Recognizing the Final Stages of Spinal Stenosis and Available Care Options
Living with spinal stenosis can drastically change your daily life. What may have started as occasional discomfort can turn into constant pain, stiffness, and difficulty moving around.
Simple activities can feel like a struggle as days go by, which leaves you wondering about its progression and how to manage it.For some, it progresses slowly, while for others, symptoms can worsen rapidly.
If you know what to look for in your symptoms you can find ways to manage them and find relief.
What is Spinal Stenosis?
Living with spinal stenosis means your spine is changing in a way that affects your mobility, comfort, and overall health. It doesn't narrow down to back pain but also how your spine interacts with the nerves that control movement and sensation in your body.
The spine is your body’s central support system, built to protect the spinal cord while allowing you to move freely. As the spaces within your spine narrow, the pressure on these nerves increases, leading to pain, weakness, and sometimes even a loss of control over basic functions.
When something interferes with this balance, such as spinal stenosis, even simple activities can become difficult.
What Happens to the Spine When Stenosis Develops?
Your spine is made up of vertebrae, discs, and nerves that work together to keep you upright and moving. The spinal canal is a hollow passage running through these bones, housing the spinal cord and the nerves that branch out to the rest of your body.
This space needs to be wide enough for the nerves to function properly. With spinal stenosis, this space becomes too narrow.
It can happen when the discs between your vertebrae wear down, when ligaments thicken, or when bone spurs form. As a result, nerves get squeezed, and that pressure causes pain, numbness, or weakness, usually in the lower back, legs, neck, or arms.
What Causes Spinal Stenosis to Worsen Over Time?
Patients with spinal stenosis don’t always have linear or static symptoms. It can start as mild pain or occasional stiffness and turn into persistent pain, weakness, or difficulty moving.
Spinal stenosis is a progressive condition, which means it tends to get worse as time goes on, especially if the underlying causes are not addressed. While some people experience slow changes over decades, others notice a faster decline.
The rate at which your condition worsens depends on several factors.
1. Aging and Wear and Tear
As you get older, the structures in your spine naturally start to break down. The discs that cushion your vertebrae lose moisture and become thinner, reducing their ability to absorb shock.
This can cause the bones in your spine to shift closer together, narrowing the space where your nerves pass through. At the same time, the ligaments that support your spine may thicken and harden.
When this happens, they can encroach on the spinal canal, adding to the pressure on your nerves. Arthritis is also common with aging and can lead to bone spurs that take up even more space in an already narrowed spinal canal.
2. Injuries and Arthritis
If you have ever injured your back or neck, you may be at greater risk for worsening spinal stenosis. Injuries like fractures, herniated discs, or dislocations can lead to inflammation, scarring, and structural changes that contribute to the narrowing of the spinal canal.
Even if an injury heals, the damage can accelerate the degenerative process, making symptoms more noticeable earlier than expected. Osteoarthritis, the most common type, wears down the cartilage between joints, leading to inflammation and bone spur growth.
These spurs can push into nerve pathways, increasing pain and limiting movement. Rheumatoid arthritis, an autoimmune condition, can also cause swelling in the joints and ligaments, worsening nerve compression over time.
3. Genetic and Lifestyle Factors
Some people are born with a naturally narrow spinal canal, which means even small changes can lead to symptoms sooner. If spinal stenosis runs in your family, you may need to be extra cautious about managing your spinal health.
Lifestyle choices can also influence how quickly the condition worsens. Carrying excess weight puts more strain on your spine, increasing pressure on already compressed nerves.
Poor posture, especially when sitting for long periods, can add unnecessary stress to the spine and speed up degeneration. A sedentary lifestyle weakens the muscles that support your back, making it harder for your body to compensate for spinal changes.
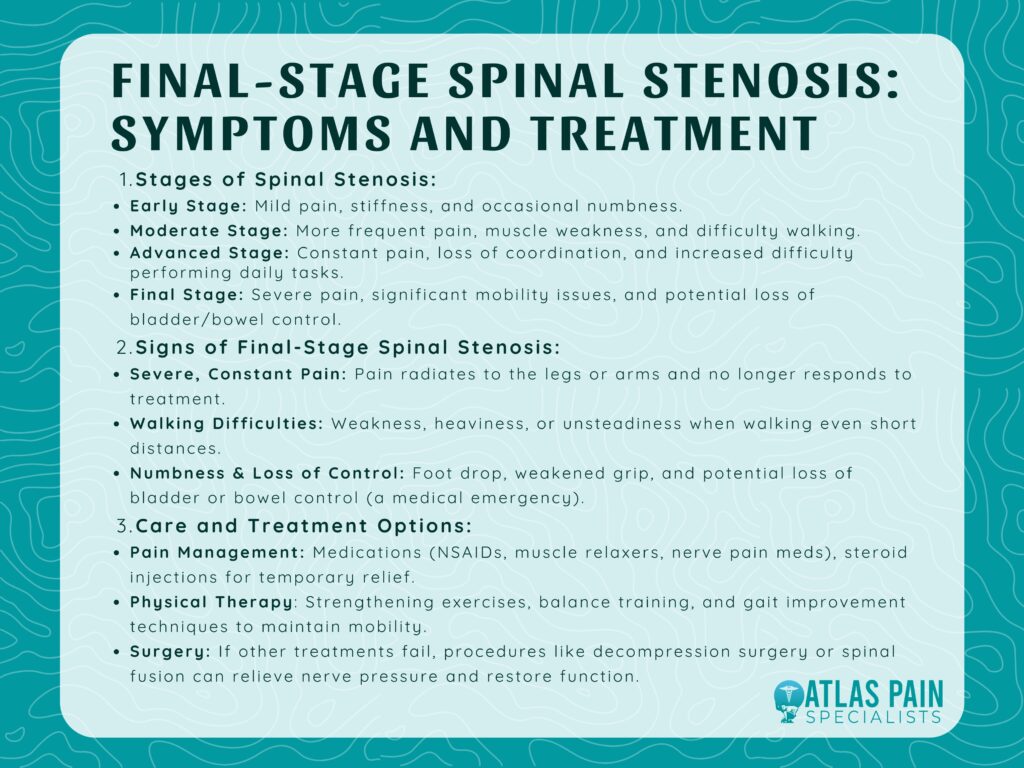
The Different Stages of Spinal Stenosis
Spinal stenosis develops gradually, often starting with minor pain that may not seem like a big deal. As time goes on, the symptoms can become more noticeable, affecting how you move, stand, or even sleep.
| Stage | Symptoms | Impact on Daily Life |
|---|---|---|
| Early Stage | Mild pain, occasional stiffness, minor numbness | Discomfort after long periods of standing or walking |
| Moderate Stage | More frequent pain, radiating discomfort, muscle weakness | Difficulty walking long distances, need to lean forward for relief |
| Advanced Stage | Constant pain, leg or arm weakness, loss of coordination | Trouble performing daily tasks, frequent need for rest |
| Final Stage | Severe pain, significant mobility issues, possible loss of bowel/bladder control | High risk of falls, loss of independence, requires medical intervention |
Not everyone experiences spinal stenosis in the same way. Some people may go years with only mild symptoms, while others may find that their condition worsens quickly.
1. Early Signs
In the beginning, spinal stenosis may not cause constant pain. You might feel occasional stiffness or discomfort in your lower back or neck, especially after standing or walking for long periods.
Some people notice mild numbness or tingling in their legs or arms, but these symptoms tend to go away with rest. At this stage, the narrowing of the spinal canal is minor, and nerves are not under significant pressure.
Because the symptoms are not severe, many people assume they are just dealing with normal aging or overuse. This is the best time to start making lifestyle changes, such as improving posture, strengthening core muscles, and maintaining a healthy weight.
2. Symptom Progression
As spinal stenosis moves into the moderate stage, symptoms become harder to ignore. Pain may become more frequent, radiating down the legs or arms.
You might feel weakness, heaviness, or a burning sensation in your lower back, making it harder to stand or walk for long periods. Some people experience "shopping cart syndrome," where leaning forward provides relief by opening up the spinal canal slightly.
At this stage, nerves are under more pressure, and symptoms may no longer disappear with rest. Everyday tasks like climbing stairs, bending over, or even getting dressed can become challenging.
How to Recognize the Final Stage of Spinal Stenosis
Spinal stenosis may start off as a mild annoyance, but as it progresses, the impact on your daily life can become impossible to ignore. What was once occasional pain can turn into constant pain, and activities that used to be easy may feel exhausting or even impossible.
If you are wondering whether you have reached the final stage of spinal stenosis, there are clear signs that indicate your condition has advanced to a critical point.
1. Extreme Consistent Pain
Pain is one of the most noticeable symptoms of spinal stenosis, but in earlier stages, it may only flare up occasionally. By the time you reach the final stage, pain tends to be constant and can become unbearable.
It may radiate from your lower back down your legs or from your neck into your arms. Some people describe it as a deep, burning, or electric shock-like sensation that does not go away even when resting.
Unlike before, pain relief methods that once worked may no longer be effective. This is a sign that nerve compression has worsened, and without treatment, it may lead to permanent nerve damage.
2. Difficulty Walking Short Distances
Walking can become a major challenge in the final stage of spinal stenosis. You may feel unsteady, weak, or as if your legs are going to give out.
Some people experience a sensation of heaviness in their legs, making it feel like they are dragging their feet with every step. If you find that you need to stop and rest frequently while walking short distances your condition may have reached an advanced stage.
This happens because the nerves controlling your leg muscles are under too much pressure. Over time, these nerves may stop functioning properly, leading to a loss of coordination and muscle strength.
3. Numbness, Weakness, and Loss of Bladder or Bowel Control
Numbness and weakness in the legs or arms are common symptoms of spinal stenosis, but in the final stage, these sensations can become more severe and widespread. You may struggle to lift your foot properly while walking, a condition known as foot drop.
Your grip may weaken, making it harder to hold onto objects or complete everyday tasks like buttoning a shirt. One of the most serious signs of advanced spinal stenosis is the loss of bladder or bowel control.
If you experience sudden incontinence, difficulty urinating, or loss of sensation in your groin area, this could indicate cauda equina syndrome. This is a medical emergency that requires immediate attention and without quick treatment, permanent nerve damage may occur.
Finding the Best Care and Treatment Options
When spinal stenosis reaches its final stage, finding the right care becomes a priority. At this point, the condition affects your ability to move, complete daily tasks, and live comfortably.
The good news is that there are options available, ranging from non-invasive treatments to surgical procedures that can provide long-term relief. Some people can manage their symptoms with a combination of pain management and physical therapy, while others may need surgery to regain mobility.
1. Pain Management Methods
For many people, the first step in treatment is pain relief. If over-the-counter medications like ibuprofen or acetaminophen no longer work, your doctor may suggest stronger ones.
Muscle relaxers, nerve pain medications, or anti-inflammatory drugs can help reduce discomfort and improve function. Steroid injections are another option for pain management.
These injections deliver a powerful anti-inflammatory medication directly into the affected area, reducing swelling around the nerves and providing temporary relief. They don't directly fix the underlying issue, but they can make it easier to move and participate in physical therapy.
2. Physical Therapy
Even in the advanced stages of spinal stenosis, physical therapy can be beneficial. A trained therapist can help strengthen the muscles that support your spine and improve flexibility.
Therapists also work on balance and coordination exercises, which can help reduce the risk of falls. Many people who experience leg weakness or numbness benefit from gait training, which focuses on improving the way they walk to maintain as much mobility as possible.
This helps you learn how to move with less strain on your back and legs.
3. Surgery
If non-surgical treatments are no longer providing relief, your doctor may recommend surgery. The goal of surgery is to relieve pressure on the spinal nerves, which can help reduce pain, numbness, and weakness.
| Procedure | Description | Best For | Recovery Time |
|---|---|---|---|
| Laminectomy | Removal of part of the vertebra (lamina) to relieve pressure on nerves | Severe nerve compression, loss of mobility | 4 – 6 weeks |
| Spinal Fusion | Fuses two or more vertebrae together for stability | Cases with spinal instability | 3 – 6 months |
| Minimally Invasive Surgery | Small incisions, less tissue disruption | Milder cases or those unable to undergo major surgery | 2 – 4 weeks |
There are different types of procedures available, and the right one for you will depend on the severity of your condition and your overall health.
- Laminectomy – This is one of the most common procedures for spinal stenosis. It involves removing part of the vertebrae (the lamina) to create more space in the spinal canal. This can relieve pressure on the nerves and improve symptoms.
- Spinal Fusion – In some cases, spinal fusion is performed along with a laminectomy. This procedure connects two or more vertebrae to stabilize the spine and prevent further narrowing.
- Minimally Invasive Surgery – Some patients may qualify for a less invasive approach that involves smaller incisions and a shorter recovery time. These procedures use specialized instruments to remove bone or tissue compressing the nerves without disrupting surrounding muscles.
Surgery is usually considered when symptoms are severe and significantly impact the quality of life.
Does Cracking Your Back Cause Arthritis
Living with spinal stenosis involves managing pain and staying as active and independent as possible. When your spine starts limiting what you can do, it can be overwhelming but knowing your treatment options puts you in control.
You may have also heard concerns about whether cracking your back could lead to arthritis. While there is no clear link between cracking your joints and developing arthritis, long-term spinal stress can contribute to issues that worsen spinal stenosis.
Frequent or forceful cracking, especially if done incorrectly, can put strain on the ligaments and joints in your spine, which may accelerate wear and tear over time. Since spinal stenosis is often caused by degeneration, it is important to protect your spine as much as possible.
About Dr. Sean Ormond



