Pain Management for Arthritis Sufferers
Arthritis is a common condition that affects millions of people worldwide. It refers to the inflammation of one or more joints, resulting in pain, stiffness, and reduced mobility.
There are several types of arthritis, but regardless of the type, one thing remains consistent – the significant impact arthritis has on the quality of life.
This article provides a comprehensive overview of pain management for arthritis sufferers, focusing on chronic and acute pain to help effectively manage their pain and improve their overall well-being.
Table of Contents
Causes of Arthritis Pain
Arthritis pain can be extremely disruptive and devastatingly affect one's way of life. Arthritis pain can be managed and alleviated if the underlying causes are identified and treated.
1. Inflammation
Inflammation happens when the immune system wrongly attacks the joints, causing swelling, redness, and pain. Several variables can set off this immune response, including heredity, physical trauma, infectious agents, and general joint wear and tear.
The pain associated with inflammatory arthritis disorders like rheumatoid arthritis and psoriatic arthritis can be excruciating and long-lasting.
2. Joint Damage
Arthritis pain can be either short-lived and severe (acute pain) or long-lasting and limiting (chronic pain). Arthritis pain has a profound impact on a person's mental and emotional health in addition to their physical health.
- When the cartilage that normally cushions the joints wears away, bones scrape against each other, resulting in degenerative conditions such as osteoarthritis. Due to this friction, pain, stiffness, and decreased movement follow.
- Arthritis pain can be worsened by joint injuries such as fractures or dislocations. When the joints are injured or inflamed, the nerve endings might become too sensitive, constantly relaying pain signals to the brain.
Pain amplification can make even the smallest of movements excruciating for people with arthritis. Arthritis pain might feel like aching or throbbing or even a sharp, shooting sensation, but its intensity and severity can vary greatly from person to person.
Stress, anxiety, and depression are all factors that might worsen when dealing with chronic pain. This means that controlling arthritis pain is all about finding strategies to lessen the condition's impact on daily living.
Types of Arthritis
Arthritis is an umbrella term for over a hundred distinct diseases affecting the joints. While the joint pain that characterizes all forms of arthritis is universal, the underlying causes and symptoms can differ widely.
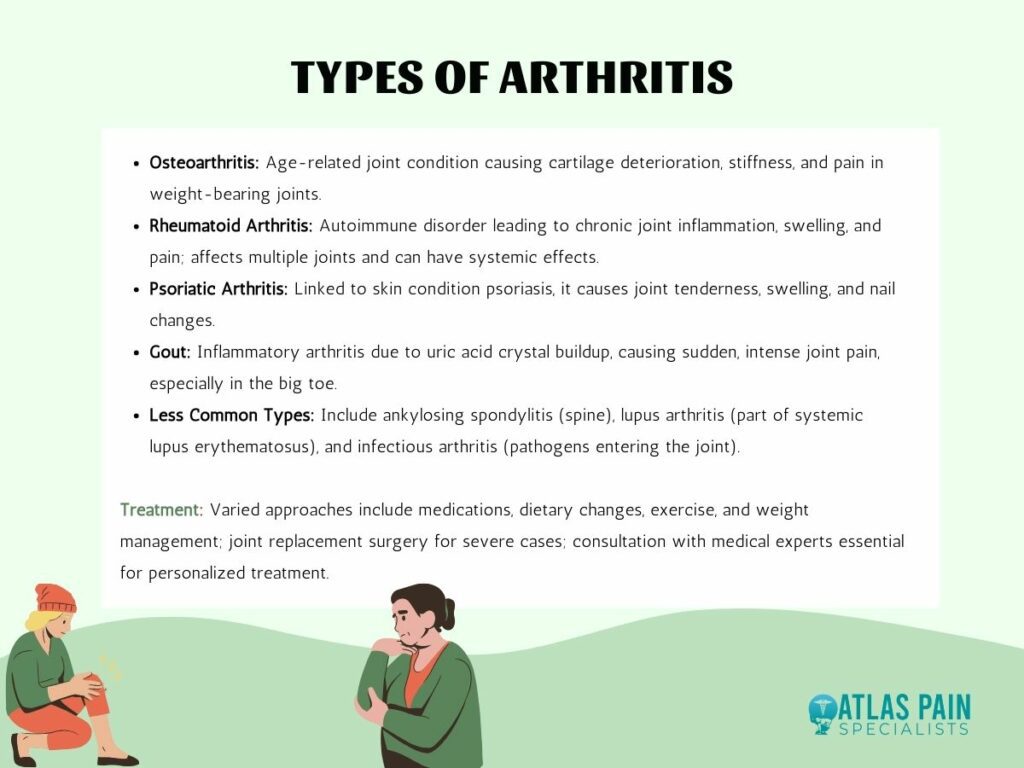
- Osteoarthritis
The degenerative joint condition is commonly linked to aging and arises from the progressive cartilage deterioration that cushions the bones' ends. The outcome is bone wear and tear, which causes stiffness, inflexibility, and eventual pain.
Symptoms of osteoarthritis tend to increase with time, and the condition is most common in weight-bearing joints, including the hips, knees, and spine.
- Rheumatoid arthritis
It's an autoimmune disorder that causes the immune system to wrongly attack the body's own tissues, especially the joints, resulting in a chronic inflammatory disease. This causes swelling and pain in the joints.
Multiple symmetrical joints may be affected by rheumatoid arthritis, and the disease frequently results in joint abnormalities and systemic repercussions.
- Psoriatic arthritis
Psoriasis is a skin ailment characterized by red, itchy, and scaly areas that can lead to the development of inflammatory arthritis. The symptoms of psoriatic arthritis include tenderness, edema, and stiffness in the affected joints.
Nails can also be affected, showing signs of change, including pitting and detachment.
- Gout
Gout is an inflammatory form of arthritis brought on by the buildup of uric acid crystals in the body's joints. A buildup can occur when uric acid is produced in large amounts or when it is not eliminated effectively.
The injured joint (often the big toe) turns red, swells up, and becomes extremely painful. Episodes of gout can come on suddenly and be very painful, although they often subside within a few days.
Other less common types of arthritis include:
- ankylosing spondylitis, a chronic inflammatory disease that majorly affects the spine;
- lupus arthritis, which occurs as a part of systemic lupus erythematosus;
- infectious arthritis, caused by bacteria, viruses, or fungi entering a joint.
Different forms of arthritis call for different approaches to treatment, depending on the etiology and severity of the condition. Medications to reduce inflammation, discomfort, and immune reactions may be employed, along with changes to one's diet, exercise routine, and body mass index (BMI).
In extreme circumstances, joint replacement surgery may be required to restore movement and relieve discomfort. Patients suffering from arthritis should seek the advice of medical experts to determine the cause of their condition and the best course of therapy.
Treatment Options for Pain Relief
Millions of people throughout the world suffer from arthritis, making their lives much more difficult and requiring treatment to alleviate the associated pain and distress. Fortunately, various treatments are available to help arthritis patients lessen their discomfort and lead better lives.
The two primary types of pain treatment are:
Medication for Pain Management
Treatment with medication is essential in the management of arthritic pain. They help with pain, inflammation, and disease progression; thus, doctors recommend them frequently.
Medication selection is condition- and patient-specific, taking into account such aspects as arthritis type and severity.
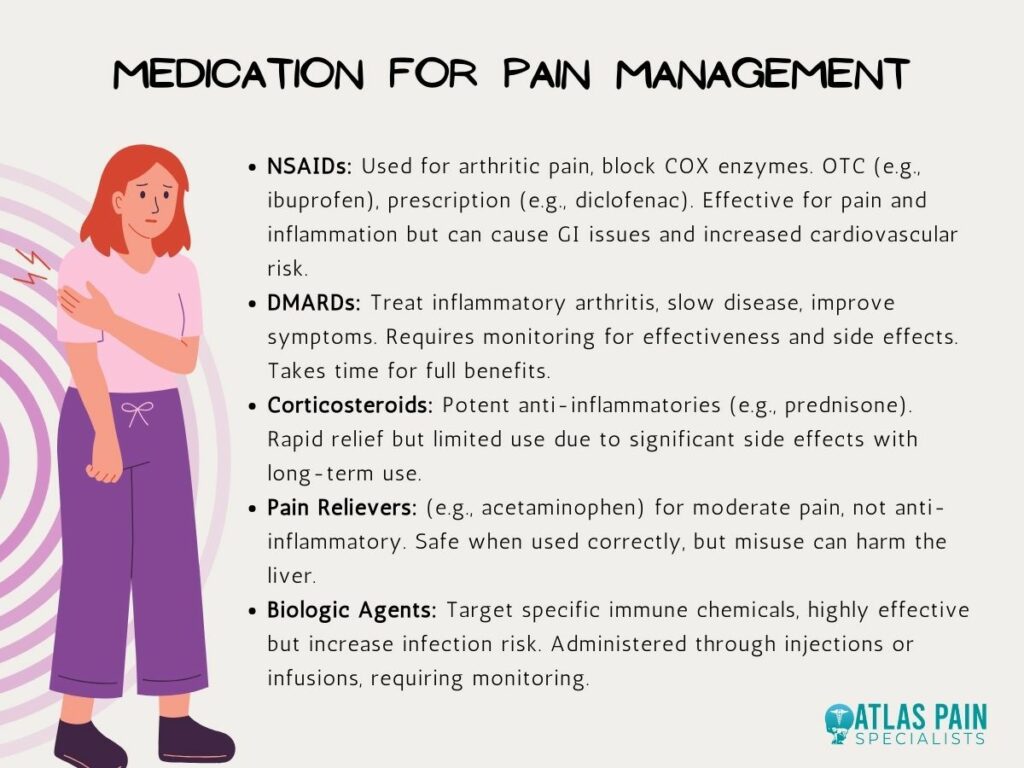
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
Anti-inflammatory drugs (NSAIDs) are commonly used to treat arthritic pain. They accomplish their anti-inflammatory and analgesic effects by blocking cyclooxygenase (COX) enzymes.
Nonsteroidal anti-inflammatory drugs (NSAIDs) come in both OTC and prescription varieties. Ibuprofen (Advil, Motrin) and naproxen (Aleve) are examples of over-the-counter NSAIDs, while NSAIDs like diclofenac and celecoxib, which require a prescription, provide more potent pain treatment.
Benefits:
- Effectively reduce pain and inflammation.
- Widely available and accessible.
- It can be used on an as-needed basis for pain flare-ups.
Considerations:
- Prolonged use of NSAIDs may lead to gastrointestinal side effects such as stomach ulcers and bleeding.
- Some NSAIDs may increase the risk of cardiovascular events, so their use should be discussed with a healthcare provider, especially for those with heart conditions.
2. Disease-Modifying Antirheumatic Drugs (DMARDs):
DMARDs are a group of drugs used to treat inflammatory forms of arthritis like rheumatoid and psoriatic. DMARDs aren't a quick fix for pain like NSAIDs are. Instead, they aim to alter the disease's progression by dampening the immune system's overreaction.
Benefits:
- Slow down the progression of arthritis by reducing joint damage.
- Improve overall symptoms, including pain, swelling, and joint stiffness.
- It may allow patients to achieve remission.
Considerations:
- Regular monitoring is essential to assess their effectiveness and watch for potential side effects, such as liver toxicity.
- It may take several weeks to months to experience the full benefits.
3. Corticosteroids:
Among the most effective anti-inflammatory drugs are corticosteroids like prednisone. They are commonly administered after other treatments have failed to alleviate severe arthritic symptoms.
Corticosteroids can be taken orally, injected into the afflicted joints, or used topically as capsules, creams, or ointments.
Benefits:
- Rapidly reduce inflammation and pain.
- It may be injected directly into inflamed joints for targeted relief.
Considerations:
- Long-term use of corticosteroids can lead to significant side effects, including weight gain, mood changes, osteoporosis, and increased infection risk.
- Their use is generally limited to short courses to minimize side effects.
4. Pain Relievers:
Acetaminophen (Tylenol) and similar pain medications can be tried for moderate arthritic pain. Although they don't have the anti-inflammatory qualities of NSAIDs, these drugs nonetheless provide welcome pain relief.
Benefits:
- Suitable for individuals who cannot tolerate NSAIDs due to stomach issues or cardiovascular concerns.
- Generally considered safe when used as directed.
Considerations:
- Overuse or exceeding recommended dosages can lead to liver damage, so careful adherence to dosing instructions is crucial.
5. Biologic Agents:
Inflammatory arthritis, such as rheumatoid arthritis and ankylosing spondylitis, is treated using a relatively new class of drugs called biologics. They go for particular immune system chemicals such as tumor necrosis factor (TNF), interleukin-6 (IL-6), and B cells.
Benefits:
- Highly effective at reducing inflammation and pain.
- It can lead to remission or significantly improved disease control.
Considerations:
- Administered through injections or infusions, which may require regular monitoring.
- Biologics can increase the risk of infections, so patients need to be vigilant for signs of illness.
Non-Medicinal Options
Although drugs are an important part of arthritis pain management, non-pharmaceutical methods can significantly impact patients' quality of life. Arthritis patients can benefit from these non-drug approaches, which attempt to lessen their pain, improve their range of motion, and improve their quality of life.
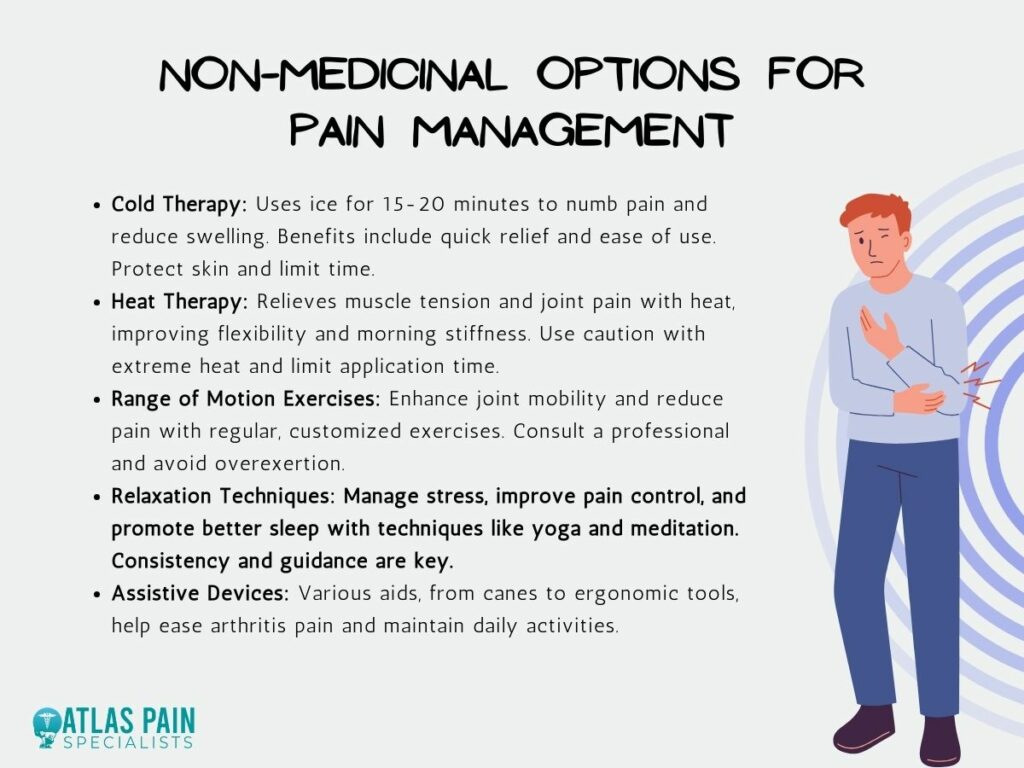
1. Ice Packs and Cold Therapy:
How it works: Applying a cold compress or ice pack to the affected area will quickly numb the pain and reduce inflammation. Pain and swelling can be reduced by using ice for 15-20 minutes at a time.
Make sure a towel or other fabric is between the cold object and your skin to prevent frostbite.
Benefits:
- Immediate Relief: Cold therapy provides quick relief from acute pain and inflammation.
- Reduces Swelling: It helps decrease swelling, relieving pressure on joints.
- Easy to Use: Ice packs are readily available and easy to apply.
Considerations:
- Protect the Skin: Always use a cloth or towel between the ice pack and the skin to prevent frostbite.
- Time Limits: Apply cold therapy for 15-20 minutes at a time, and allow the skin to return to normal temperature between applications.
2. Heating Pads and Hot Therapy:
How it works: On the flip side, heat therapy can reduce muscle tension and joint pain. Increasing blood flow to the afflicted area—through heating pads, warm baths, or warm towels—can alleviate arthritic pain.
Heat therapy is especially helpful when applied to osteoarthritis and other disorders involving muscle strain.
Benefits:
- Muscle Relaxation: Heat can relieve muscle tension and improve flexibility.
- Morning Stiffness: It's particularly beneficial for reducing morning stiffness often associated with arthritis.
- Comforting: Many people find the warmth soothing and comforting.
Considerations:
- Avoid Excessive Heat: Avoid extreme heat sources like hot water bottles or heating pads set on high to prevent burns.
- Limit Time: Apply heat for 15-30 minutes at a time.
3. Range of Motion Exercises:
How it works: Physical activity, especially light stretching and other range-of-motion exercises can help increase joint mobility and decrease pain when practiced on a regular basis. These moves are great for keeping your joints flexible and pain-free.
Get in touch with a physical therapist or rheumatologist to create an activity program suited to your unique case of arthritis.
Benefits:
- Improved Mobility: Regular exercises can increase the range of motion in affected joints.
- Pain Reduction: They help reduce pain by keeping joints mobile and preventing muscle atrophy.
- Enhanced Function: Exercises tailored to specific joints can improve daily function.
Considerations:
- Consult a Professional: Work with a physical therapist to develop a customized exercise plan for your arthritis type and individual needs.
- Avoid Overexertion: Avoid overexerting yourself, and stop any exercise that causes excessive pain.
4. Relaxation Techniques:
How it works: Arthritis pain can be made worse by stress and anxiety. Try some yoga, meditation, or deep breathing exercises to handle stress better and lessen the intensity of physical pain.
Additionally, it helps people go to sleep easier, which is important for controlling pain.
Benefits:
- Stress Reduction: Lowering stress levels can improve pain management and overall well-being.
- Better Sleep: Relaxation techniques can aid in achieving restful sleep, which is vital for managing pain.
Considerations:
- Regular Practice: Consistency is key; incorporate relaxation techniques into your daily routine for maximum benefit.
- Seek Guidance: Consider joining a mindfulness or meditation class or seeking guidance from a therapist or counselor for personalized techniques.
5. Assistive Devices for Arthritis:
Using these aids, people with arthritis can continue to do the things they enjoy while experiencing less pain and a greater degree of ease.
- Canes and Walkers: Single-point canes, quad canes, and walkers.
- Braces and Splints: Knee braces and wrist splints.
- Adaptive Kitchen Tools: Ergonomic utensils, jars, and bottle openers.
- Mobility Aids: Mobility scooters and manual wheelchairs.
- Reachers and Grabbers: Long-handled devices that help people with limited mobility reach and pick up objects without bending or stretching.
- Ergonomic Office Equipment: Ergonomic keyboards and mice, voice recognition software.
- Adaptive Gardening Tools: Ergonomic garden tools, garden kneelers, and seats.
- Adaptive Dressing Aids: Button hooks and zipper pulls, sock aids.
- Personal Care Aids: Long-handled shoehorns, specially designed toothbrushes.
How to Sleep Better When Living with Chronic Pain
To effectively manage the pain associated with arthritis, it is necessary to take a multifaceted strategy. Improving arthritis patients' quality of life requires close cooperation with healthcare specialists to create a personalized pain management plan.
Those dealing with persistent pain, such as arthritis pain, may find it difficult to get a good night's rest. It might be difficult to get to sleep and stay asleep when you're in pain.However, some methods and modifications to one's lifestyle can help alleviate arthritis-related pain and lead to better sleep. If you suffer from chronic pain from arthritis, read on to learn how to sleep better when living with chronic pain.
About Dr. Sean Ormond