
Nerve Ablation Costs: What You Need to Know Before Treatment
Nerve ablation is a medical procedure designed to alleviate chronic pain by destroying specific nerve tissues that transmit pain signals. This technique is often considered when other pain management methods have failed, providing relief for conditions such as lower back pain and arthritis.
However, potential patients should be aware of the associated nerve ablation costs, which can vary significantly depending on factors like the type of ablation performed and geographic location.
Types of Nerve Ablation
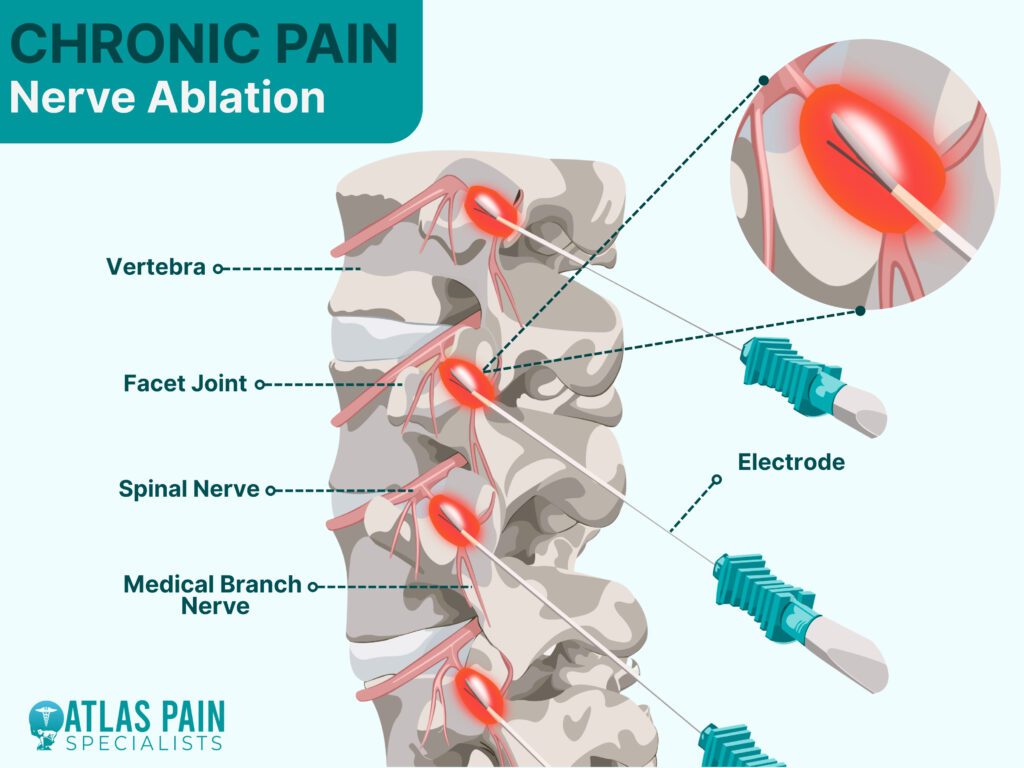
Nerve ablation is a medical procedure that disrupts nerve signals to relieve pain or treat various conditions. The two primary types of nerve ablation are Radiofrequency Ablation (RFA) and Laser Ablation.
| Type of Ablation | Description | Common Uses | Average Cost |
|---|---|---|---|
| Radiofrequency Ablation (RFA) | Uses heat from radio waves to destroy nerve tissues and block pain signals. | Chronic back pain, neck pain, arthritis, varicose veins, cardiac arrhythmias. | $3,000 - $30,000 (varies by procedure type) |
| Laser Ablation | Uses concentrated light energy to remove or destroy nerve tissue. | Varicose veins, some nerve pain, tumor removal. | $1,000 - $2,500 |
| Cryoablation | Freezes nerve tissues to stop pain signals. | Neuropathy, chronic pain, tumors. | $3,500 - $7,000 |
| Ultrasound-Guided Ablation | Uses ultrasound waves to target nerves and alleviate pain. | Chronic pain, cancer pain management. | $5,000 - $15,00 |
1. Radiofrequency Ablation (RFA)
RFA uses heat generated from radio waves to target and destroy specific nerve tissues, preventing them from transmitting pain signals. This technique is commonly used for chronic pain conditions such as arthritis, back pain, and neck pain.
It is also used for treating varicose veins and even certain types of tumors. RFA is minimally invasive, performed on an outpatient basis, and offers longer-lasting pain relief compared to steroid injections.
2. Laser Ablation
Laser ablation involves using highly focused light energy to destroy nerve tissue or unwanted blood vessels. It is commonly used for pain management, treating varicose veins, and even for neurological conditions.
Compared to RFA, laser ablation is less frequently used for nerve pain but is highly effective for specific applications, such as vein treatments. The procedure is also minimally invasive and has a relatively quick recovery period.
Cost Overview
The cost of nerve ablation varies depending on the procedure, location, and provider. On average, the cost of radiofrequency ablation is around $5,411 per procedure, while laser ablation typically costs between $1,000 and $2,500.
Specific Procedures and Their Costs
- Cervical Radiofrequency Ablation: This procedure targets nerves in the neck and typically costs around $3,195 per treated level. It is commonly used for chronic neck pain caused by arthritis or disc degeneration.
- Varicose Veins RFA: Treating varicose veins with radiofrequency ablation generally costs between $2,000 and $4,500, depending on the number of veins treated and whether the procedure is performed in a hospital or clinic setting.
- Cardiac Radiofrequency Ablation: This is a more complex procedure used to treat abnormal heart rhythms (arrhythmias). Due to the high level of expertise and hospital resources required, the cost ranges from $25,000 to $30,000.
- Liver Radiofrequency Ablation: Liver RFA is used to treat certain types of liver tumors, particularly in patients who are not candidates for surgery. The procedure costs between $15,000 and $20,000, depending on the hospital and specific treatment plan.
Factors Influencing Cost
The cost of nerve ablation procedures, whether radiofrequency ablation (RFA) or laser ablation, is influenced by multiple factors. These include the type of procedure, location, medical facility, physician expertise, insurance coverage, and additional expenses such as follow-up care.
1. Type of Procedure and Complexity
The specific nerve ablation technique and the area being treated play a significant role in determining cost.
Simple procedures like laser ablation for varicose veins typically cost less, ranging from $1,000 to $2,500, whereas more complex procedures like cardiac RFA can cost upwards of $25,000 to $30,000. The difference in cost arises from the complexity of the condition being treated, the precision required, and the level of medical expertise involved.
2. Geographic Location
Medical costs vary widely based on geographic region. In major metropolitan areas or high-cost-of-living states, procedures tend to be more expensive due to higher facility fees and physician charges.
For example, nerve ablation in New York City or Los Angeles might cost significantly more than in a smaller city or rural area. International cost differences exist, with some countries offering nerve ablation procedures at a fraction of the cost found in the United States due to lower healthcare costs and different medical regulations.
3. Hospital vs. Outpatient Clinic
The choice of treatment facility also impacts cost. Procedures performed in hospitals tend to be more expensive than those done in outpatient clinics or specialized pain management centers.
Hospital-based procedures come with additional facility fees, anesthesia costs, and longer recovery monitoring, which drive up the total expense. Outpatient centers are often more cost-effective for less complex procedures, such as cervical RFA for neck pain.
4. Physician Expertise and Specialization
Specialists with extensive experience and board certification often charge higher fees. For instance, an interventional pain specialist with decades of experience may charge more than a general practitioner performing the same procedure.
While a highly experienced physician may charge more, their expertise often reduces complications, enhances precision, and improves patient outcomes, which can be cost-effective in the long run.
5. Insurance Coverage and Out-of-Pocket Costs
Insurance significantly impacts the final cost patients pay. Many insurance plans cover nerve ablation when deemed medically necessary, such as for chronic pain management or cardiac arrhythmias.
However, coverage varies, and patients may still be responsible for copayments, deductibles, and out-of-pocket costs. Without insurance, patients often face the full cost of the procedure, which can be a significant financial burden.
6. Additional Expenses
Beyond the procedure itself, patients may encounter additional costs such as pre-procedure consultations, imaging (MRI or CT scans), post-procedure medications, follow-up appointments, and physical therapy if needed.
These can add hundreds or even thousands of dollars to the overall expense. For example, a patient undergoing radiofrequency ablation for chronic back pain may need multiple sessions, leading to cumulative costs over time.
Economic Analysis and Cost-Effectiveness
Nerve ablation procedures are often evaluated not just by their upfront costs but by their cost-effectiveness in the long run. While nerve ablation can be expensive, it is frequently considered a financially viable option compared to alternative treatments, particularly for chronic pain and cardiovascular conditions.
1. Comparing Costs to Alternative Treatments
For chronic pain patients, common alternatives to nerve ablation include opioid medications, physical therapy, corticosteroid injections, and surgery. Each of these has its own cost structure and long-term financial implications:
- Opioid Medications: While pain medications seem inexpensive at first, long-term use can become costly and lead to complications such as dependency or tolerance, requiring higher doses over time. The indirect costs of opioid dependence, including lost productivity and additional healthcare expenses, can far exceed the cost of nerve ablation.
- Physical Therapy: PT is often recommended for pain management, but multiple sessions over months or years can add up to thousands of dollars. Additionally, some patients do not experience long-term relief, making nerve ablation a more effective option in certain cases.
- Steroid Injections: While injections may provide temporary relief, they often require multiple treatments over time, which increases long-term costs without offering permanent pain resolution.
- Surgery: Compared to spinal surgery or joint replacement, which can cost $50,000 or more, nerve ablation is significantly cheaper and carries fewer risks. Many patients opt for nerve ablation as a minimally invasive and cost-effective alternative to surgery.
2. Long-Term Savings and Patient Benefits
A major advantage of radiofrequency ablation (RFA) for chronic pain is that it can provide relief lasting 6 to 18 months, sometimes longer. Compared to repetitive injections or daily medication, this reduces healthcare costs over time. For patients who undergo RFA every 12 to 18 months, the annual cost may be lower than the cumulative expenses of medications, physical therapy, or frequent doctor visits.
| Treatment | Duration of Effectiveness | Estimated Cost Over 5 Years |
|---|---|---|
| RFA (every 12-18 months) | 6-18 months | $6,000 - $15,000 |
| Steroid Injections (every 3 months) | 2-3 months | $10,000 - $25,000 |
| Opioid Medications (daily use) | Short-term relief | $12,000 - $18,000 |
| Spinal Surgery (one-time) | Permanent (if successful) | $50,000+ |
For varicose vein treatment, laser ablation is often preferred over sclerotherapy or surgical vein stripping because it is minimally invasive, has a quicker recovery time, and eliminates the need for repeated interventions. Even though the initial cost of $1,000 to $2,500 may seem high, it prevents future complications such as ulcers, swelling, or blood clots, reducing the need for additional medical care.
3. Cost-Effectiveness of Cardiac and Liver Ablation
Cardiac RFA, despite its high cost of $25,000 to $30,000, is considered a cost-effective solution for treating arrhythmias compared to long-term antiarrhythmic drug therapy or implantable cardiac devices. By eliminating abnormal heart rhythms, patients reduce their risk of hospitalization, stroke, and emergency interventions, ultimately saving money in the long term.
Similarly, liver RFA for tumor treatment is cost-effective when surgical removal is not an option. While $15,000 to $20,000 may seem expensive, it offers a minimally invasive alternative to surgery, reducing hospital stays and recovery times, making it a financially viable choice for many patients.
4. Quality of Life and Indirect Savings
Beyond direct medical costs, nerve ablation improves the quality of life, work productivity, and mobility. Chronic pain can lead to missed workdays, reduced earning potential, and emotional distress, all of which come with economic consequences.
By providing long-term pain relief, nerve ablation allows patients to return to work, engage in daily activities, and avoid costly disability claims or mental health treatments.
The Benefits of Radiofrequency Ablation for Chronic Back Pain
Radiofrequency ablation offers a promising solution for individuals suffering from chronic back pain, providing significant relief and improving quality of life. While the procedure can be highly effective, it’s essential to consider the associated costs and insurance coverage options to ensure you’re making a financially sound decision.
By weighing the benefits against the expenses, you can better prepare for this treatment. Always consult with your healthcare provider to discuss your specific situation and explore all available pain management options. With the right approach, you can regain control over your pain and enhance your overall well-being.
About Dr. Sean Ormond



