
What is Peripheral Arterial Disease (PAD)?
Peripheral Arterial Disease (PAD) affects millions worldwide, yet its impact often goes unrecognized. This silent condition, characterized by narrowed arteries in the limbs, can lead to serious complications if left untreated.
In this blog post, we'll delve into the intricacies of PAD, exploring its causes, symptoms, diagnostic methods, and treatment options. By increasing awareness and understanding of PAD, we aim to empower individuals to recognize the signs, seek timely medical intervention, and make informed lifestyle choices to manage this condition effectively.
What is Peripheral Arterial Disease (PAD)?
Peripheral Arterial Disease (PAD) is a circulatory condition characterized by narrowed arteries that reduce blood flow to the limbs, typically the legs. This narrowing, often caused by atherosclerosis, inflammation, injury, or radiation exposure, results in decreased oxygen and nutrient supply to the affected tissues. PAD is associated with various risk factors including diabetes, smoking, obesity, high blood pressure, and high cholesterol levels.
Symptoms of PAD
PAD manifests through a range of symptoms, reflecting the compromised blood flow to the lower extremities:
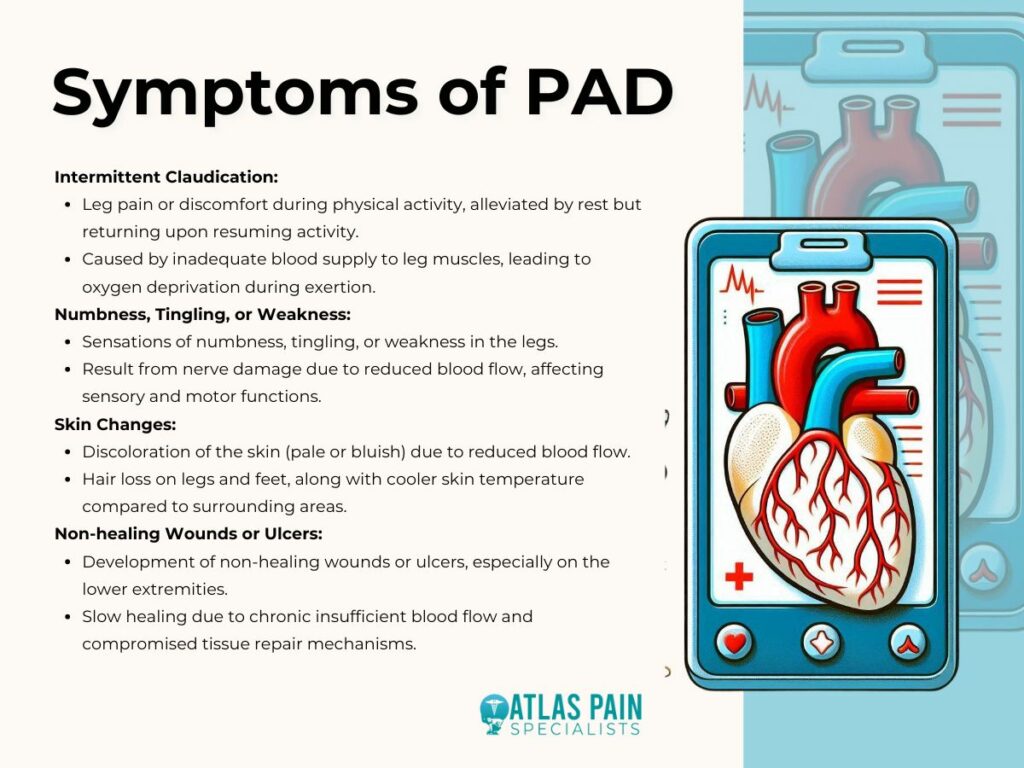
- Intermittent Claudication: One of the hallmark symptoms of PAD is intermittent claudication, which refers to leg pain or discomfort that occurs during physical activity, particularly walking. This pain typically subsides with rest but recurs upon resuming activity. It stems from inadequate blood supply to the leg muscles, leading to oxygen deprivation during exertion.
- Numbness, Tingling, or Weakness: Patients with PAD may experience sensations of numbness, tingling, or weakness in their legs. These sensations often indicate nerve damage due to reduced blood flow, leading to impaired sensory and motor functions.
- Skin Changes: PAD can cause noticeable changes in the skin of the legs and feet. These changes may include discoloration, where the skin appears pale or bluish due to reduced blood flow. Additionally, patients may experience hair loss on the legs and feet, as well as alterations in skin temperature, which can feel cooler than the surrounding areas.
- Non-healing Wounds or Ulcers: Chronic insufficient blood flow in PAD can result in the development of non-healing wounds or ulcers, particularly on the lower extremities. These wounds may appear as open sores or ulcers on the feet or toes and are often slow to heal due to compromised tissue repair mechanisms.
Diagnosing PAD
Diagnosing Peripheral Arterial Disease (PAD) involves a comprehensive evaluation combining various clinical assessments and specialized tests to confirm the presence and severity of the condition.
Physical Exam and Medical History
The initial step in diagnosing PAD typically involves a thorough physical examination and a detailed medical history review. During the physical exam, a healthcare provider may assess the patient's pulses in the affected limbs, looking for weak or absent pulses, which can indicate reduced blood flow. They may also examine the patient's legs for signs of skin changes, such as discoloration or ulcers, and evaluate any symptoms reported by the patient, such as leg pain or numbness.
A comprehensive medical history review helps identify potential risk factors for PAD, such as diabetes, smoking, hypertension, and hyperlipidemia. Understanding the patient's medical history provides valuable insights into their overall health status and aids in determining the likelihood of PAD.
Ankle-Brachial Index (ABI) Test
The Ankle-Brachial Index (ABI) test is a non-invasive diagnostic tool used to assess blood flow and detect arterial obstruction in the lower extremities. During the ABI test, blood pressure measurements are taken at the ankles and compared to blood pressure measurements taken at the arms (brachial arteries).
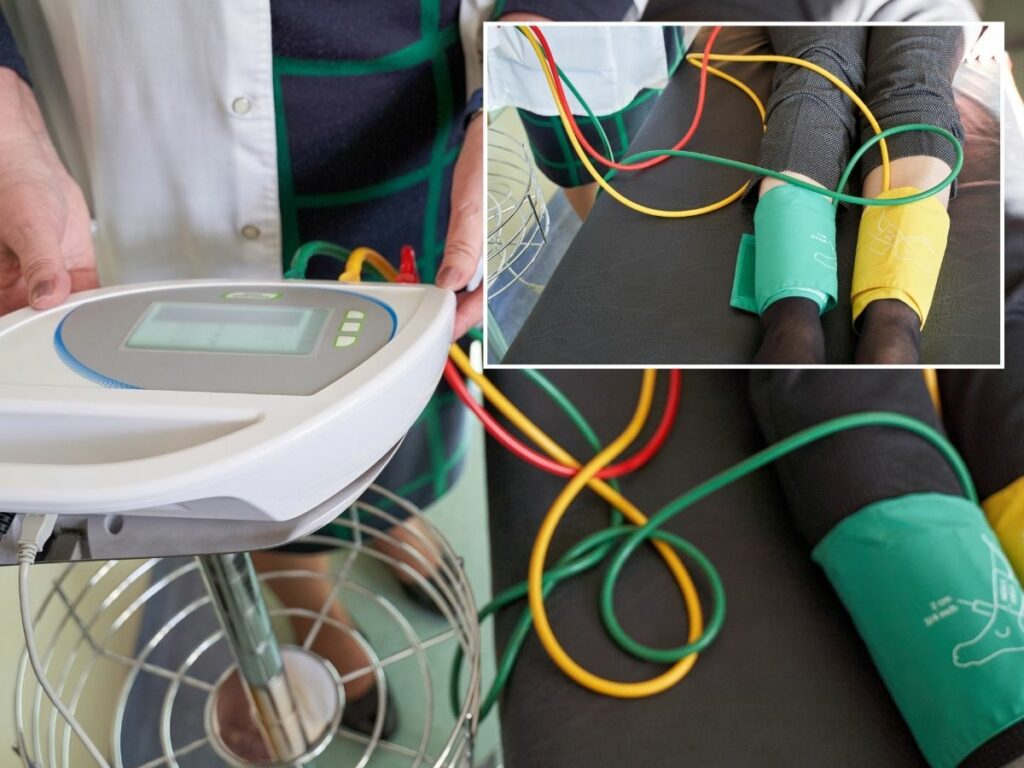
A ratio of the ankle systolic blood pressure to the brachial systolic blood pressure is calculated, with lower ratios indicating poorer arterial circulation. An ABI value of less than 0.90 is generally considered abnormal and indicative of PAD. This simple and cost-effective test is often performed in a clinical setting and provides valuable information about the severity of arterial obstruction in the lower limbs.
Imaging Tests
Imaging tests play a crucial role in diagnosing PAD by providing detailed anatomical information about the arterial system and identifying areas of stenosis or occlusion. Two common imaging modalities used in the diagnosis of PAD include ultrasound and angiography.
Ultrasound
Ultrasound imaging, also known as duplex ultrasonography, utilizes high-frequency sound waves to visualize blood flow within the arteries and assess the presence of arterial narrowing or blockages. This non-invasive technique provides real-time images of the blood vessels, allowing healthcare providers to evaluate blood flow velocity, detect plaque buildup, and identify any abnormalities in the arterial walls.

Ultrasound is particularly useful for assessing the severity and location of arterial lesions and guiding treatment decisions, such as determining the suitability for endovascular interventions like angioplasty or stenting.
Angiography
Angiography is a more invasive imaging procedure that involves the injection of a contrast dye into the arterial system followed by X-ray imaging to visualize the blood vessels. This technique provides detailed images of the arterial anatomy, including the location and extent of arterial blockages.
Peripheral angiography can be performed using conventional X-ray angiography or newer techniques such as magnetic resonance angiography (MRA) and computed tomography angiography (CTA). These advanced imaging modalities offer high-resolution images of the arterial vasculature and help guide treatment planning for patients with PAD.

Stages of PAD
Peripheral Arterial Disease (PAD) is often classified into stages based on the severity of symptoms and the degree of arterial obstruction. Two commonly used staging systems for PAD are the Fontaine and Rutherford classifications.
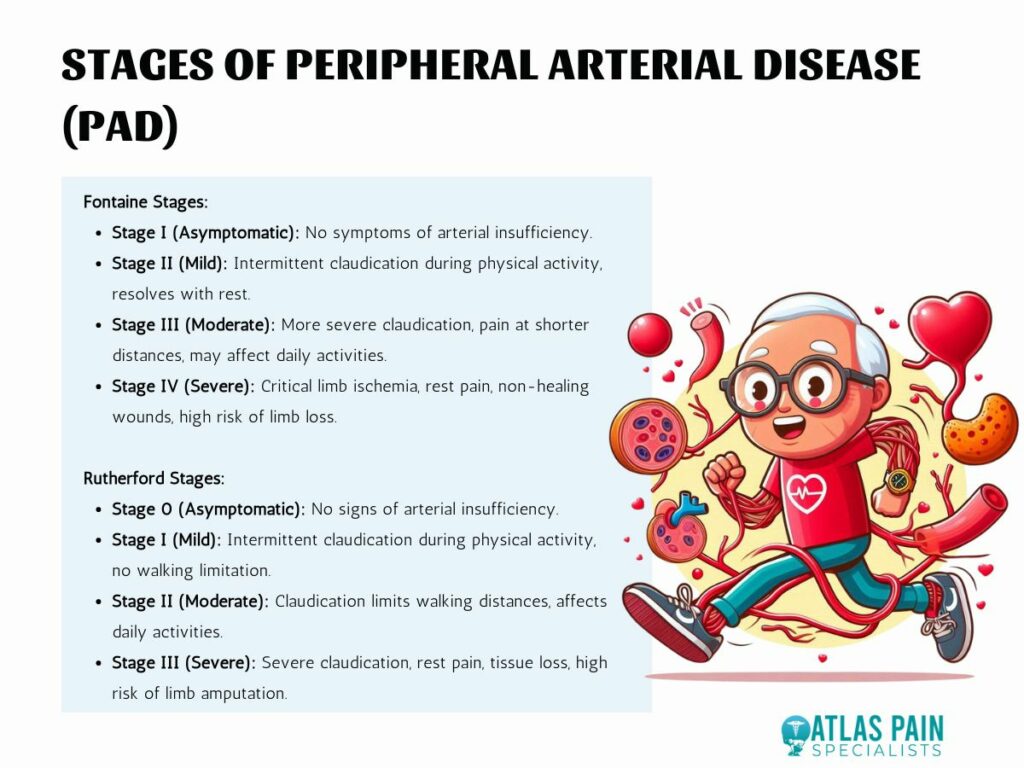
Fontaine Stages
The Fontaine classification system categorizes PAD into four stages based on the presence and severity of symptoms:
- Stage I (Asymptomatic): Patients with Stage I PAD are asymptomatic and do not experience any symptoms of arterial insufficiency.
- Stage II (Mild): Stage II PAD is characterized by intermittent claudication, where patients experience leg pain, cramping, or discomfort during physical activity. Symptoms typically resolve with rest.
- Stage III (Moderate): In Stage III PAD, patients experience more severe intermittent claudication, with pain occurring at shorter walking distances and potentially affecting their daily activities.
- Stage IV (Severe): Stage IV PAD is characterized by critical limb ischemia, where patients experience rest pain, non-healing wounds or ulcers, and tissue necrosis. Severe arterial obstruction puts patients at high risk of limb loss and requires immediate medical intervention.
Rutherford Stages
The Rutherford classification system also divides PAD into four stages based on the severity of symptoms and tissue damage:
- Stage 0 (Asymptomatic): Patients with Stage 0 PAD are asymptomatic and do not exhibit any signs of arterial insufficiency.
- Stage I (Mild): Stage I PAD is characterized by mild claudication, where patients experience intermittent leg pain or discomfort during physical activity but can walk without limitation.
- Stage II (Moderate): In Stage II PAD, patients experience moderate claudication, with pain occurring at shorter walking distances and potentially limiting their daily activities.
- Stage III (Severe): Stage III PAD is marked by severe claudication, rest pain, and tissue loss, indicating critical limb ischemia. Patients are at high risk of limb amputation without prompt intervention.
The Fontaine and Rutherford staging systems provide valuable frameworks for assessing the severity of PAD and guiding treatment decisions based on the patient's clinical presentation and functional status. Early diagnosis and appropriate management are essential for optimizing outcomes and reducing the risk of complications associated with PAD.
Complications of Untreated PAD
Untreated Peripheral Arterial Disease (PAD) can lead to various complications, posing significant risks to an individual's health and well-being.
Increased Risk of Heart Attack and Stroke
PAD shares common risk factors and underlying mechanisms with coronary artery disease (CAD) and cerebrovascular disease, increasing the likelihood of heart attacks and strokes. The atherosclerotic plaques responsible for narrowing peripheral arteries can also affect the coronary arteries supplying the heart and the carotid arteries supplying the brain. Consequently, individuals with untreated PAD are at a heightened risk of developing myocardial infarction (heart attack) and ischemic stroke.


Limb Amputation due to Severe Tissue Damage
In advanced cases of PAD, severe and prolonged arterial insufficiency can result in critical limb ischemia (CLI), a condition characterized by inadequate blood flow to the affected limb. CLI can lead to tissue necrosis, non-healing wounds, and gangrene, significantly increasing the risk of limb amputation. Without timely intervention and revascularization procedures to restore blood flow, the risk of limb loss becomes substantial, profoundly impacting an individual's mobility and quality of life.

Treatment Options for PAD
Effective management of Peripheral Arterial Disease (PAD) focuses on relieving symptoms, improving vascular health, and reducing the risk of complications through a multidisciplinary approach.
Lifestyle Changes
Lifestyle modifications play a fundamental role in PAD management and often form the cornerstone of treatment. Key lifestyle changes include:
- Smoking Cessation: Quitting smoking is crucial for patients with PAD as smoking exacerbates arterial narrowing and impairs blood flow, significantly increasing the risk of complications.
- Exercise: Regular physical activity, particularly walking exercises, can improve arterial blood flow, enhance exercise tolerance, and alleviate symptoms of intermittent claudication.
- Diet: Adopting a heart-healthy diet low in saturated fats, cholesterol, and sodium can help manage PAD risk factors such as hypertension and dyslipidemia, promoting overall cardiovascular health.
Medications
Pharmacological interventions are commonly prescribed to manage PAD and its associated risk factors:
- Antiplatelet Drugs: Medications such as aspirin or clopidogrel are often prescribed to reduce the risk of blood clot formation and cardiovascular events in patients with PAD.
- Cholesterol-Lowering Drugs: Statins are widely used to lower cholesterol levels and stabilize atherosclerotic plaques, slowing the progression of PAD and reducing the risk of cardiovascular events.
Endovascular Procedures
Endovascular interventions are minimally invasive procedures performed to improve blood flow in obstructed arteries:
- Angioplasty: During angioplasty, a catheter with a small balloon at its tip is inserted into the narrowed artery and inflated to widen the vessel, restoring blood flow.
- Stenting: In some cases, a stent—a small mesh tube—is inserted into the artery during angioplasty to help keep it open and prevent re-narrowing (restenosis).
Surgical Interventions
In cases where endovascular procedures are not feasible or effective, surgical interventions may be necessary:
- Bypass Surgery: Bypass surgery involves creating a new pathway for blood flow by grafting a healthy blood vessel from another part of the body or using a synthetic graft to bypass the obstructed artery, restoring adequate circulation to the affected limb.
The choice of treatment modality depends on various factors, including the severity of PAD, the extent of arterial obstruction, the patient's overall health status, and their treatment goals. A personalized treatment plan tailored to the individual's needs and preferences is essential for optimizing outcomes and improving long-term prognosis in PAD management.
Conclusion
Peripheral Arterial Disease (PAD) is a significant vascular condition that demands attention and proactive management. By understanding its causes, recognizing its symptoms, and seeking prompt diagnosis and treatment, individuals can mitigate the risks of complications such as heart attack, stroke, and limb amputation.
Lifestyle modifications, medications, and interventional procedures offer avenues for improving vascular health and enhancing quality of life for those affected by PAD. With awareness and action, we can combat PAD and its detrimental effects, promoting better cardiovascular outcomes and overall well-being.
About Dr. Sean Ormond