
Understanding Opioid Therapy for Chronic Pain
Living with chronic pain can be stressful, affecting every aspect of a person's life, from their physical well-being to their emotional and psychological health. Opioid therapy has long been recognized as a cornerstone in managing chronic pain, offering relief and restoring functionality to those who struggle daily with persistent discomfort.
However, the complexities surrounding opioid therapy extend beyond its pain-relieving benefits. The decision to undergo opioid therapy for chronic pain is not one to be taken lightly, as it requires a comprehensive understanding of the benefits and risks involved, as well as a commitment to careful management and monitoring.
The Benefits of Opioid Therapy
Opioid therapy stands as a pillar in the management of chronic pain, offering individuals relief from persistent discomfort that may otherwise severely impact their quality of life.

1. Effective Pain Relief
Opioids are potent analgesic medications that act on the body's opioid receptors to alleviate pain. Unlike many other pain medications, opioids have a unique ability to provide substantial relief, even in cases of severe or refractory pain.
Opioids efficiently reduce pain by attaching to opioid receptors in the brain and spinal cord to alter pain perception and transmission. This analgesic effect is especially helpful for people with chronic pain issues when typical pain treatment techniques may not be effective, such as neuropathic pain, cancer-related pain, or musculoskeletal ailments.
2. Improved Quality of Life
Chronic pain not only causes physical discomfort but also takes a toll on an individual's emotional and psychological well-being, leading to decreased quality of life. Opioid therapy has been shown to significantly enhance the overall quality of life for many individuals living with chronic pain.
Opioids allow patients to participate more completely in everyday activities, social interactions, and recreational pursuits that may have been restricted by pain by effectively lowering pain severity and frequency. Furthermore, the pain relief that opioid medication offers can have a profound impact on mental health, reducing the symptoms of anxiety, stress, and depression related to chronic pain.
3. Increased Functionality and Mobility
The ability of opioid therapy to help people with chronic pain regain their mobility and functionality is one of its main advantages. Opioids allow patients to resume activities of daily life, such as walking, standing, and doing housework, with more ease and comfort as they lessen physical limits and pain.
This restoration of functionality is essential for preserving independence and autonomy, allowing individuals to maintain a sense of normalcy in their lives. Furthermore, opioid therapy can facilitate participation in rehabilitative efforts aimed at improving strength, flexibility, and range of motion.
Administration Methods to Prevent Side Effects
Effective administration of opioid therapy is essential not only for optimizing pain relief but also for minimizing the risk of adverse effects that may accompany its use. Proper dosing, monitoring, and adherence to safe prescribing practices are critical in preventing or mitigating potential side effects associated with opioids
1. Proper Dosage and Monitoring
One of the primary considerations in opioid therapy is ensuring that patients receive the appropriate dosage based on their individual pain levels, medical history, and tolerance to opioids. Starting with the lowest effective dose and titrating gradually based on the patient's response is crucial for preventing overdose and minimizing side effects.
Regular monitoring of patients receiving opioid therapy is essential for detecting signs of inadequate pain control, medication misuse, or adverse reactions. Monitoring may include periodic assessments of pain intensity, functional status, and medication adherence, as well as screening for signs of opioid-related side effects such as constipation, sedation, or respiratory depression.
2. Slow Titration and Careful Adjustment
The principle of "start low and go slow" applies to opioid therapy, particularly when initiating treatment or adjusting dosage levels. Slow titration allows patients to acclimate to the effects of opioids gradually, reducing the likelihood of adverse reactions such as sedation, nausea, or dizziness.
Patients transitioning from short-acting to long-acting opioid formulations or vice versa require careful adjustment of dosage to maintain optimal pain control while minimizing side effects. Individualized treatment plans tailored to the patient's specific needs and circumstances are essential for optimizing the safety and efficacy of opioid therapy.
3. Use of Extended-Release Formulations
Extended-release (ER) or long-acting (LA) opioid formulations offer several advantages over immediate-release (IR) formulations in terms of both efficacy and safety. ER/LA opioids provide sustained pain relief over an extended period, allowing for less frequent dosing and improved medication adherence.
ER/LA formulations help reduce changes in pain intensity and lower the likelihood of breakthrough pain and opioid-related adverse effects by maintaining stable plasma concentrations of opioids. In addition, because of their longer onset of action and tamper-resistant characteristics, ER/LA opioids are less likely to be abused and diverted than IR formulations.
4. Avoidance of Concurrent Sedative Medications
Concurrent use of opioids with other sedative medications, such as benzodiazepines, muscle relaxants, or certain antidepressants, can potentiate central nervous system depression and increase the risk of respiratory depression, sedation, and overdose.
Whenever possible, alternative non-sedating medications or non-pharmacological approaches should be considered to minimize the risk of adverse drug interactions and respiratory complications.
5. Individualized Treatment Plans and Risk Stratification
Opioid therapy should be individualized based on the patient's unique characteristics, including age, comorbidities, concurrent medications, genetic factors, and history of substance abuse or mental health disorders. High-risk patients may require closer monitoring, lower initial doses, and more frequent follow-up visits to ensure their safety and well-being.
When starting opioid medication, healthcare professionals should also involve patients in shared decision-making, going over the advantages, disadvantages, and alternatives to opioids depending on the patient's preferences and treatment objectives. Better treatment outcomes and patient satisfaction are patient-centered care's ultimate goals, which strongly emphasize cooperation, openness, and respect for the patient's autonomy in making decisions.
The Side Effects of Opioid Therapy
Opioids can elicit a range of adverse effects that may impact physical, emotional, and psychological well-being. Identifying the underlying causes of opioid-related side effects is essential for implementing targeted interventions to manage symptoms effectively while minimizing the risk of complications.
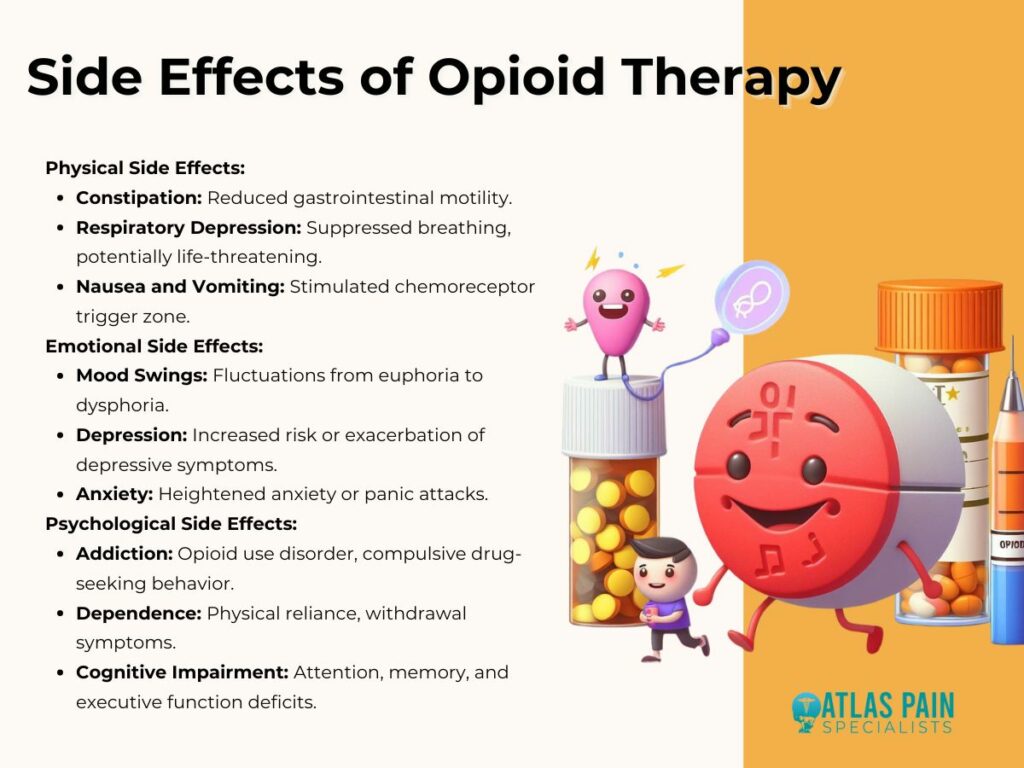
1. Physical Side Effects
- Constipation: Opioids bind to opioid receptors in the gastrointestinal tract, leading to decreased gastrointestinal motility and constipation. This common side effect can significantly impact patients' quality of life and adherence to opioid therapy.
- Respiratory Depression: High doses of opioids can suppress respiratory drive, leading to shallow or slow breathing and potentially life-threatening respiratory depression. Respiratory depression is a serious concern, particularly in patients with underlying respiratory conditions or those receiving concurrent sedative medications.
- Nausea and Vomiting: Opioids can stimulate the chemoreceptor trigger zone in the brain, resulting in nausea and vomiting, especially during initiation of therapy or dose escalation. Antiemetic medications may be prescribed to alleviate these symptoms and improve medication tolerance.
2. Emotional Side Effects
- Mood Swings: Opioids can affect neurotransmitter systems involved in mood regulation, leading to mood fluctuations ranging from euphoria to dysphoria. Patients may experience emotional instability, irritability, or mood swings while on opioid therapy.
- Depression: Prolonged opioid use has been associated with an increased risk of developing depression or exacerbating pre-existing depressive symptoms. The neurobiological mechanisms underlying this association are complex and may involve alterations in neurotransmitter signaling and neuroplasticity.
- Anxiety: Some individuals may experience heightened anxiety or panic attacks while taking opioids, particularly during periods of dose adjustment or withdrawal. Anxiety-related side effects can be distressing and may necessitate adjustments to the opioid regimen or adjunctive treatment with anxiolytic medications.
3. Psychological Side Effects
- Addiction: Opioid use disorder (OUD) is a significant concern associated with long-term opioid therapy, characterized by compulsive drug-seeking behavior, loss of control over drug use, and continued use despite adverse consequences. Genetic predisposition, environmental factors, and neurobiological changes contribute to the development of addiction.
- Dependence: Physical dependence on opioids can occur with prolonged use, leading to withdrawal symptoms upon abrupt discontinuation or dose reduction. Tolerance, the need for escalating doses to achieve the same level of pain relief, is also a hallmark of opioid dependence.
- Cognitive Impairment: Chronic opioid use has been linked to cognitive impairment, including deficits in attention, memory, and executive function. These cognitive side effects can impair daily functioning and quality of life, particularly in elderly patients or those with pre-existing cognitive deficits.
Combining Opioid Therapy with Other Modalities
While opioid therapy can be effective in managing chronic pain, a multimodal approach that combines opioids with other treatment modalities offers several advantages, including enhanced pain relief, reduced opioid requirements, and a lower risk of adverse effects. Integrating non-pharmacological therapies, interventional procedures, and complementary modalities with opioid therapy allows for a more comprehensive and individualized approach to pain management.

1. Multimodal Approach to Pain Management
- Comprehensive Pain Relief: Combining opioids with non-opioid medications, such as NSAIDs, acetaminophen, or adjuvant analgesics, can provide synergistic pain relief by targeting different pain pathways and mechanisms. Multimodal analgesia allows for lower opioid doses, reducing the risk of opioid-related adverse effects while maximizing pain control.
- Addressing Multifactorial Pain: Chronic pain is often multifactorial, involving physical, psychological, and social dimensions. A multimodal approach that addresses these various aspects of pain can lead to more holistic and effective pain management outcomes. Incorporating interventions such as physical therapy, cognitive-behavioral therapy (CBT), and mindfulness-based techniques can help patients develop coping skills, improve functional outcomes, and reduce reliance on opioids for pain relief.
2. Integration of Non-pharmacological Therapies
- Physical Therapy: Physical therapy plays a crucial role in pain management by improving strength, flexibility, and mobility, reducing musculoskeletal pain, and promoting overall physical function. Exercise-based interventions, manual therapy techniques, and modalities such as heat or cold therapy can complement opioid therapy by addressing underlying musculoskeletal dysfunction and promoting tissue healing.
- Cognitive-Behavioral Therapy (CBT): CBT is a psychotherapeutic approach that focuses on modifying maladaptive thoughts, beliefs, and behaviors associated with pain. By teaching patients coping skills, relaxation techniques, and stress management strategies, CBT can help reduce pain intensity, improve mood, and enhance overall coping abilities, thereby reducing the need for opioids and minimizing the risk of psychological side effects.
3. Minimizing Side Effects through Complementary Treatments
- Adjunctive Medications: Certain medications, such as antidepressants, anticonvulsants, or muscle relaxants, can augment the analgesic effects of opioids and target specific pain mechanisms, such as neuropathic pain or muscle spasms. Adding adjunctive medications to opioid therapy can improve pain relief, reduce opioid requirements, and mitigate the risk of opioid-related side effects.
- Integrative Therapies: Integrative therapies, including acupuncture, massage therapy, chiropractic care, and biofeedback, offer additional avenues for pain management while minimizing reliance on opioids. These modalities can modulate pain perception, promote relaxation, and enhance overall well-being, providing patients with alternative strategies for managing pain and improving quality of life.
Are Alternative Pain Management Techniques Effective?
Even though opioids can be quite helpful for those with chronic pain, there are risks and restrictions associated with them that should be carefully considered and closely monitored. We can maximize treatment success while lowering the danger of side effects by understanding the advantages of opioid therapy, putting safe delivery techniques into practice, and investigating coping mechanisms and substitutes.
The inclusion of alternative pain management approaches in an opioid treatment plan is important in delivering patient-centered, holistic care. This conversation naturally led to the question, "Are Alternative Pain Management Techniques Effective?" which encourages additional research into complementary therapies, interventional techniques, and non-pharmacological interventions that provide effective substitutes for opioids.
Through fostering communication across traditional and non-traditional pain care modalities, patients have a more customized and varied toolkit to manage their pain and reduce their dependency on opioids.
About Dr. Sean Ormond



