The Role of Neuromodulation in Chronic Pain Management
Chronic pain is difficult to understand, treat, and live with for pain specialists and patients. You may be wondering what is the role of neuromodulation in chronic pain management.
Desperate patients may undergo radical and irreversible surgeries like nerve amputation to reduce pain, although even those may fail.Moreover, pharmaceutical medications rarely alleviate pain and can cause addiction, overdose, and death.
Patients often have low quality of life, frequent hospitalizations, and long-term opioid use. A unique technology that improves many people's quality of life has been developed thanks to research on pain perception and our nervous system's response to pain remedies.
This article discusses neuropathic pain and pharmacological treatments through neuromodulation to manage pain.
Table of Contents
Pharmacological Treatment of Pain
Traditional analgesics are commonly recommended for acute pain because they are effective and inexpensive. Concerns about the use of opioids to manage pain have been raised as a public health issue since the 1980s, and efforts have been made to address opioid addiction since then.
According to the Council On Foreign Relations, the United States has proclaimed an epidemic of opioid abuse and fatalities caused by opioids. However, the difficulty in controlling dosing and use increases the likelihood of side effects and adverse outcomes in situations of persistent neuropathic pain. This is because we all feel pain differently, and our opioid response is individual and inconsistent.
In order to minimize opioid side effects, NSAIDs are used to relieve pain by reducing inflammation or inflammatory factor production. However, at-risk groups with cardiovascular disease and stroke should not use NSAIDs; large doses in chronic use may cause renal and gastrointestinal adverse effects.
This calls for an even more effective treatment.
What is Neuromodulation?
Neuromodulation was ushered in by Dr. Norman Shealy, a neurosurgeon, who implanted the first device for the relief of intractable pain in 1967. Neuromodulation therapies help to re-establish normal function of the nervous system.
It works by sending regulated physical energy to the central nervous system's predetermined neuronal targets. The field of neurology is becoming interested in it because of its drug-free, nonaddictive, and better-targeted properties.
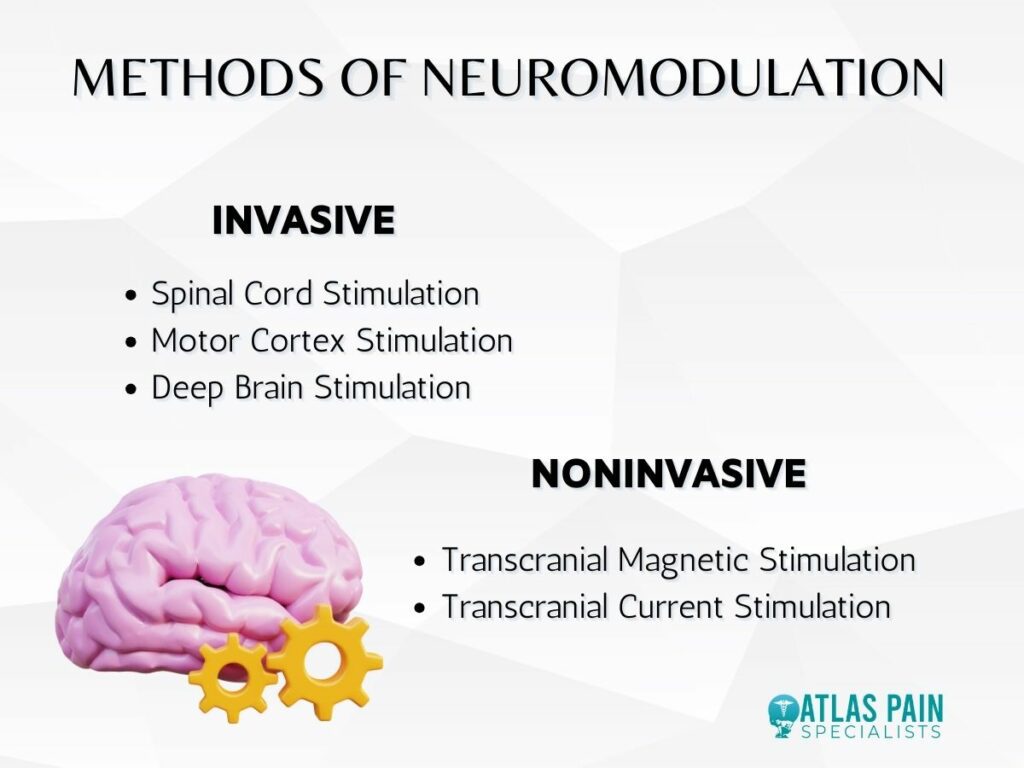
Methods of Neuromodulation
| Type of Method | Technique |
| Invasive | Spinal Cord StimulationMotor Cortex StimulationDeep Brain Stimulation |
| Noninvasive | Transcranial Magnetic Stimulation Transcranial Current Stimulation |
Brain neuromodulation devices, whether invasive or noninvasive, stimulate the brain with electrical, magnetic, optical, or acoustic energy to intervene with neuronal activation and restore health. Treatment with neuromodulation is more specific than medical treatments and more reversible than surgery or medication.
Neuromodulation for pain has several categories.
- Peripheral versus CNS modulation
Parkinson's disease can be treated with deep brain stimulation (DBS), pelvic problems and incontinence can be treated with stimulation of the sacral nerve, migraines can be treated with stimulation of the vagus nerve, and ischemic disorders of the heart and peripheral arteries can be treated with spinal cord stimulation.
- Invasive versus noninvasive modes of interface
Invasive neuromodulation is usually considered when pharmaceutical treatments fail due to its danger and cost. But with reliable, noninvasive neuromodulation techniques, it could be a nonaddictive alternative to opioids.
Invasive neuromodulation procedures like spinal cord stimulation (SCS), motor cortex stimulation (MCS), and deep brain stimulation (DBS) are used when treatments fail or patients have pre-existing problems. Invasive stimulations are expensive and require proper target localization, risk infections, and consequences.
This called for non-invasive neuromodulation, which, in recent advances, has led to chronic neuropathic pain treatments. TMS and TCS, despite their limited spatial locality and deep penetration, have shown potential pain reduction results.
1. Invasive Neuromodulation: Spinal Cord Stimulation
Spinal cord stimulation (SCS) is a popular form of neuromodulation used to treat persistent pain. Multiple pharmacological therapy strategies involve blocking CNS communication with the spinal cord.
It works like a gate, modulating the cortical and subcortical brain to perform an inhibition in the spinal cord. The primary sites of action are the trigeminal nerve for facial pain, the vagus nerves to lessen headaches and pain related to inflammation, and the dorsal root ganglion for peripheral pain.
A small lead (or wire) is inserted into the epidural area just outside the spinal cord to provide electrical stimulation for SCS. The compact generator device, with its associated lead, is surgically inserted in the subcutaneous tissue just below the skin of the buttocks or lower back.
The devices' frequent, low-voltage electrical impulses sent to the spine will modulate pain signals traveling to the brain. These impulses are often experienced as mild tingling or buzzing (a condition known as paresthesia) anywhere on the body.
The hardware and technology have improved since the initial device was installed, and patients report greater pain control and fewer vibrations. However, long-term efficacy in pain reduction is not consistent due to the possibilities of foreign body response encapsulation of electrodes or therapeutic tolerance.
2. Invasive Neuromodulation: Motor Cortex Stimulation
Patients with neuropathic pain who do not respond to pharmaceutical treatments may find relief through MCS, which has been demonstrated to alleviate pain in cases when deafferentation (the loss of pain-related afferent information) has occurred. Some examples of such pain types are
- Pain after a stroke
- Phantom limb pain
- Multiple sclerosis
- Injury to the spinal cord
Through small incisions in the skull, electrodes for epidural stimulation can be positioned over the motor cortex, with a typical stimulation frequency of 50 hertz. The mechanisms behind the MCS are a mystery.
Some researchers believe that the changing of the somatosensory and motor cortex at the level of deafferentation or above may be responsible for the pain associated with deafferentation. Therefore, pain alleviation can be achieved by stimulating the motor cortex, which disturbs the unusual arrangement.
One drawback of MCS is that it is challenging to predict which patients would benefit from treatment, which is especially problematic given the hazards and irreversibility of invasive procedures.
3. Invasive Neuromodulation: Deep Brain Stimulation
High specificity and therapeutic efficiency are provided by DBS in the CNS thanks to the implantation of electrodes at various depths within the brain. The basic parts of today's DBS systems consist of a patient programmer, an implantable pulse generator (IPG), and connection cables that link the DBS to the IPG and the targeted area of the brain.
The patient programmer acts as a radio or Bluetooth link between the doctor and the IPG, allowing for remote adjustments to DBS stimulation parameters. However, DBS necessitates permanent surgical implantation procedures and is associated with risks of inflammation, gliosis, and cell death.
As a result, there is a requirement for more precise and less risky stimulation target selection in the management of pain. Several neuromodulation methods have been discovered that do not require invasive surgical procedures to modulate brain tissue.
Noninvasive neuromodulation techniques have the potential to be applied in numerous applications despite the comparatively restricted spatial resolution compared with invasive procedures.
4. Noninvasive Neuromodulation: Transcranial Magnetic Stimulation
TMS generates rapidly changing magnetic fields using a coil of wire, which induces electromagnetic induction and eddy currents in the brain, eliciting synchronized brain activities at cortical brain regions.
The focused and pulsed magnetic stimulation is commonly delivered using a figure-eight coil. While transcranial magnetic stimulation (TMS) has been shown to be beneficial in treating pain, stroke, and Parkinson's disease, it still needs to have improvements made to its focality and penetrating depth in order to have more targeted effects in managing brain illnesses.
MCS is mostly used for pain treatment because TMS cannot focally excite deep brain regions, and the reduction in pain persists for days to weeks following daily stimulation due to plasticity.
Constraints imposed by the conductivity and permeability of the magnetic field mean that rTMS can only penetrate so far and can only provide a limited amount of spatial information. Disadvantages of a transcranial intervention tool include possible pain at the stimulation location and headache.
The loud, repetitive clicking sound that accompanies the magnetic stimulation pulses is another reason why TMS may not be appropriate for certain populations, such as young children, the elderly, or those suffering from tinnitus. The creation of a quiet TMS (qTMS) with an ultra-brief pulse for moving the transmitted energy towards the inaudible, high-frequency band is a new attempt to lessen such unwanted noises and address safety concerns.
5. Noninvasive Neuromodulation: Transcranial Current Stimulation
TCS is a noninvasive neuromodulation technology that uses rectangular or ring electrodes to regulate cortical excitability by applying low levels of current to the scalp. Using weak, direct currents, transcranial direct current stimulation (tDCS) alters cortical excitability and spontaneous neural activity, while tACS uses currents with alternating polarities to entrain neural oscillations.
Patients with neuropathic pain from traumatic spinal cord damage reported less discomfort after tDCS treatment, while those suffering from chronic low back pain reported less discomfort after tACS treatment. As with TMS, direct electrical stimulation through the scalp may cause scalp pain and safety risks, limiting TCS current and desired results.
An Overview of Ultrasound Neuromodulation
Many different clinical applications can be carried out with the help of high-intensity focused ultrasound, which is successful primarily through thermal induction or non-thermal ablation. Recently, low-intensity transcranial focused ultrasound (tFUS) has emerged as a noninvasive neuromodulation approach with the ability to target the deep brain thanks to its excellent spatial resolution and focal.
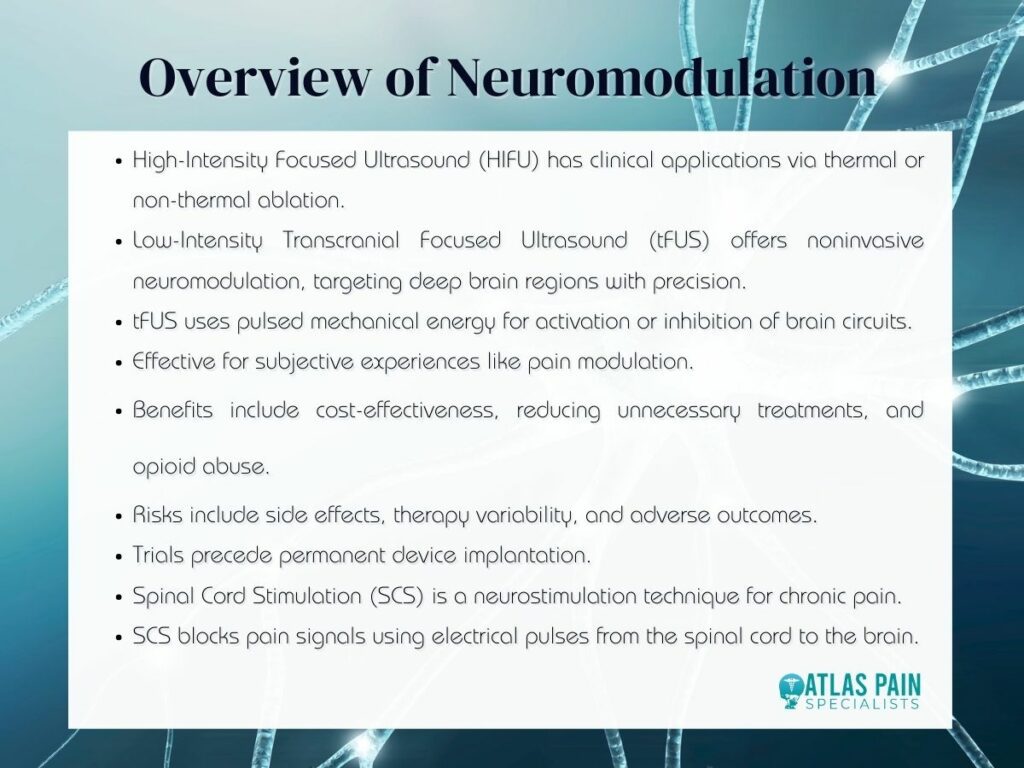
Transcranial ultrasound stimulation (tFUS) is a type of neuromodulation in which highly controllable, pulsed mechanical energy is sent through the skull with high spatial selectivity, and this energy may be guided and used to induce activation or inhibition by parameter tweaking.
An example of a subjective experience that requires multiple brain regions to process is pain. One can block the relevant brain areas or activate circuits that suppress downstream brain activities to alleviate such subjective pain.
The brain's response to tFUS modulation can be either excitatory or inhibitory, depending on the stimulation parameters and paradigm.
The Benefits of Neuromodulation in Pain Management
Neuromodulation treatments are usually offered after patients have tried drugs, physical and occupational therapy, or surgery due to their high cost and innovation. Insurance policies and clinical guidelines are evolving to incorporate neuromodulation early in the treatment planning process.
Early therapy with these techniques has been found to be cost-effective by reducing unnecessary doctor's visits, ER visits, hospitalizations, inefficient or hazardous surgeries, and opioid abuse, among other things. Your doctor will be in the best position to advise you on when to pursue these options based on your specific condition and response to previous pain treatments.
Neuromodulation treatment is not without risks.
Common side effects of medical procedures include excessive blood loss, infection, blood clots, and adverse drug reactions (in the case of an intrathecal pump). Due to individual differences in the neurological system, therapy outcomes may also vary between individuals.
Due to these concerns, a trial is always conducted prior to the permanent implantation of a device. Implantation, hardware failure, and stimulation-induced injury are all potential causes of adverse outcomes in patients with implanted DBS.
The Ultimate Guide to Spinal Cord Stimulation
Neuromodulation has shed light on the treatment of pain, particularly chronic pain. In recent years, spinal cord stimulation has emerged as a viable treatment option for a wide variety of back-related ailments.Neuromodulation, also known as neurostimulation, is a prevalent form of neurotherapy that uses electrical pulses to block pain signals en route from the spinal cord to the brain. Atlas Pain Specialists provides neuromodulation treatments to alleviate chronic pain, and in the same vein, here is the ultimate guide on spinal cord stimulation (SCS).
About Dr. Sean Ormond