
The Importance of Early Intervention in Pain Management
Pain, both acute and chronic, is a universal human experience that significantly influences one's quality of life. The timeliness of intervention in managing pain is a critical factor in determining the trajectory of an individual's health and well-being. So, What is the importance of early intervention in pain management?
We have all been there before…attempting to do something and ending up with pain or an injury. Anything from a strained ankle to your lower back "throwing out... "Do you always know what to do when these ridiculous problems happen? Did you know that you can speed up your recovery by scheduling an evaluation with your pain management doctor right away?
The importance of addressing pain at its onset cannot be overstated, as timely and targeted interventions not only provide relief but also play a pivotal role in preventing long-term complications. Our overarching goal is to underscore the significance of early intervention in pain management for individuals, healthcare professionals, and the broader healthcare system.
Table of Contents
What Is Early Intervention Therapy?
Failing to address pain promptly can lead to a cascade of adverse consequences, impacting both physical and psychological well-being. When left unmanaged, acute pain has the potential to transition into a chronic state, creating persistent discomfort and diminishing an individual's quality of life.
Early intervention in pain management refers to the prompt identification and treatment of pain symptoms, aiming to mitigate its potential progression into chronic and debilitating conditions. Imagine a scenario where a seemingly minor backache is shrugged off as just a result of a strenuous day.
You might think it will go away on its own, or perhaps you believe it's not worth bothering a doctor about. However, pain, even in its mildest form, can set off a domino effect in your body.
- Physical Compensations: Your body is an intricate system of interconnected parts. When one part is in pain, other parts of your body might start compensating to reduce strain. For example, if you're favoring your left knee due to pain, you might unintentionally put more pressure on your right leg. This can lead to a whole new set of problems.
- Psychological Impact: Constant pain can take a toll on your mental well-being. It can lead to anxiety, depression, sleep disturbances, and decreased quality of life.
- Chronic Pain Development: Ignored pain often becomes a chronic issue. What started as a minor discomfort can turn into a long-term condition that's much harder to treat.
Treating patients as soon as possible following an injury is known as early intervention therapy. Physical and occupational therapists work in tandem with patients to help them restore mobility and reduce discomfort. This can be accomplished using a variety of techniques, including stretches, exercises, and manual therapy.
The Importance of Early Intervention
An essential part of the palliative framework for pain management is played by interventional pain management. Physically, delayed intervention may worsen the severity of underlying conditions, impeding the natural healing process and contributing to prolonged recovery times.
Beyond the physical realm, the psychological toll of uncontrolled pain is substantial, often leading to increased stress, anxiety, and depression. The interplay between physical and mental health underscores the necessity of early intervention to break this cycle and mitigate the far-reaching consequences of pain that extend well beyond the immediate discomfort.
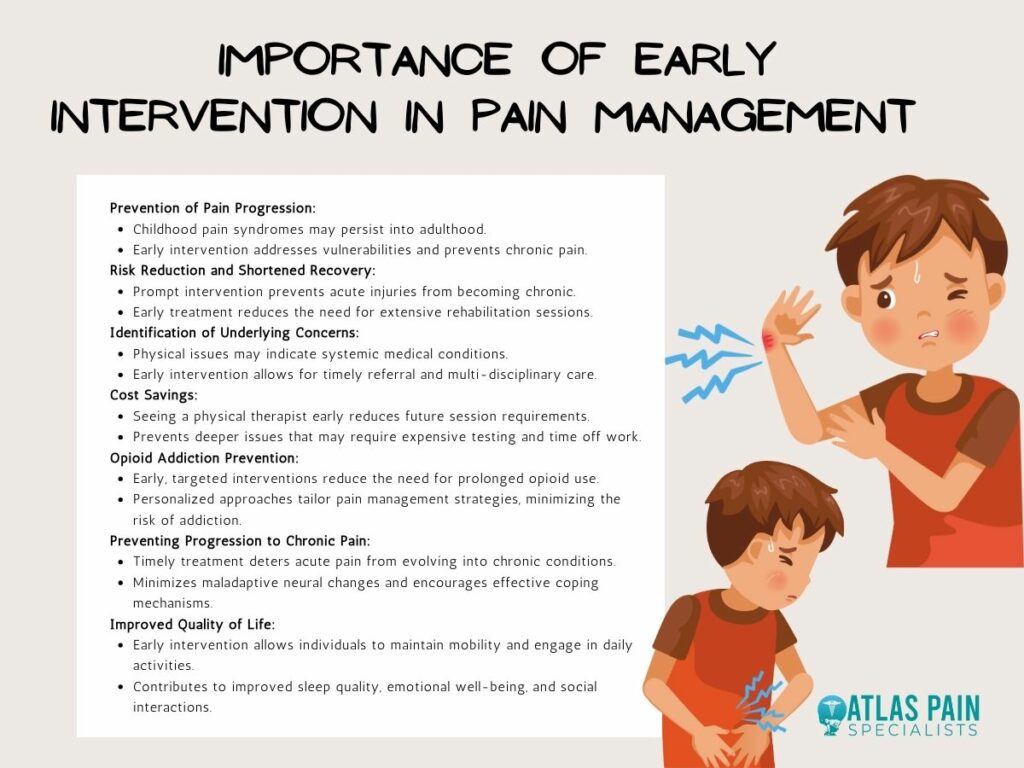
1. Prevents The Progression Of Pain
Childhood pain syndromes frequently persist throughout adulthood. A variety of vulnerabilities that may have preceded the start of childhood pain or that may co-occur as a result of childhood pain are linked to chronic pain in childhood.
These susceptibility factors have been demonstrated to prolong pain and disability in childhood, but they may also be involved in long-term health and developmental deficits that impact adulthood. When it comes to managing childhood trauma and vulnerabilities linked to an increased likelihood of maladaptive adult consequences, psychological interventions can be quite helpful.
Chronic pain, if not tackled early, can result in a cycle of decreased mobility, muscle atrophy, and heightened sensitivity, further complicating treatment. Pain can also be prevented in adulthood through:
- Mitigating Central Sensitization: Timely intervention plays a crucial role in mitigating central sensitization, a phenomenon where the nervous system becomes hypersensitive to stimuli, which can contribute to heightened pain perception.
- Targeting Underlying Causes: Early identification and intervention enable healthcare professionals to target and address the root causes of pain. This proactive approach aims to eliminate or manage the factors triggering pain, preventing its transformation from an acute condition to a persistent, chronic state.
- Promoting Neural Plasticity: Early pain management supports positive neural plasticity, the brain's ability to adapt and reorganize.
- Preserving Functional Abilities: Swift intervention aids in preserving or restoring functional abilities by implementing strategies to minimize the impact of discomfort on an individual's physical capabilities, supporting a quicker return to normal daily activities.
Early intervention serves as a pivotal interruption in the cascade of pain signaling. Addressing pain promptly disrupts the series of physiological and neurological events that can lead to an exacerbation of discomfort.
2. Reduces Risks And Shortens Recovery Time
If pain were persistent and intense, most would see a doctor right away. But if it's occasional – there is an urge to put it off.
The “I'm sure it will get better on its own” mentality. Sound familiar? You do yourself a disservice in waiting because doing so significantly increases the odds that you will aggravate your injury.
If you do, it could make a mountain of what should have been a molehill. Early intervention's goal is to address tissue fatigue and injury before it becomes a more serious issue.
Making a clear game plan on the best way to reduce pain and foster healing, preventing a possibly more costly accident or issue later down the road. This is how acute injuries become chronic ones. Early intervention can prevent that from happening.
When you wait to see a PT and subsequently aggravate an injury, you effectively add to the number of services required (ie: manual/massage therapy, dry needling, blood flow restriction, electrical stimulation, etc.) to correct your worsened ailment. Because injuries that have been festering tend to become very irritable and sensitive, therapy must start by calming the injury down before the real rehab can begin.
This increases the number of sessions required for recovery and logically increases the length of recovery time. An injury that could have taken 1-2 months of PT (if addressed early) can quickly expand to 6 months of recovery time or more. Take action today to mitigate the risk of lengthened recovery time.
3. Can Identify Other Underlying Concerns, Early
Not every physical pain, discomfort, or mobility issue is connected to a strain, fracture, or tear. There are times when these are symptoms of an underlying systemic medical condition that need to be addressed by a physician. A PT can identify this and refer you to the appropriate professional before the issue escalates.
And if your issue is connected to a medical condition, the PT will be there to assist in a multi-disciplinary plan prescribed by your doctor. Not all injuries may manifest symptoms immediately following an accident.
Some conditions, such as whiplash or back injuries, may have a delayed onset of symptoms. Seeking early intervention allows for a thorough examination to identify any hidden injuries that may have gone unnoticed.
4. It Can Actually Save You Money
You may hesitate to see a PT due to concerns over expense. Even if you're covered by insurance, you may not want to “use up” your covered visits. Whatever the case may be, you're not doing your bank account or insurance policy allowance any favors by waiting.
By seeing a PT early, before you aggravate an existing injury, extend recovery time, and/or leave an ailment unchecked, you generally reduce your number of session requirements in the future. Not to mention, deeper issues may also require testing, which ain't cheap! And don't forget about the time away from work or fun!
5. Prevents Opioid Addiction Or Dependency
More than half of those who abuse opioids on a regular basis got their prescriptions from doctors, according to a recent study. The fact that over 90% of people who survived prescription drug overdoses were able to obtain another prescription for the same medication that caused the overdose raises even more concerns!
Moreover, most of those patients got a new prescription from the physician who referred them. These startling figures can be partially attributed to the fact that patients are more prone to develop an addiction to opioid medications the longer they take them.
Early, targeted interventions may reduce the need for prolonged medication use, thereby promoting a more sustainable and balanced pain management strategy. It allows healthcare providers to tailor and optimize pain control strategies based on the specific needs and responses of the individual.
This personalized approach ensures that the chosen interventions align with the patient's unique pain profile, leading to more effective and sustainable relief.
7. Preventing Progression
Early intervention acts as a crucial deterrent to the progression of acute pain into a persistent, chronic state. Many acute pain issues, if left untreated, can progress into chronic conditions, which can be much more challenging to manage and may require more aggressive treatments.
For instance, back pain caused by a herniated disc, if treated promptly, can often be managed with conservative methods like physical therapy and pain medications. However, if left unaddressed, it can lead to nerve damage and long-term pain that may require surgery.
Early intervention supports the minimization of maladaptive changes in neural pathways associated with persistent pain, reducing the likelihood of the development of neural patterns that contribute to chronic pain. It also allows individuals to develop and implement effective coping mechanisms for managing pain in ways that discourage the development of chronic pain-related conditions.
Preventing chronic pain through early intervention can also lead to a decrease in the long-term healthcare utilization associated with chronic pain management. This includes a reduction in the need for frequent medical visits, extensive diagnostic procedures, and prolonged use of medications or surgical interventions.
8. Improved Quality of Life
When you take the initiative to seek help for your pain, you're investing in your well-being. You can continue to enjoy your daily activities, maintain your mobility, and participate in the things you love without pain holding you back.
Early intervention in pain management contributes to improved sleep quality and facilitates restorative rest, reducing disruptions caused by pain-related discomfort and promoting overall well-being. This way, it also positively influences emotional well-being.
Chronic pain often takes a toll on mental health, leading to conditions such as anxiety and depression, and by addressing pain early, individuals can better cope with the emotional challenges associated with persistent pain.
Proactive pain management also preserves or restores physical functionality, allowing individuals to maintain their ability to engage in daily activities. These activities allow for improved social interactions since chronic pain can lead to social isolation due to the limitations it imposes on an individual's ability to participate in social activities.
Why Is Early Intervention Therapy A Better Solution?
Several studies have demonstrated that an individual's ability to resume work sooner is correlated with the timing of their rehabilitation. In order to ensure a pain-free future, pain management goes beyond only treating pain in the present.
It gives medical professionals a chance to inform patients about their disease and available treatments. This knowledge fosters a sense of accountability that leads to improved rehabilitation outcomes.
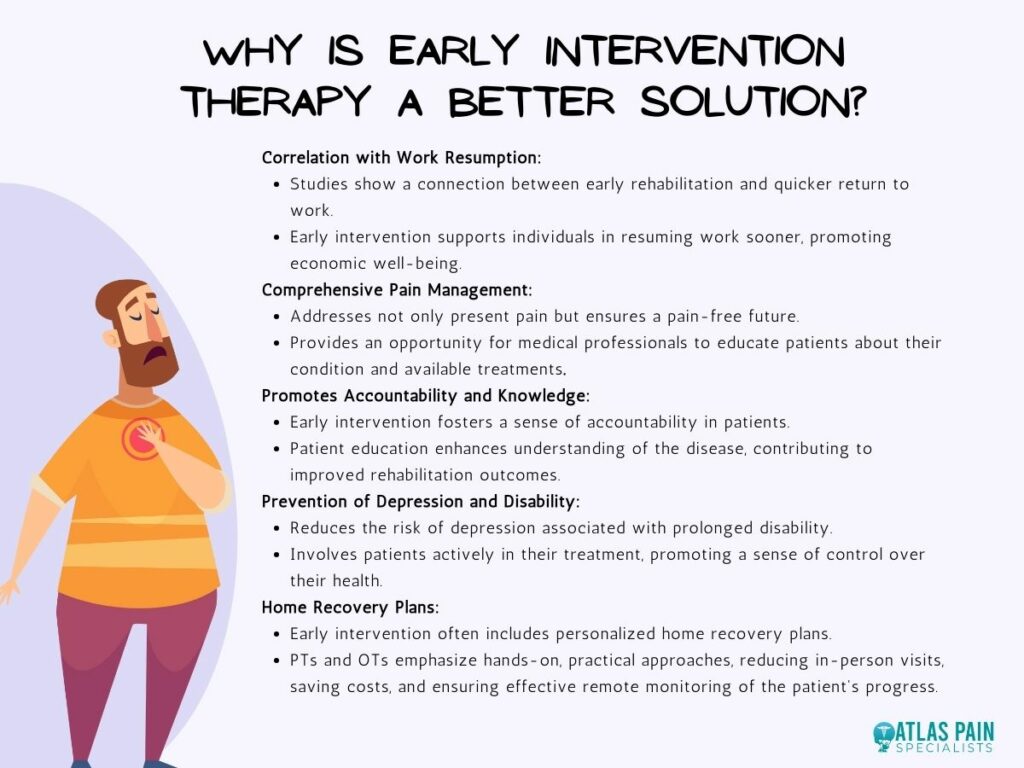
Keep in mind that getting help early on is essential for living a pain-free, healthy life. In addition to lowering the risk of depression that is frequently connected to becoming disabled, functional recovery involves patients in their treatment.
Early intervention treatment also has the advantage of frequently providing workers with home recovery plans. The hands-on, practical approach that PTs and OTs emphasize trains patients to complete rehabilitation tasks at home with routine "check-ins" with the PT or OT. This creative method reduces in-person visits, saves money, and keeps track of the patient's recovery path.
Acute vs. Chronic Pain: What Are The Differences?
It is evident that proactive strategies not only prevent the escalation of pain but also pave the way for improved overall well-being. From recognizing the diverse manifestations of pain to strategizing early interventions, the imperative is clear—timely action yields positive outcomes.
However, understanding pain is only part of the equation since acute and chronic pain is a fundamental distinction. This understanding sets the stage for our next exploration—"Acute vs. Chronic Pain," which influences not only immediate relief but also long-term well-being.
About Dr. Sean Ormond



