust your form or the weight you're lifting. Don’t push through pain, as it can lead to more serious injuries.
8. Get Adequate Rest and Recovery
Allow your muscles to recover fully between lifting sessions to avoid fatigue and muscle strain. Prioritize sleep, rest days, and proper nutrition to support muscle repair and growth.
By focusing on form, building strength where it counts, and being mindful of your body's limits, you can avoid lower back pain and deadlift safely for the long term.
Recovery from Lower Back Pain Caused by Deadlifting
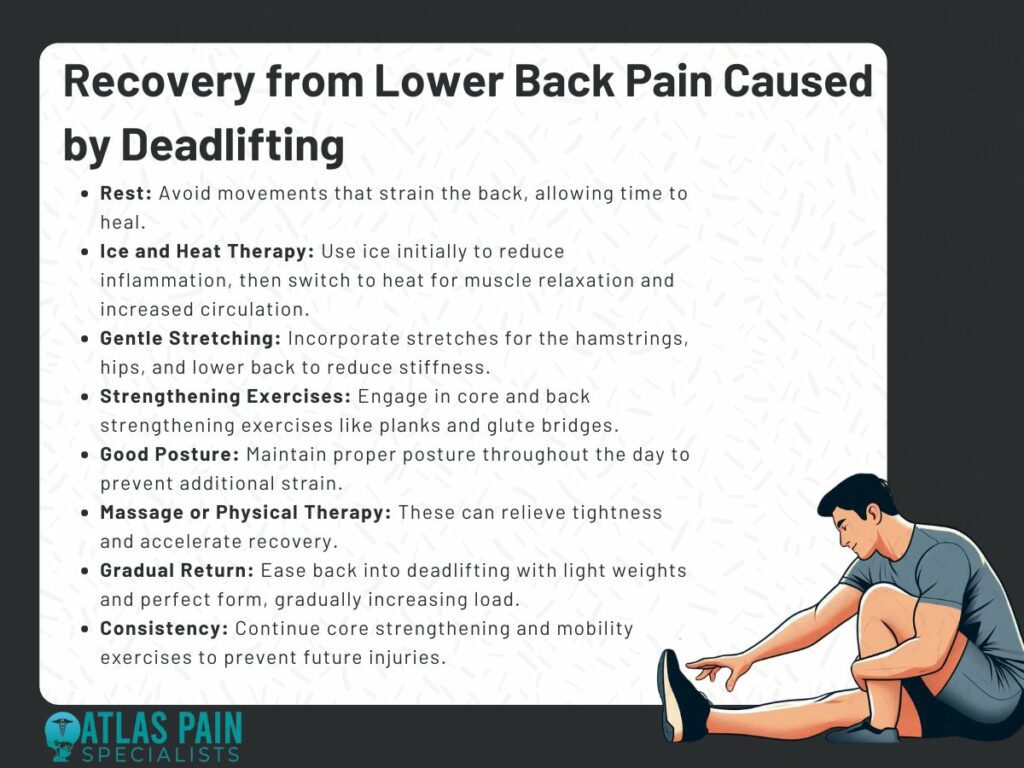
Recovering from lower back pain caused by deadlifting requires a combination of rest, rehabilitation exercises, and a gradual return to lifting. Here's a step-by-step approach to help you recover and prevent future issues:
1. Rest and Avoid Aggravating Movements
Give your lower back time to heal by avoiding heavy lifting or exercises that strain the area. Gentle movement, like walking, can help maintain circulation without worsening the pain.
2. Ice and Heat Therapy
Apply ice in the first 48 hours to reduce inflammation, then switch to heat to relax muscles and increase blood flow. Both can help alleviate pain and promote healing.
3. Gentle Stretching and Mobility Work
Once the pain subsides, incorporate gentle stretches to improve flexibility and reduce muscle tightness. Focus on stretches for the hamstrings, hips, and lower back to avoid stiffness.
4. Strengthening Exercises for Core and Back
Start strengthening your core and back muscles with low-impact exercises like bird dogs, planks, and glute bridges. These exercises support the spine and help prevent future injuries.
5. Use Proper Posture and Ergonomics
Maintain good posture throughout the day to avoid putting additional strain on your lower back. Proper sitting and standing habits help support recovery and reduce pain.
6. Massage or Physical Therapy
Massage can relieve muscle tightness, while physical therapy can provide specific exercises for strengthening and mobility. Both help accelerate recovery and reduce the risk of re-injury.
7. Gradual Return to Deadlifting
Ease back into deadlifting with lighter weights and perfect form, focusing on maintaining a neutral spine. Gradually increase the load as your back strengthens and the pain resolves.
8. Stay Consistent with Core and Mobility Work
Continue to strengthen your core and improve flexibility even after recovering to prevent future injuries. Regular core and mobility exercises will keep your back strong and flexible for lifting.
By giving yourself time to heal, strengthening the right muscles, and returning to deadlifting gradually, you’ll be able to recover effectively and reduce the risk of future lower back pain.
When to Seek Medical Attention
While most cases of lower back pain from deadlifting can be managed with rest and rehab, there are times when you should seek medical attention. Here are the key signs that it's time to consult a doctor or specialist:
1. Severe or Persistent Pain
If the pain is sharp, intense, or doesn’t improve after a few days of rest and treatment, it may be a sign of a serious injury. Ongoing or worsening pain requires professional evaluation.
2. Radiating Pain (Sciatica)
Pain that travels down your leg, accompanied by tingling, numbness, or weakness, may indicate nerve involvement, like a herniated disc. This requires medical attention to avoid long-term damage.
3. Loss of Function
If you’re struggling to stand, walk, or perform basic movements due to pain, it’s a sign that your injury may be more severe. Loss of function often means you need immediate medical help.
4. Weakness in the Legs or Feet
If you experience leg weakness or difficulty controlling foot movements, it could indicate nerve compression. This is a concerning sign and should be evaluated by a healthcare professional.
5. Bladder or Bowel Dysfunction
Incontinence or loss of control over bladder or bowel function is a medical emergency. These symptoms may indicate cauda equina syndrome, which requires immediate intervention.
6. Increased Pain with Coughing, Sneezing, or Bending
Pain that intensifies when coughing, sneezing, or bending forward can indicate disc problems or nerve irritation. Seek medical advice if this pain persists or worsens.
7. Pain After a Fall or Trauma
If the pain started after a fall, accident, or heavy lift, it may indicate a fracture or more serious injury. You should consult a doctor to rule out structural damage.
8. Pain with Fever or Unexplained Weight Loss
Pain accompanied by fever, unexplained weight loss, or night pain suggests an infection or other serious condition. This requires urgent medical evaluation.
9. No Improvement After Several Weeks
If your lower back pain doesn’t improve after 4-6 weeks of consistent care (rest, stretching, strengthening exercises), it's worth seeking professional evaluation. This could indicate an underlying issue that needs more specific treatment.
In these situations, it’s always better to err on the side of caution and get checked by a healthcare professional. They can provide a proper diagnosis and recommend a treatment plan tailored to your condition.
Conclusion
This article covers the causes, prevention, and recovery of lower back pain from deadlifting. It identifies common causes such as poor form, weak supporting muscles, overtraining, and mobility issues. To prevent injury, it emphasizes the importance of proper technique, strengthening key muscle groups, and gradually increasing weight.
For recovery, the article suggests rest, stretching, mobility exercises, and core strengthening. It also highlights when to seek medical attention for severe or persistent pain, ensuring a balanced approach to avoiding and addressing back issues related to deadlifting.
Arm pain has a sneaky way of creeping up on you when you least expect it. One moment, you're reaching for the remote, and the next, it feels like your arm's been through a round with a professional wrestler.
But before you panic and start imagining the worst, know that most arm pain has pretty straightforward causes — and thankfully, a lot of them can be managed. Maybe it's the after-effects of hauling groceries up the stairs, or perhaps it’s that weird angle you slept in last night.
Sometimes, the reason is obvious, but other times, arm pain just seems to show up uninvited like a party crasher you didn’t plan for. The good news is, you’re not alone — most of us deal with arm pain at some point, and figuring out what’s behind it is the first step toward relief.
What Could Be Behind Arm Pain?
It’s easy to assume that a bit of arm soreness will pass, but when the pain sticks around, it’s natural to start wondering what’s really going on. Your arms are crucial for pretty much everything—whether you’re lifting, typing, or just scrolling through your phone—and when something feels off, it’s hard to ignore.
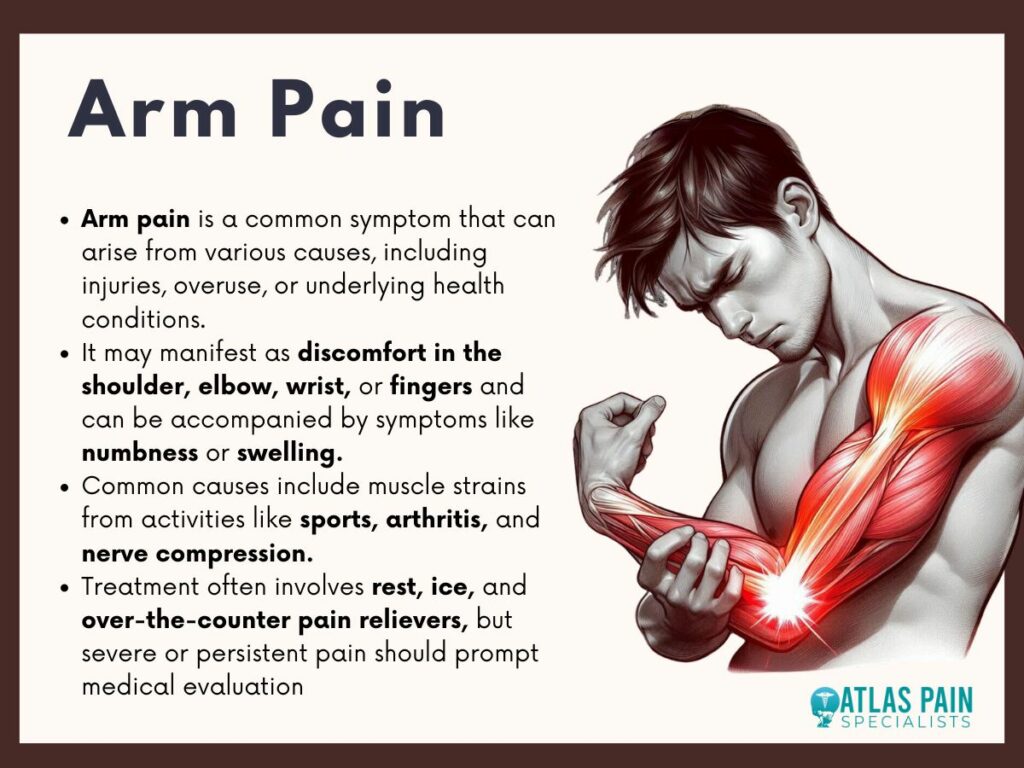
There are many potential reasons for arm discomfort, and while some are more common than others, each has its own unique set of factors. And, let’s face it—ignoring arm pain in hopes that it’ll magically disappear often doesn’t work out too well.
Why Arm Pain Happens to So Many People
When you think about it, your arms are like the all-stars of your body, always moving and getting things done. So, when they start hurting, it makes sense that they might need a break.
Everyday actions—like carrying heavy bags or spending hours in front of a computer—can take their toll. If your muscles, tendons, and joints don’t get a chance to rest or stretch, they could start to rebel with soreness or stiffness. You might not even realize how much you rely on your arms until you’re struggling to pour yourself a glass of water without wincing.
Is Your Arm Pain Something Serious?
It’s easy to downplay arm pain as something minor, but sometimes, it’s a sign that something more serious is going on. Pain that lingers, gets worse, or comes with other symptoms shouldn’t be brushed off.
Sure, your arm might just be sore from overuse, but if there’s swelling, numbness, or tingling involved, it might be time to take a closer look. Your arms do a lot of important work, and when they start sending you signals that something’s not right, it’s worth paying attention.
After all, there’s no harm in being cautious, especially when it comes to something as important as your mobility and overall comfort.
Everyday Causes of Arm Pain You Might Overlook
Arm pain doesn’t always come from some dramatic injury or major health issue. It’s easy to overlook how much strain your arms endure daily until they start giving you trouble.
When arm pain shows up unexpectedly, it can be tempting to chalk it up to “just getting older” or “being out of shape.” But more often than not, it’s not about age or fitness. The reality is, even everyday activities can lead to discomfort if your muscles, tendons, and joints are overworked or out of alignment.
If you’ve been wondering why your arm is bothering you, the answer might lie in something you do without even realizing it.
1. Repetitive Movements
Think about how often you do the same thing over and over again—whether it’s typing at work, scrolling through your phone, or carrying heavy bags. Your arms are on the job all day, repeating the same motions, and over time, that can lead to soreness or even injury.
Repetitive strain injuries (RSIs) happen when you put too much stress on certain muscles or tendons without giving them a chance to recover. It’s like when you overuse a tool—it starts to wear down, and your arms are no different.
Even hobbies like knitting, playing an instrument, or working out can contribute to arm pain if you’re not careful. The key is to take breaks, switch things up, and give your arms a chance to recover from the constant motion they endure.
2. Strains and Sprains
Sometimes, arm pain comes from a small injury that you might not even remember. Maybe you twisted your arm the wrong way while lifting something or reached too far during a workout.
Strains and sprains are common, and they can happen when you least expect it. A muscle strain occurs when you overstretch or tear the fibers in your muscles, while a sprain happens when you injure the ligaments that support your joints.
Both can cause pain, swelling, and tenderness, making it hard to use your arm normally. The thing about strains and sprains is that they don’t always feel like a big deal at first.
4. Bad Posture
Believe it or not, the way you sit and stand can have a big impact on your arms. If you’re slouching at your desk, hunching over your phone, or constantly reaching forward to grab things, your posture could be putting unnecessary strain on your arms.
Over time, bad posture can lead to muscle imbalances that cause discomfort in your neck, shoulders, and arms. It’s easy to overlook, but something as simple as adjusting your posture can make a big difference in how your arms feel at the end of the day.
When you maintain good posture—whether you’re sitting, standing, or even walking—you take the pressure off your arms and allow your muscles to work more efficiently. So, next time your arm starts to feel sore, take a moment to check your posture.
Medical Conditions That Could Be Causing Your Arm Pain
Sometimes, arm pain isn’t just a result of overdoing it at the gym or spending too much time on your phone. It might be pointing to a deeper issue that requires a bit more attention.
When the pain doesn’t seem to go away with rest or home remedies, it’s natural to wonder if something else is going on. It’s important to be aware of the potential medical conditions that could be at the root of your discomfort.
Conditions involving inflammation, nerve compression, or even issues with your circulatory system can all lead to arm pain that feels confusing or out of place.
1. Tendonitis
If you’ve ever experienced a nagging pain that seems to flare up when you move your arm a certain way, tendonitis could be to blame. This condition happens when the tendons in your arm become inflamed, often due to overuse or repetitive motions.
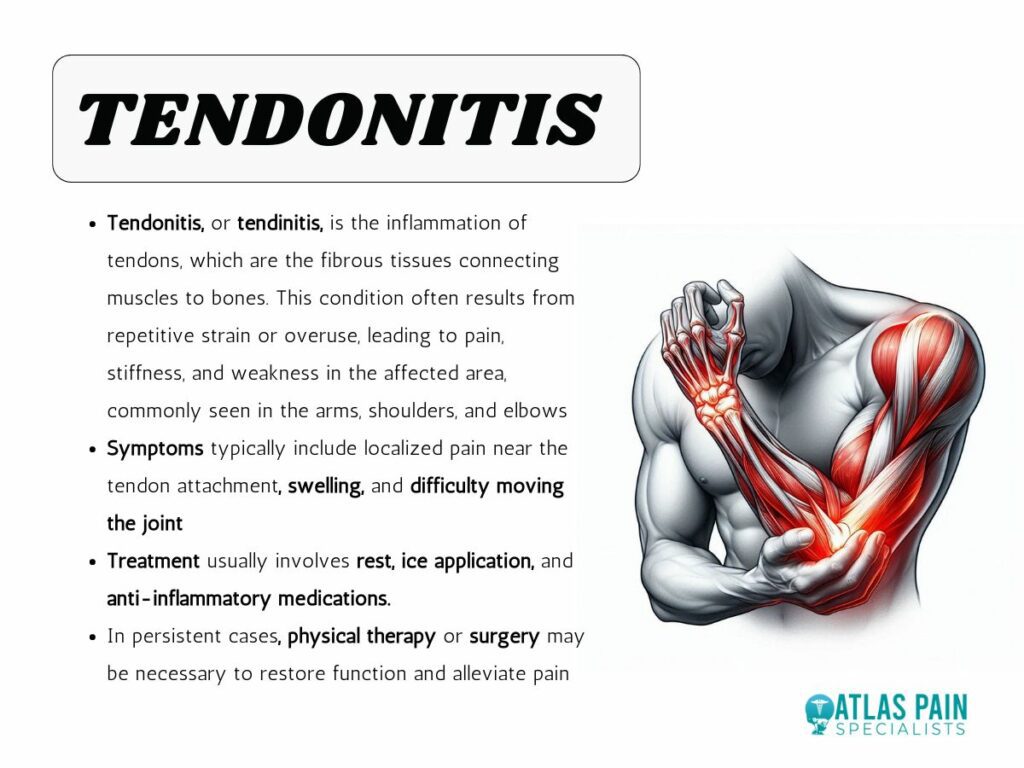
Tendonitis is common in the elbow (commonly known as tennis elbow) or shoulder, and while it can start as a minor annoyance, it can get worse over time if left untreated. It’s like when a rubber band gets stretched out too many times—it loses its flexibility and starts to fray.
The good news is that tendonitis can usually be managed with rest, physical therapy, and adjustments to how you use your arm.
2. Bursitis
Bursae are small, fluid-filled sacs that act as cushions between your bones, muscles, and tendons. When these bursae become inflamed—usually from repetitive movement or pressure—it leads to bursitis, which can cause pain in your arm, particularly in the shoulder or elbow.
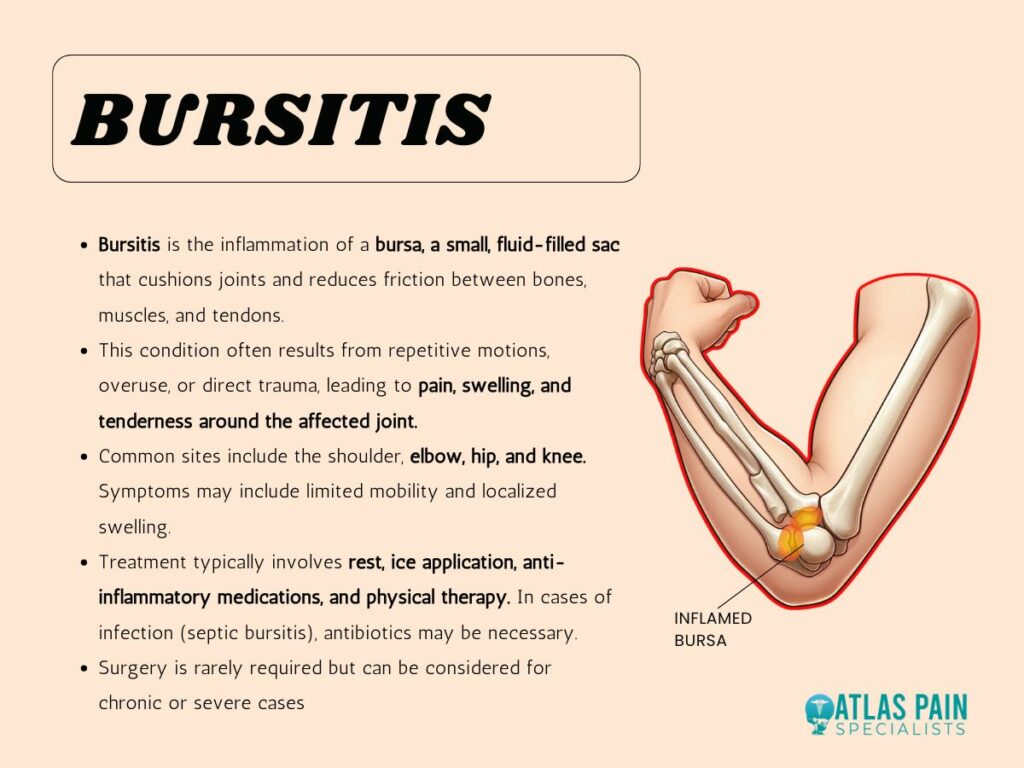
Bursitis often gets mistaken for other issues because the pain can feel similar to a sprain or strain, but it’s the inflammation of these tiny sacs that’s actually causing the discomfort. It can make simple activities like lifting your arm or carrying groceries feel much harder than they should be.
The pain may also flare up at night or after periods of inactivity, making it hard to get comfortable. Luckily, with the right care—including rest, ice, and anti-inflammatory treatments—bursitis can usually be managed effectively.
3. Nerve-Related Causes
Sometimes, arm pain doesn’t come from the muscles or joints at all—it can be nerve-related. Conditions likecarpal tunnel syndrome or a pinched nerve can cause pain that radiates down your arm, often accompanied by numbness or tingling.
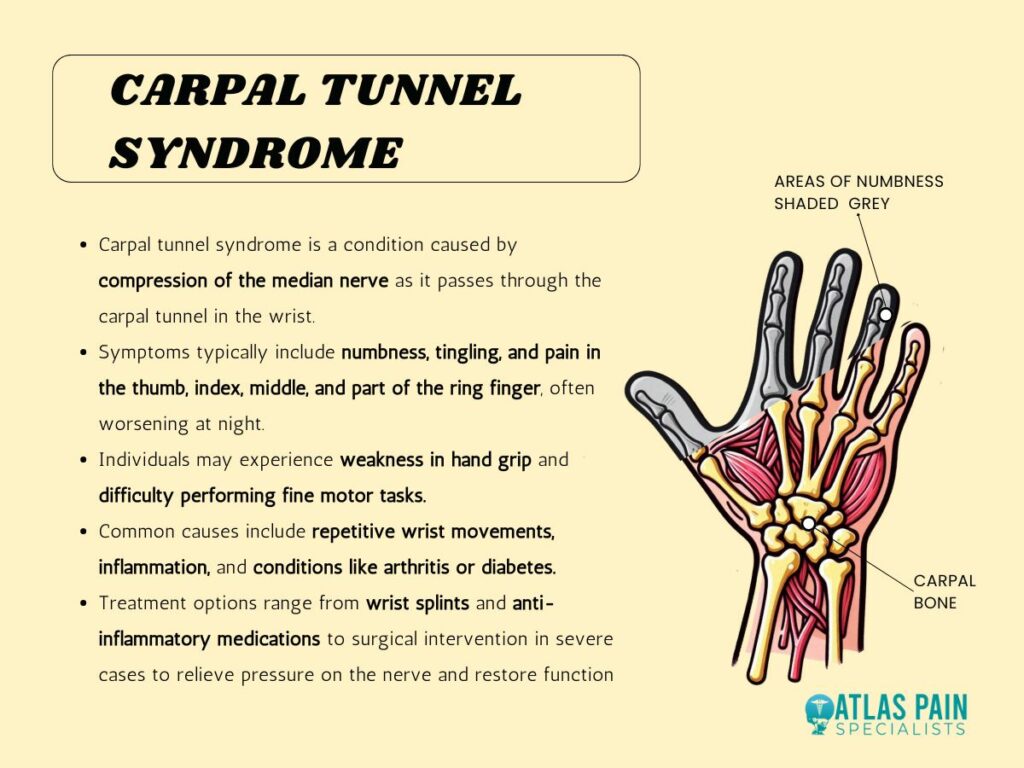
If the pain feels like it’s traveling, or if you’re experiencing weakness in your hand or fingers, nerve issues could be the culprit. Carpal tunnel syndrome, for instance, happens when the median nerve in your wrist becomes compressed, leading to pain, weakness, and discomfort that can make even simple tasks like holding a coffee cup a challenge.
Another nerve-related condition that could be behind your arm pain is a pinched nerve in your neck or upper back. This happens when a nerve gets compressed by surrounding tissues, like muscles or bones, causing pain to radiate down your arm.
Serious Causes of Arm Pain That Shouldn't Be Ignored
Sometimes arm pain is more than just a mild annoyance or the result of overuse—it can be a warning sign of something more serious happening in your body. When the pain feels different, more intense, or is accompanied by other symptoms, it’s important not to brush it off.
Your body has its own way of sending signals when something’s not right. While most arm pain can be managed with rest or simple treatment, there are cases when it’s crucial to take immediate action.
1. Heart-Related Pain
One of the more serious causes of arm pain is heart-related, especially when the discomfort radiates from your chest or upper body. While many people associate heart attacks with chest pain, arm pain—particularly in the left arm—can be one of the early warning signs.
If the pain is sudden, severe, or accompanied by shortness of breath, dizziness, or tightness in the chest, it could be a signal that something’s wrong with your heart. In these cases, it’s important to recognize that the pain isn’t just a muscle or joint issue.
Your heart can refer pain to other parts of the body, including the arm, as a way of letting you know it’s under stress.
2. Fractures and Broken Bones
If your arm pain follows a fall or a sudden impact, there’s a chance that you could be dealing with a fracture or broken bone. While some fractures are obvious and accompanied by swelling, bruising, or deformity, others might not be as immediately clear.
A hairline fracture, for example, can still cause significant pain even if the arm doesn’t look broken. In these cases, pushing through the pain or waiting for it to go away on its own can lead to complications, such as improper healing or long-term issues with mobility.
The sharp, persistent pain that comes from a fracture or break is your body’s way of telling you that something’s wrong. If you suspect a break, it’s crucial to get it checked out so that the bone can be set properly and heal without complications.
3. Nerve Damage
While nerve-related pain has already been touched on, it’s important to note that severe or long-lasting nerve damage is a serious concern. If you’re experiencing ongoing tingling, numbness, or a sharp, electric-like pain in your arm, there could be significant nerve compression or damage that requires medical attention.
Unlike other sources of pain, nerve issues don’t always go away with rest, and they can actually get worse if not treated properly. Conditions like a pinched nerve or something more serious, like a herniated disc, can lead to nerve damage that affects your arm’s strength and ability to function.
If you’re finding it hard to grip objects or if the pain in your arm doesn’t seem to improve with basic care, it’s worth getting checked out to avoid long-term damage.
How to Manage Pain from Carpal Tunnel Syndrome
When you're dealing with arm pain, it can really disrupt your daily life. Taking small steps, like adjusting your posture or using at-home remedies, might help ease the pain, but if the problem persists, don't hesitate to reach out for medical advice.
In some cases, conditions like carpal tunnel syndrome can be the source of your arm pain, especially if the discomfort is concentrated in your wrist or radiates down your arm. Managing this type of pain involves a combination of rest, wrist support, and sometimes medical intervention.
Carpal tunnel syndrome highlights how arm pain can stem from issues with the nerves, and understanding how to treat and prevent it is essential in keeping long-term pain at bay. Learning how to address nerve-related pain can make a big difference in how you handle arm pain, whether it’s from carpal tunnel syndrome or another cause.
Managing pain isn’t just about addressing physical discomfort—your mental health plays a huge role in how you experience and cope with it. When you're dealing with chronic pain, the emotional strain can be just as overwhelming as the pain itself. Stress, anxiety, and depression often intensify the pain, creating a cycle that's hard to break.
That’s why mental health support is a vital part of effective pain management. By prioritizing your emotional well-being, you can gain better control over your pain and improve your overall quality of life, making it easier to heal and feel like yourself again.
Understanding the Connection Between Pain and Mental Health
Pain is more than just a physical sensation. It can affect every aspect of your life, including your emotional well-being. In fact, pain and mental health are often closely connected, with each influencing the other in powerful ways. Understanding this connection is crucial to finding the right approach to managing both your physical and emotional health.
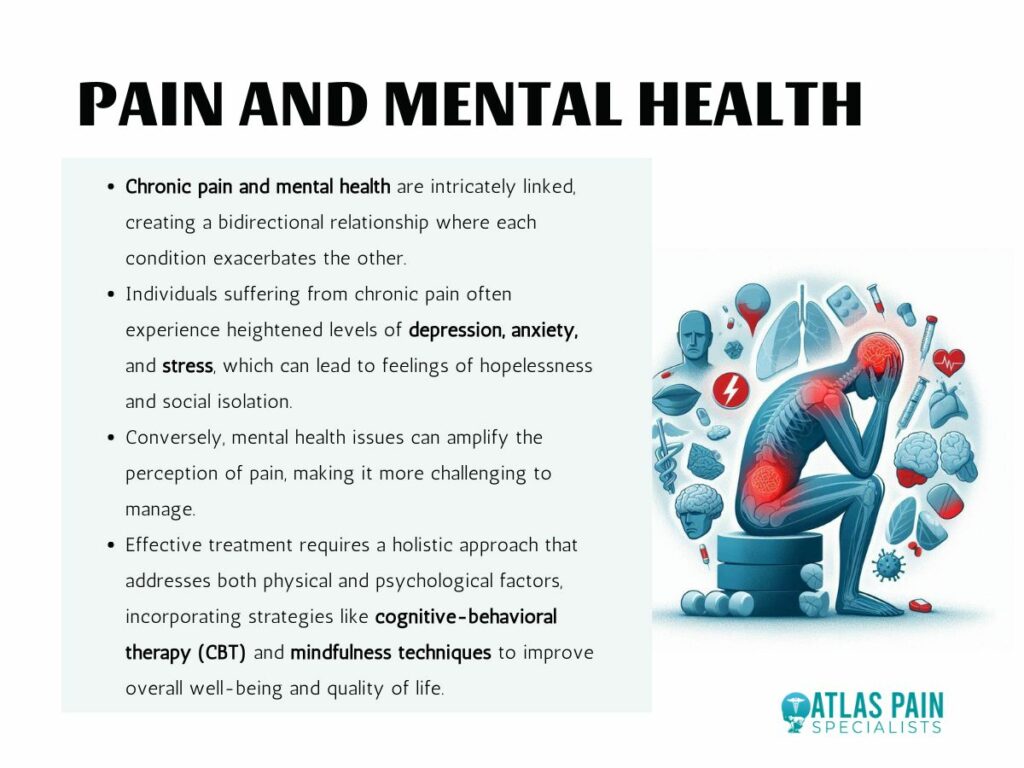
The Impact of Chronic Pain on Mental Health
Living with chronic pain can take a toll on your mental health. Prolonged pain often leads to feelings of frustration, anxiety, and depression. This emotional distress can, in turn, make the physical pain feel worse. When you're constantly in pain, it can be difficult to stay positive, leading to a cycle where your mood and pain levels feed off each other.
How Mental Health Affects Your Perception of Pain
Your mental state doesn’t just affect how you cope with pain—it can also influence how you physically feel it. Stress, anxiety, and depression can heighten your sensitivity to pain, making even mild discomfort feel unbearable. The brain processes pain signals differently when you are under emotional distress, often amplifying the sensation.
The Role of Mental Health Support in Pain Management
Given the strong connection between pain and mental health, it’s no surprise that mental health support plays a crucial role in pain management. Addressing both the physical and emotional aspects of pain is key to achieving long-term relief.
Cognitive Behavioral Therapy (CBT) for Pain Management
One of the most effective mental health treatments for pain management is cognitive behavioral therapy (CBT). CBT helps you change negative thought patterns that contribute to pain and teaches you coping strategies to manage discomfort. By changing how you think about your pain, you can reduce its emotional impact and improve your ability to cope with it.
CBT focuses on breaking the cycle of pain and emotional distress by addressing both the mental and physical aspects.
The Importance of Emotional Support
Living with chronic pain can be isolating, and many people find it difficult to talk about their experiences. Having a strong support network of friends, family, or even a therapist can make a significant difference in how you cope with pain. Emotional support helps you stay positive and can provide a sense of comfort when you're feeling overwhelmed by pain.
Support groups, both in-person and online, can also be beneficial. Talking to others who understand what you're going through can reduce feelings of isolation and give you new insights into managing pain.
Integrating Mental Health into Pain Management Plans
Many healthcare providers now recognize the importance of integrating mental health support into pain management plans. Treating pain isn't just about addressing the physical symptoms—it’s also about ensuring that the emotional aspects of pain are managed. For this reason, pain management programs often include mental health counseling, stress management techniques, and relaxation exercises like meditation or yoga.
By addressing both your mental and physical health, you can create a more comprehensive pain management plan that leads to better outcomes. It's important to take a holistic approach where attention to both appearance and structure ensures long-term stability.
Barriers to Accessing Mental Health Support in Pain Management.
Mental health support plays a critical role in managing chronic pain, but accessing this support isn't always easy. There are several barriers that can prevent individuals from getting the mental health care they need. Understanding these challenges is the first step in finding ways to overcome them and improve overall pain management.
Stigma Surrounding Mental Health
One of the biggest barriers to accessing mental health support is the stigma that still surrounds mental health issues. Many people feel ashamed or embarrassed to seek help for emotional or psychological struggles, especially when it comes to pain management.
This stigma can prevent individuals from seeking the care they need, leaving them to suffer in silence. When chronic pain is involved, there’s often a perception that focusing on mental health might downplay the seriousness of the physical pain. However, the connection between mental health and physical pain is real, and ignoring it can make the pain even worse.
Limited Access to Resources
Another significant barrier is limited access to mental health resources. In many areas, especially rural or underserved communities, there are simply not enough mental health professionals to meet the demand. Even in more populated regions, long wait times and limited availability of mental health providers can make it difficult to get timely care.
The cost of mental health services can be prohibitive for many individuals. Without insurance coverage or affordable options, seeking counseling or therapy may feel out of reach. This lack of access is a major roadblock for those who need support as part of their pain management plan and can lead to more costly repairs down the road.
Lack of Awareness
Many people are simply unaware of the role mental health plays in pain management. They may not realize that addressing their emotional well-being can have a direct impact on their physical pain.
This lack of awareness can prevent individuals from seeking out the mental health support they need, leaving them to focus solely on physical treatments that may not fully address their pain. Increasing awareness about the connection between mental health and pain can help more people take proactive steps to get the support they need.
Recommendations for Improving Mental Health Support in Pain Management
Given the barriers to accessing mental health support, it's clear that improvements are needed to ensure that individuals managing chronic pain can receive the comprehensive care they deserve.
Raising Awareness About the Connection Between Pain and Mental Health
One of the most important steps in improving mental health support is raising awareness. Healthcare providers, including doctors and pain specialists, need to emphasize the link between mental health and chronic pain. Educating patients about how their mental state can influence their physical pain can encourage them to seek out mental health support as part of their treatment plan.
This education should start early in the pain management process. The sooner patients understand the importance of mental health in managing pain, the more likely they are to seek help when they need it.
Expanding Access to Mental Health Services
To address the issue of limited access, there need to be more mental health professionals available, particularly in underserved areas. Telehealth services can be an effective solution, providing patients with access to mental health support from the comfort of their own homes.
By offering online therapy and counseling options, patients who may not have access to local providers can still get the care they need. Insurance companies and healthcare providers should also work to make mental health services more affordable. Investing in mental health support can prevent more significant issues down the line.
Integrating Mental Health into Pain Management Plans
Mental health support should be fully integrated into pain management plans. Rather than treating mental health as a separate issue, it should be considered an essential part of managing chronic pain. This means that pain specialists should work closely with mental health professionals to provide coordinated care that addresses both the physical and emotional aspects of pain.
For example, if a patient is receiving treatment for back pain, their plan should include not only physical therapies but also mental health support, such as counseling or stress management techniques.
Reducing Stigma Around Mental Health
Reducing the stigma surrounding mental health is critical for encouraging individuals to seek help. Public awareness campaigns and education initiatives can play a significant role in breaking down the barriers of stigma and making mental health care more accessible and acceptable.
Healthcare providers can also help by normalizing conversations about mental health during routine check-ups and pain management appointments. When patients feel that it’s normal and encouraged to discuss their emotional well-being, they may be more likely to seek the help they need.
Providing Supportive Resources and Tools
Finally, providing patients with easy access to mental health resources and tools can improve their ability to manage both their pain and emotional health. Support groups, mobile apps, and online therapy platforms can all offer valuable support for individuals who may not have access to traditional services.
Managing chronic pain effectively requires access to mental health support tools. Patients should be informed about the resources available to them so they can take control of their own care.
Pain Management for Athletes: Balancing Performance and Injury Prevention
When it comes to athletes, balancing performance with injury prevention requires a strategic approach that often extends beyond just physical conditioning. Managing pain effectively is a key part of staying at the top of your game, and the right pain management plan can help you not only recover faster but also prevent further injury.
As we explore pain management strategies for athletes, you'll discover how a proactive approach can keep you performing at your best while minimizing the risk of long-term damage.
Selecting the right pain management clinic is crucial for effectively managing chronic pain and improving your quality of life. With numerous clinics offering various treatments, it’s important to consider key factors such as specialization, range of services, practitioner expertise, and available telehealth options.
By carefully evaluating each clinic, you can find one that aligns with your specific needs and offers a comprehensive approach to pain management. This guide will help you understand what to look for in a pain clinic, ensuring you make an informed choice for long-term relief and well-being. Let's look at how to choose the right pain management clinic.
Understanding Pain Management Clinics
Before diving into the process of selecting a clinic, it’s important to understand what pain management clinics are and their purpose. These clinics specialize in diagnosing and treating chronic pain, using various techniques to improve the patient’s quality of life.
The goal is to provide long-term pain relief by addressing the underlying causes of pain or managing the symptoms effectively. Pain management clinics often take a holistic approach to treatment, considering physical, emotional, and mental well-being.

Types of Pain Management Clinics
There are two main types of pain management clinics, and understanding the difference can help narrow your choices:
- Procedure-Focused Clinics
These clinics emphasize interventional treatments and procedures, such as nerve blocks, steroid injections, and radiofrequency ablation. The primary focus here is reducing pain through targeted interventions, often performed by specialists like anesthesiologists, orthopedic surgeons, or pain specialists. - Interdisciplinary Clinics
These clinics take a more comprehensive approach, involving multiple healthcare professionals like doctors, physical therapists, psychologists, and nutritionists. They often provide a combination of treatments such as medication, physical therapy, counseling, and lifestyle modifications. This approach is ideal for those who want to explore a wider range of pain management techniques beyond just procedures.
Initial Steps in Finding a Pain Management Clinic
Choosing the right pain management clinic requires careful research and consideration. Below are two important steps to begin your search.
A. Consult Your Primary Care Physician
Your primary care physician (PCP) is often the best place to start when looking for a pain management clinic. They know your medical history and can provide valuable referrals based on your condition and needs.
Importance of Referrals
A referral from your PCP adds a layer of trust to your decision-making process. Your doctor will likely refer you to a reputable clinic with specialists experienced in managing your type of pain.
Additionally, many insurance plans require a referral before covering visits to specialists like pain management doctors. Therefore, consulting your PCP not only helps in finding the right clinic but also ensures your treatment is covered by insurance.
Discussing Pain History and Treatment Options
When consulting your PCP, discuss your pain history in detail, including past treatments and their effectiveness. Your doctor can help you determine the type of pain management approach that might work best for you, whether it’s interventional procedures or a more holistic, interdisciplinary approach.
Based on this conversation, they can guide you toward a clinic that aligns with your specific needs.
B. Research Pain Support Groups
Pain management isn’t just about medical treatments—it’s also about emotional and psychological support. Pain support groups, both online and in-person, can be a great resource when searching for the right clinic.
Benefits of Community Support
Joining a pain support group can provide you with emotional relief and encouragement from others who understand your struggles. These communities can offer insights into various treatment experiences, what worked or didn’t work for others, and which clinics they recommend. The shared experiences can help you feel less isolated in your journey toward pain management.
Gathering Recommendations from Peers
Support groups can be an excellent way to gather first-hand recommendations. Many people in these groups have likely visited several clinics and can share their honest experiences, including the quality of care, professionalism of the staff, and overall effectiveness of treatments.
This information can be invaluable when you’re trying to narrow down your options.
Key Factors to Consider When Choosing a Clinic
When evaluating a pain management clinic, several factors should be weighed carefully to ensure you receive the best care possible.
A. Specialization and Expertise
The first step in finding the right clinic is ensuring that it specializes in treating your specific pain condition. Chronic pain comes in many forms, from neuropathic pain to musculoskeletal conditions, and finding specialists familiar with your condition can greatly improve treatment outcomes.
Importance of Finding Specialists Familiar with Specific Pain Conditions
Each type of chronic pain requires a unique treatment approach, and general pain management techniques may not always be effective. Clinics specializing in your specific pain condition, whether it’s sciatica, fibromyalgia, or complex regional pain syndrome, will have a deeper understanding of the most effective treatments and interventions.
These specialists will also be more adept at managing the unique challenges associated with your condition.
Verification of Board Certification and Training
To ensure the quality of care, verify that the clinic’s practitioners are board-certified in pain management or relevant specialties like anesthesiology, physical medicine, or neurology.
Certification indicates that the provider has received specific training in pain management and has passed rigorous exams in this area. Board certification also shows that the practitioner adheres to continuing education requirements to stay current with evolving treatment methods.
B. Range of Services Offered
A well-rounded clinic will offer a variety of services to address chronic pain from multiple angles. Pain management is not a one-size-fits-all solution, and having access to a broad range of treatments increases the likelihood of finding a combination that works for you.
Overview of Treatment Options
Effective pain management often includes a mix of interventions, such as physical therapy, psychological therapies like cognitive-behavioral therapy (CBT), medications, and interventional procedures (e.g., injections, nerve blocks). The clinic you choose should offer a comprehensive array of treatments so you can explore multiple options and tailor your care plan.
Importance of a Multidisciplinary Approach
Multidisciplinary clinics, which bring together experts from different fields, can provide a more holistic treatment plan. For instance, a clinic that combines medical treatments with physical rehabilitation and psychological support may offer better long-term outcomes than one that focuses solely on medication or procedures.
C. Credentials and Experience of Practitioners
While a clinic’s range of services is important, the quality of the practitioners delivering those services is equally critical.
- Checking Qualifications and Experience: It’s important to check the credentials and experience of the clinic’s team. Look for practitioners who are board-certified and have a proven track record in treating your specific type of pain. More experienced practitioners will have seen a wider range of cases and are more likely to offer effective solutions, even for complex or rare conditions.
- Importance of Experience with Specific Pain Conditions: Experience is especially important if your pain condition is rare or difficult to treat. Specialists with years of experience treating patients with conditions like trigeminal neuralgia or cluster headaches will be more adept at managing your care, as they have likely refined their treatment strategies over time.
D. Telehealth Options
Telehealth has emerged as a valuable tool in pain management, especially for patients who may have mobility issues or live far from a clinic.
- Availability of Virtual Consultations: Virtual consultations allow patients to receive guidance, follow-up care, and consultations without the need to travel. This can be particularly beneficial for those with severe pain that makes traveling difficult or for patients living in rural areas.
- Benefits for Mobility-Challenged Patients: For those with limited mobility, telehealth offers an accessible option for staying in touch with healthcare providers, adjusting medications, or receiving counseling. A clinic that offers robust telehealth services ensures that you can maintain consistent care without the added burden of traveling.
E. Insurance Coverage and Payment Options
Understanding your insurance coverage and available payment options is a crucial step in selecting a pain management clinic. Treatment for chronic pain can be ongoing, and costs can add up quickly.
- Importance of Understanding Coverage Details: Before committing to a clinic, check whether it accepts your health insurance. Ensure that any treatments or procedures you may need are covered under your plan. Ask for a detailed breakdown of what your insurance will cover, including consultations, procedures, and follow-up appointments.
- Inquiring About Self-Pay Options and Discounts: If you don’t have insurance or your coverage is limited, inquire about self-pay options. Many clinics offer payment plans or discounts for patients who pay out of pocket. It’s also important to ask about any hidden fees or additional costs that may arise during treatment, such as for diagnostic tests or specialized procedures.
Questions to Ask Potential Clinics
Once you’ve identified some potential clinics, it’s essential to ask specific questions to evaluate their suitability for your needs.
A. Treatment Approaches
The clinic’s approach to treatment can greatly impact your care experience. You’ll want to understand whether they take a holistic approach or focus more on medication-based therapies.
- Types of Therapies and Interventions Available: Ask about the specific types of treatments the clinic offers. Does the clinic focus on interventional procedures, such as nerve blocks or epidurals, or do they provide a broader range of services like physical therapy, acupuncture, or psychological support?
- Focus on Holistic Care vs. Medication-Centric Approaches: A clinic that offers holistic care will provide a range of non-medication treatments, such as physical therapy, counseling, or alternative therapies like acupuncture. Holistic clinics aim to treat the whole person, not just the symptoms, which can lead to better overall outcomes.
B. Patient Support and Education
A good clinic doesn’t just treat your pain—they support and educate you throughout your journey.
- Availability of Support Groups and Educational Resources: Ask if the clinic offers patient support groups or educational materials to help you better understand your condition. Support groups provide a space for patients to share their experiences and learn from one another, while educational resources can empower you to take an active role in your treatment.
- Opportunities for Family Involvement in Treatment Planning: Chronic pain affects not only the patient but also their loved ones. Some clinics encourage family involvement in treatment planning, which can provide additional emotional support and help family members better understand your pain and the treatment process.
Red Flags to Avoid
While searching for the right clinic, there are certain warning signs that you should be aware of. Avoid clinics that exhibit the following red flags:
A. Clinics Focused Solely on Narcotics
Some clinics may over-rely on narcotics or opioids to manage pain. While opioids can be an effective short-term solution, they carry the risk of dependency and often don’t address the root cause of pain.
- Risks Associated with Opioid Dependency: Long-term use of opioids can lead to tolerance, dependence, and even addiction. It’s important to choose a clinic that offers a comprehensive treatment plan rather than solely prescribing narcotics. The clinic should explore other options like physical therapy, psychological support, or interventional treatments to manage your pain.
- Importance of a Comprehensive Treatment Plan: A clinic that offers a variety of treatments shows that they are invested in treating your pain in a comprehensive manner, not just masking it with medication. Look for clinics that emphasize long-term solutions and rehabilitation rather than quick fixes.
Lack of Transparency or Communication
Communication is key to successful pain management. Avoid clinics that are unclear or evasive about treatment plans, costs, or expected outcomes.
- Importance of Clear Communication About Treatment Plans and Progress: The clinic should communicate openly about your treatment options, expected outcomes, and potential risks. You should feel empowered to ask questions, and the staff should be willing to explain your care plan in a way that you can easily understand. A lack of transparency or poor communication is a red flag that the clinic may not prioritize patient-centered care.
Conclusion
Choosing the right pain management clinic can significantly impact your journey toward managing chronic pain. By prioritizing specialization, a multidisciplinary approach, and experienced practitioners, you can find a clinic that provides effective, personalized care.
Don’t hesitate to ask important questions about treatment options and patient support, and remain mindful of red flags like over-reliance on narcotics. With careful consideration and research, you can select a clinic that helps improve your pain management and overall quality of life, guiding you toward a more comfortable and fulfilling future.
Chronic pain affects many individuals, and for women, hormonal fluctuations significantly impact pain experience. Hormones like estrogen, progesterone, and testosterone can alter pain sensitivity and modulation throughout life stages such as menstruation, pregnancy, and menopause.
These hormonal changes can exacerbate chronic pain conditions like endometriosis, fibromyalgia, migraines, and irritable bowel syndrome (IBS). Effective pain management involves understanding these hormonal influences.
This article examines how hormonal changes impact chronic pain in women, and provides strategies for managing pain with hormonal considerations. Integrating these factors into pain management can lead to better relief and improved quality of life.
The Role of Hormones in Pain Perception
Hormones play a crucial role in regulating pain perception, influencing how the body experiences and responds to pain. Here’s how different hormones contribute to this complex process:
Estrogen and Pain Sensitivity:
Estrogen, a primary female sex hormone, can affect pain sensitivity by modulating the body's pain pathways. Higher levels of estrogen, such as those during the follicular phase of the menstrual cycle, can increase pain sensitivity, making individuals more susceptible to pain. Conversely, lower levels of estrogen, such as during the luteal phase or menopause, may reduce pain sensitivity, though this effect can vary depending on the individual and the pain condition.
Progesterone and Pain Modulation
Progesterone, another key hormone in the female reproductive system, has been shown to have anti-inflammatory and analgesic properties, which can modulate pain perception. Elevated progesterone levels, particularly during the luteal phase of the menstrual cycle or pregnancy, can help alleviate pain by counteracting some of the inflammatory processes associated with pain. However, fluctuations in progesterone levels can also contribute to variations in pain perception.
Testosterone and Pain Response
Testosterone, though present at lower levels in women, can influence pain perception by exerting analgesic effects. Higher levels of testosterone may contribute to reduced pain sensitivity, while lower levels, such as those observed in menopause, could potentially lead to increased pain sensitivity. The exact impact of testosterone on pain perception in women is still an area of ongoing research.
Cortisol and Stress-Related Pain
Cortisol, a hormone produced by the adrenal glands in response to stress, can influence pain perception by modulating the body’s stress response. Chronic stress and elevated cortisol levels can heighten pain sensitivity and contribute to the development or exacerbation of chronic pain conditions. Conversely, balanced cortisol levels are essential for maintaining proper pain modulation and managing stress-related pain.
These hormonal influences on pain perception underscore the intricate relationship between hormonal fluctuations and pain sensitivity, highlighting the need for personalized approaches to pain management that consider individual hormonal profiles.
Chronic Pain Conditions Affected by Hormonal Changes
Several chronic pain conditions in women are notably influenced by hormonal changes, with fluctuations in hormones often exacerbating symptoms or altering pain perception. Here’s how hormonal changes impact specific chronic pain conditions:
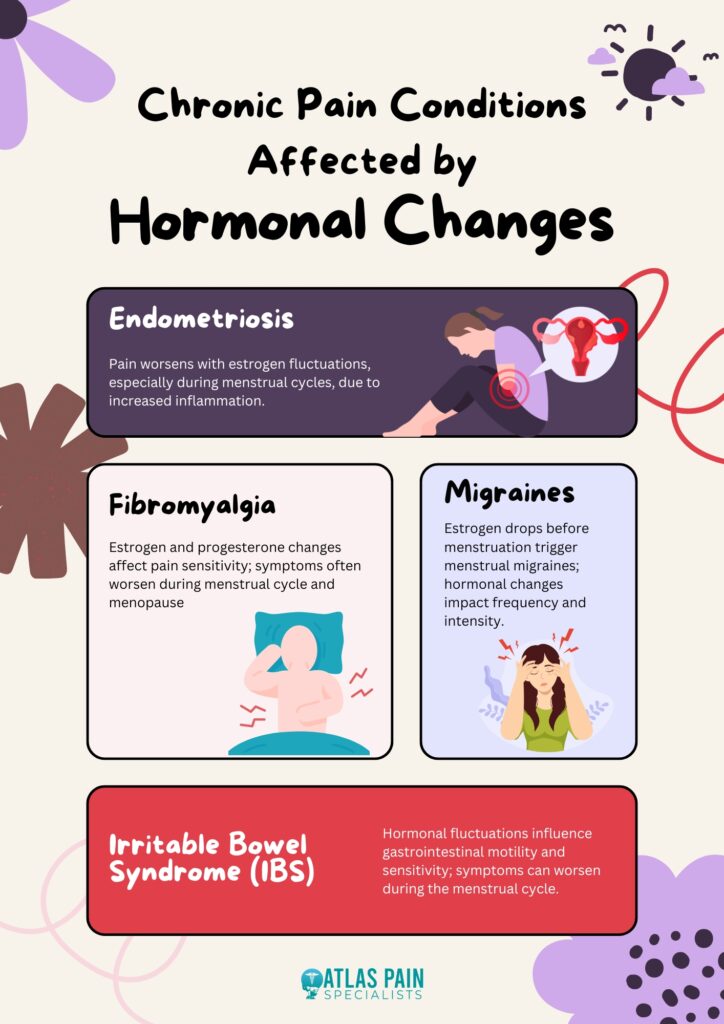
Endometriosis
Endometriosis is a condition characterized by the growth of tissue similar to the uterine lining outside the uterus, leading to significant pain and discomfort. Hormonal fluctuations, particularly variations in estrogen levels, can significantly impact the severity of endometriosis symptoms. Women often experience worsening pain during their menstrual cycle when estrogen levels are high, which can exacerbate the inflammatory processes associated with the condition.
Fibromyalgia
Fibromyalgia is a chronic condition marked by widespread musculoskeletal pain, fatigue, and tenderness. Hormonal changes, including those related to the menstrual cycle and menopause, can influence the severity of fibromyalgia symptoms. Estrogen and progesterone fluctuations are thought to affect pain sensitivity, with some women reporting increased pain during specific phases of their menstrual cycle or around menopause.
Migraines
Migraines are severe, recurring headaches that can be significantly influenced by hormonal changes. Many women experience migraines in relation to their menstrual cycle, a phenomenon known as menstrual migraines. The drop in estrogen levels just before menstruation is often linked to migraine attacks, making hormonal fluctuations a key factor in the frequency and intensity of migraines.
Irritable Bowel Syndrome (IBS)
IBS is a gastrointestinal disorder that can cause chronic abdominal pain, bloating, and changes in bowel habits. Hormonal changes can affect IBS symptoms, with many women experiencing exacerbations of their symptoms during their menstrual cycle. Fluctuations in estrogen and progesterone can influence gastrointestinal motility and sensitivity, contributing to the variability in IBS symptoms.
These chronic pain conditions illustrate the significant impact that hormonal changes can have on pain perception and management, highlighting the need for targeted approaches to treatment that consider hormonal influences.
Managing Chronic Pain with Hormonal Considerations
Effectively managing chronic pain in women requires addressing the impact of hormonal fluctuations on pain perception. Here are some strategies that consider hormonal influences:
Hormone Therapy
Hormone therapy, including estrogen or progesterone treatments, may be used to manage pain related to hormonal fluctuations. This approach needs to be tailored to individual needs and monitored by a healthcare provider to ensure effectiveness and minimize potential side effects.
Lifestyle Modifications
Adopting a healthy lifestyle can help manage chronic pain and its hormonal influences. Regular exercise, a balanced diet, and effective stress management can alleviate some of the symptoms and improve overall well-being. Maintaining a healthy weight and staying active can also enhance pain management.
Pain Management Techniques
Various techniques, such as cognitive-behavioral therapy (CBT), acupuncture, and mindfulness-based stress reduction (MBSR), can be beneficial. These approaches help manage chronic pain and its psychological impacts by developing coping strategies and reducing pain perception.
Medical Interventions
Medications, including analgesics, anti-inflammatory drugs, and hormone-specific treatments, can be used to address chronic pain. A healthcare provider can help determine the most appropriate medication regimen based on individual symptoms and hormonal factors.
By incorporating these strategies, individuals can better manage chronic pain while addressing the underlying hormonal influences.
Additional Tips to Manage Chronic Pain in Women
In addition to the primary strategies for managing chronic pain, there are several additional tips that can help women cope with pain exacerbated by hormonal changes:
Track Hormonal Cycles
Keeping a detailed record of menstrual cycles, hormonal fluctuations, and pain patterns can help identify triggers and patterns. This information can be valuable for adjusting treatments and predicting periods of increased pain.
Consider Hormonal Contraceptives
For some women, hormonal contraceptives can help regulate menstrual cycles and stabilize hormone levels, which may reduce pain associated with conditions like endometriosis or menstrual migraines. Consult a healthcare provider to determine if this approach is suitable.
Explore Dietary Adjustments
Certain dietary changes, such as increasing omega-3 fatty acids, reducing caffeine and sugar intake, and incorporating anti-inflammatory foods, can help manage pain. A nutritionist can provide personalized recommendations based on individual needs and hormonal influences.
Practice Relaxation Techniques
Stress can exacerbate pain and hormonal imbalances. Techniques such as deep breathing exercises, yoga, and progressive muscle relaxation can help reduce stress and improve pain management.
Use Heat and Cold Therapy
Applying heat or cold to affected areas can provide temporary relief from pain. Heat can relax muscles and alleviate stiffness, while cold packs can reduce inflammation and numb painful areas.
Stay Hydrated
Proper hydration is essential for overall health and can help prevent dehydration-related muscle cramps and discomfort. Drinking adequate water throughout the day can support pain management and overall well-being.
Seek Support Groups
Joining support groups or online communities for women with similar pain conditions can provide emotional support and practical advice. Sharing experiences and strategies can be empowering and help manage chronic pain.
Consult a Pain Specialist
Working with a pain specialist who understands the interaction between hormones and pain can lead to more tailored and effective treatment plans. They can offer advanced therapies and interventions specific to hormonal pain issues.
Incorporating these additional tips can enhance the management of chronic pain and address the specific challenges posed by hormonal changes.
Summary
Understanding the impact of hormones on chronic pain is essential for effective management in women. Hormones like estrogen, progesterone, and testosterone can influence pain sensitivity and worsen conditions such as endometriosis, fibromyalgia, migraines, and irritable bowel syndrome (IBS). Addressing these hormonal effects through hormone therapy, lifestyle changes, and targeted pain management strategies can enhance pain relief and overall well-being.
By integrating hormonal considerations into treatment plans, women can achieve better control over chronic pain and improve their quality of life.
If you’ve been living with chronic pain, you know how much it can take over your life. It can make even the simplest tasks feel overwhelming and steal the joy from activities you once loved.
Finding relief becomes a daily struggle, and it’s easy to feel like you’ve tried everything with little success. But there’s hope. Neuromodulation is an innovative treatment that’s making a real difference for many people like you.
It’s not just about masking pain; it’s about giving you the chance to regain control over your life. Whether you’re dealing with persistent back pain, nerve pain, or other chronic conditions, neuromodulation might be the option that helps you finally find relief.
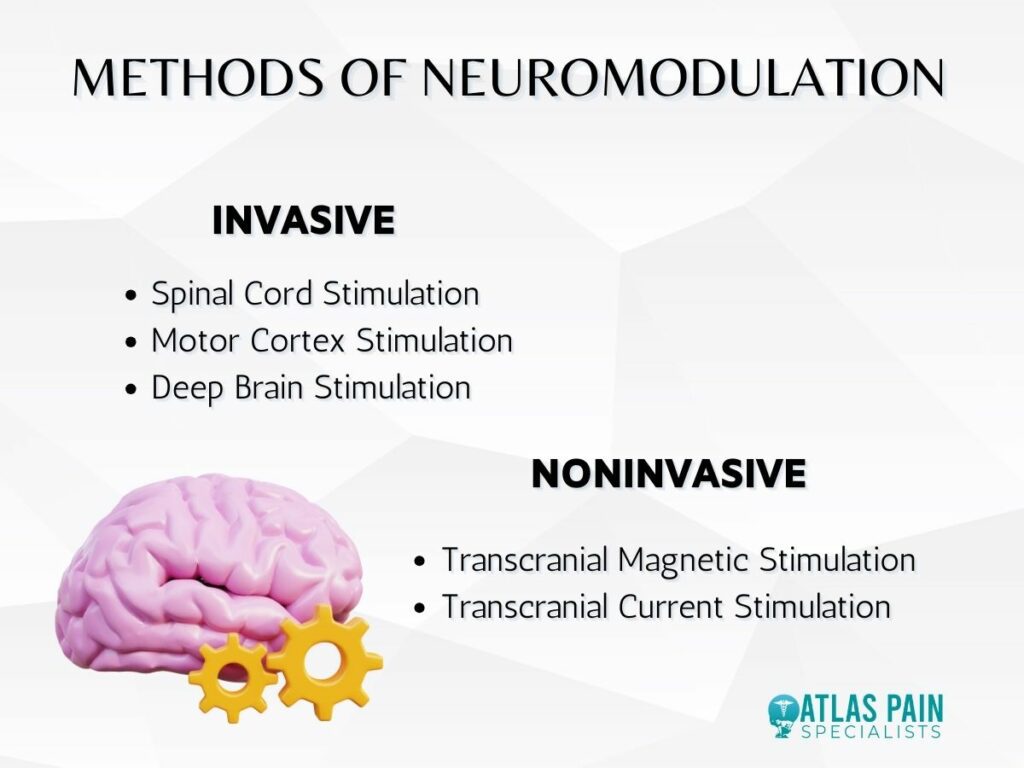
What is Neuromodulation?
When you’re dealing with chronic pain, you want a solution that targets the problem at its source. Neuromodulation offers that kind of precision. It’s a treatment that’s gaining attention for its ability to help people who haven’t found relief through other methods.
But what exactly is neuromodulation, and how can it make such a difference in your life? Neuromodulation isn’t just another approach to managing pain; it’s a way to actively change how your body processes pain signals.
How Neuromodulation Works
Neuromodulation involves the use of technology to alter nerve activity in your body. This is usually done through electrical impulses or chemical agents that are delivered directly to the nerves responsible for your pain.
These impulses work by blocking or modifying the pain signals before they reach your brain, effectively reducing the intensity of the pain you feel. There are different types of neuromodulation, with spinal cord stimulation (SCS) being one of the most common.
In SCS, a small device is implanted near your spine, where it delivers electrical impulses to the spinal cord. This interrupts the pain signals that travel to your brain, replacing them with a tingling sensation instead of pain.
Other forms include peripheral nerve stimulation, which targets specific nerves outside the spinal cord, and deep brain stimulation, used for more complex pain conditions.
Conditions Treated by Neuromodulation
Neuromodulation is a versatile treatment option that can be tailored to suit different types of chronic pain. It’s commonly used for conditions like chronic back pain, especially when it’s linked to nerve damage or failed back surgery syndrome.
If you’re struggling with nerve pain, such as that caused by diabetic neuropathy or complex regional pain syndrome (CRPS), neuromodulation might offer relief where other treatments have failed.
This treatment isn’t just limited to these conditions, though. It’s also used for pain related to conditions like fibromyalgia, migraines, and even certain types of pelvic pain. The adaptability of neuromodulation makes it a promising option for many people who have struggled to find effective pain management.
The Key Benefits of Neuromodulation
When you’re living with chronic pain, every day can feel like a challenge. Finding a treatment that truly helps can make all the difference, not just in how you feel physically but in your overall quality of life.
Neuromodulation stands out because it offers several key benefits that can directly impact your daily experiences. Choosing neuromodulation is about more than just pain relief. It’s about taking back control and improving how you live.
With a treatment that’s customizable, minimally invasive, and adjustable to your needs, neuromodulation provides a way to address your pain in a more targeted and effective manner.
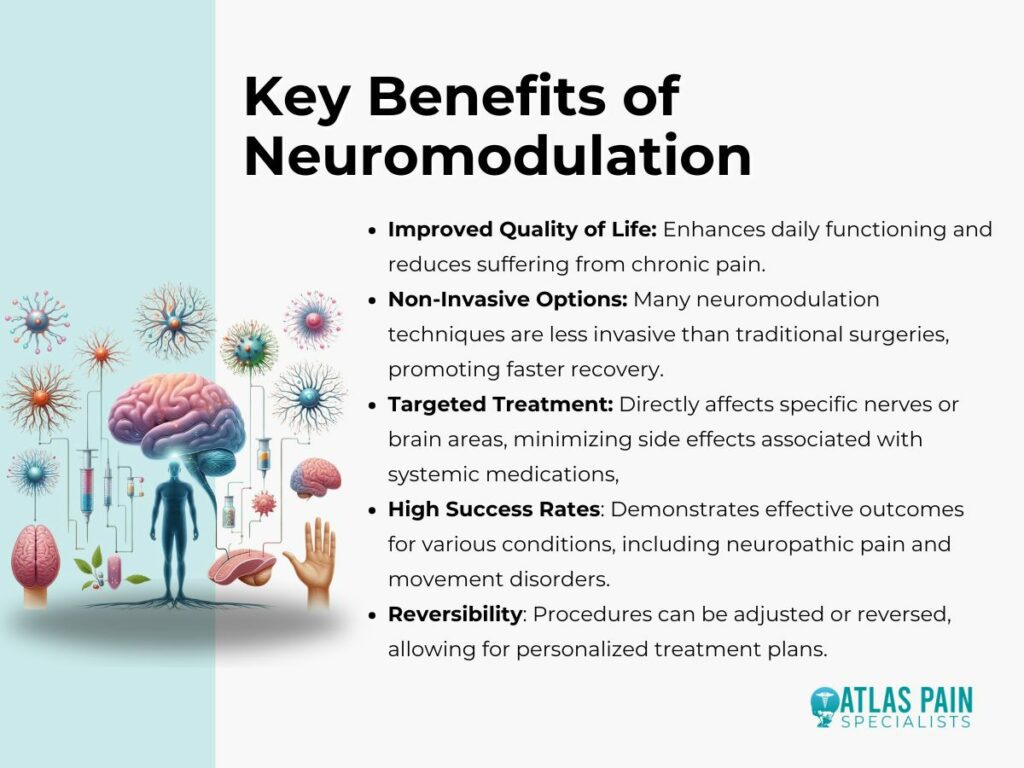
1. Pain Relief Without Heavy Reliance on Medications
One of the biggest advantages of neuromodulation is that it offers a way to manage pain without relying solely on medications. This can be a huge relief, especially if you’ve been concerned about the side effects or long-term use of painkillers.
Neuromodulation provides targeted relief, helping to reduce or even eliminate the need for other pain medications. By focusing on the nerves that are causing your pain, neuromodulation can offer significant relief where it’s needed most.
This direct approach means you might be able to cut back on medications that come with their own set of challenges, helping you feel better overall.
2. Improved Quality of Life
Pain doesn’t just affect your body; it impacts every aspect of your life. Neuromodulation can help you get back to doing the things you love, whether that’s spending time with family, pursuing hobbies, or simply enjoying a good night’s sleep.
The relief provided by neuromodulation can make it easier to participate in daily activities, which can boost your mood and overall well-being. Feeling better physically can lead to improvements in your mental and emotional health, too.
3. Customizable and Adaptable Treatment
No two people experience pain in exactly the same way, which is why a one-size-fits-all treatment often isn’t enough. Neuromodulation is customizable, meaning it can be adjusted to meet your specific needs.
Whether your pain changes over time or you need different levels of stimulation, this treatment can be fine-tuned to offer the best possible results. This adaptability is a key reason why many people find success with neuromodulation.
Your treatment can evolve with you, providing ongoing relief as your condition or pain patterns change.
4. Minimally Invasive Approach
For many, the idea of a major surgery is daunting, especially when you’re already dealing with chronic pain. Neuromodulation offers a minimally invasive option, typically involving a simple procedure to implant the device.
Recovery is usually quicker than with more invasive surgeries, allowing you to start experiencing the benefits sooner. The minimally invasive nature of neuromodulation also means fewer risks and complications compared to more traditional surgical approaches.
5. Reversible and Adjustable Treatment
One of the standout features of neuromodulation is that it’s both reversible and adjustable. If the treatment isn’t working as expected, or if you want to stop it for any reason, the device can be adjusted or even removed entirely.
This flexibility gives you and your healthcare provider the ability to make changes as needed, ensuring the treatment is always working in your best interest. Before fully committing to the treatment, many patients also undergo a trial period.
This allows you to test how well neuromodulation works for your specific pain condition without making a permanent decision right away. If it’s effective, the treatment can continue; if not, adjustments can be made, or alternative options can be explored.
6. Increased Activity Levels
With chronic pain, it’s easy to fall into a cycle of inactivity, which can further exacerbate your condition. Neuromodulation can help break this cycle by providing pain relief that allows you to be more active.
Increased physical activity can, in turn, lead to better overall health, including improved strength, flexibility, and endurance. Neuromodulation promotes a healthier lifestyle by allowing you to move more freely and exercise frequently, both of which can help with long-term pain management and general well-being.
7. Better Sleep Quality
Chronic pain doesn’t just affect your waking hours; it can disrupt your sleep as well. Many people with chronic pain struggle with insomnia or poor sleep quality, which only worsens their overall health and well-being.
Neuromodulation can help address this issue by reducing the pain that keeps you awake at night. Better pain management through neuromodulation often leads to improved sleep, which in turn supports better overall health.
When you sleep better, you’re more likely to wake up feeling refreshed and ready to face the day, rather than fatigued and drained from a restless night.
8. Long-Term Cost Savings
While the initial cost of neuromodulation might seem significant, it’s important to consider the long-term financial benefits. Chronic pain often leads to ongoing expenses, including medications, frequent doctor visits, and even lost income from missed work.
Neuromodulation, by providing more effective pain relief, can reduce these ongoing costs over time. By potentially lowering your need for medications and reducing the frequency of medical visits, neuromodulation can help you save money in the long run.
Who Can Benefit from Neuromodulation?
Living with chronic pain can feel isolating, especially when it seems like nothing provides lasting relief. Neuromodulation offers a path forward for many people who are seeking more than just temporary solutions.
It’s a treatment designed for those whose pain has persisted despite trying various other methods, offering hope where other options might have fallen short. If you’re wondering whether neuromodulation could be the right choice for you, it’s important to understand who typically benefits from this approach.
Ideal Candidates for Neuromodulation
Neuromodulation is often considered for those who haven’t found sufficient relief through medications, physical therapy, or less invasive treatments. It’s particularly beneficial for people with chronic pain conditions such as:
- Failed back surgery syndrome
- Complex regional pain syndrome
- Neuropathic pain
- Certain types of nerve pain
If your pain is localized and has been resistant to other treatments, neuromodulation might be an option worth exploring. Your healthcare provider will assess your overall health, the nature of your pain, and how you’ve responded to other treatments to determine if neuromodulation is a good fit for you.
Common Patient Profiles
Neuromodulation has helped a wide range of people, from those dealing with long-term back pain to individuals with nerve-related pain disorders. If you’ve been managing your pain for years without finding lasting relief, you might be a candidate for this treatment.
Many who benefit from neuromodulation have tried multiple treatments, including surgery, without the desired outcome. Each person’s experience with chronic pain is unique, and neuromodulation offers a customizable approach that can be adapted to your specific situation.
Considerations and Potential Side Effects
When you’re thinking about trying a new treatment for chronic pain, it’s important to have all the information you need to make the best decision for your health. Neuromodulation offers many benefits, but like any medical procedure, it’s essential to consider the potential risks and side effects before moving forward.
Neuromodulation is a powerful tool, but it’s not a one-size-fits-all solution. Each person’s experience with this treatment can vary, so it’s crucial to have realistic expectations and be aware of what to look out for as you explore this option.
Potential Side Effects
While neuromodulation is generally safe, some potential side effects should be considered. These can include infection at the implant site, temporary pain at the implant location, and, in rare cases, hardware malfunction.
Some people may also experience changes in their pain patterns or develop new areas of discomfort. It’s important to discuss these possibilities with your healthcare provider, who can help you understand how likely these side effects are and how they can be managed.
Most side effects are temporary or manageable, but being aware of them allows you to take action quickly if something doesn’t feel right.
The Role of Neuromodulation in Chronic Pain Management
Chronic pain doesn’t have to define your life. If you’ve been searching for a treatment that offers more than temporary relief, neuromodulation could be the solution that finally helps you reclaim control.
It’s not just about reducing pain; it’s about giving you the freedom to enjoy your daily activities again with fewer limitations and a renewed sense of well-being. The role of neuromodulation in chronic pain management is essential to understanding why this treatment can be so effective.
This role is directly connected to the benefits we’ve discussed, showing how neuromodulation fits into a broader pain management strategy designed to improve your quality of life. If you’re ready to explore new possibilities in your pain management journey, neuromodulation might be the key to unlocking a better, more fulfilling life.
