Comprehensive Guide to Deep Vein Thrombosis (DVT)
A blood clot in a deep vein, usually in the legs, can cause a medical disorder called deep vein thrombosis (DVT). Though DVT can affect any deep vein, the legs are most commonly involved, leading to not only local discomfort but also the potential for serious complications.
The implications of an untreated DVT extend beyond immediate health concerns, as clots can dislodge and travel to the lungs, causing a life-threatening pulmonary embolism. The pathophysiology of DVT is complex, influenced by factors neatly categorized by Virchow's Triad with elements that contribute to its risk and development. Let as now delve into a comprehensive guide to deep vein thrombosis.
What is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis (DVT) is a condition characterized by the formation of a blood clot, or thrombus, within a deep vein in the body. Although DVT can occur in any deep vein, it most commonly affects those in the legs, including the calves, thighs, or pelvis.
The concern with DVT extends beyond the local symptoms it may cause, such as pain, swelling, and redness. The development of DVT is influenced by several factors, including lifestyle risks such as smoking, genetic risks such as inherited clotting disorders (Factor V Leiden), and health-related risks such as certain cancers and their treatments.
The Pathophysiology of DVT
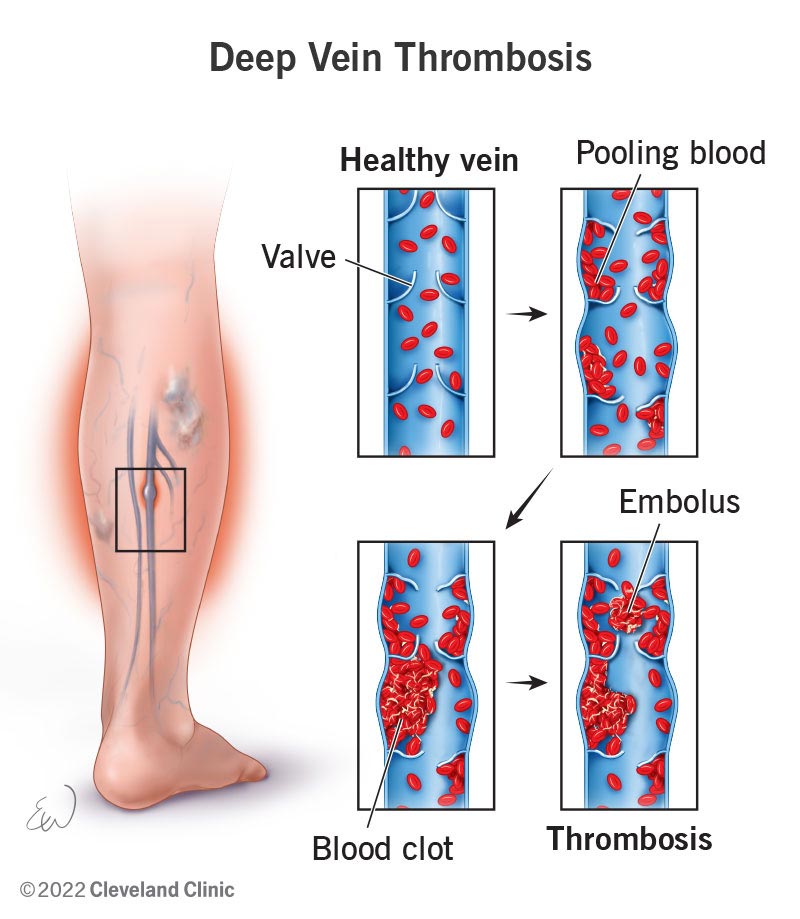
Central to the pathophysiology of DVT is the Virchow's Triad. It outlines the three primary conditions that predispose individuals to thrombosis: venous stasis, vascular injury, and hypercoagulability.
Additionally, whether the DVT is actute or chronic has an impact on the condition's full spectrum, from initial onset to potential long-term management.
- Venous Stasis
Venous stasis occurs when the normal flow of blood through the veins is slowed or interrupted, a common predisposing factor for DVT. This condition is particularly prevalent in individuals who are immobilized for long periods, such as those undergoing prolonged bed rest, travelers on long flights, or patients with paralysis.
Venous stasis leads to an accumulation of blood in the lower limbs, increasing the contact time between blood components and the vein walls. This prolonged contact time facilitates the aggregation of clotting factors and the formation of thrombi.
- Vascular Injury
Vascular injury to the inner lining of the vein (endothelium) is another critical component of Virchow's Triad. Such injuries can result from surgical procedures, traumatic events, or the insertion of intravenous catheters.
The damage to the endothelium triggers the body's natural coagulation cascade as a repair mechanism. However, this process can become pathological if the coagulation is excessive, leading to thrombus formation within the vein.
- Hypercoagulability
Hypercoagulability refers to an increased tendency of the blood to clot, which can be inherited or acquired. Conditions such as Factor V Leiden or prothrombin gene mutation, antiphospholipid syndrome, and certain cancers can inherently increase clotting risk.
Acquired hypercoagulability may result from hormone therapy, pregnancy, or cancer. This heightened state of coagulability significantly elevates the risk of forming thrombi.
Types of DVT and Severity Scale
Deep Vein Thrombosis (DVT) can be classified based on the location of the clot within the venous system. This classification into proximal and distal DVT is critical for assessing the risk of complications, guiding treatment decisions, and understanding the potential outcomes associated with each type.
The severity scale of DVT hinges on this classification, influencing both immediate management strategies and long-term care.
1. Proximal DVT
Proximal DVT refers to clots that occur in the deep veins located above the knee, including the popliteal, femoral, and iliofemoral veins. These veins are responsible for carrying a significant portion of the blood back to the heart from the lower limbs.
Due to their larger diameter and the higher volume of blood they handle, clots in these veins pose a greater risk for serious complications, such as pulmonary embolism.
2. Distal DVT
Distal DVT, also known as calf vein thrombosis, involves clots in the deep veins below the knee, such as the peroneal, tibial, and gastrocnemius veins. While these clots are generally considered less dangerous than proximal DVTs, they are not without risk.
There is a potential for distal DVTs to extend into the proximal veins, thereby increasing the risk of pulmonary embolism.
3. Acute vs. Chronic DVT
Acute DVT refers to the initial phase of thrombus formation and is characterized by sudden symptoms such as swelling, pain, and redness in the affected limb. The immediate implications of acute DVT include the risk of the clot growing or dislodging and causing a pulmonary embolism. Prompt diagnosis and treatment are essential to mitigate these risks.
Chronic DVT refers to the long-term consequences that can arise after an initial DVT episode, including the possibility of post-thrombotic syndrome (PTS). PTS can result in chronic pain, swelling, and discoloration of the affected limb, and, in severe cases, venous ulcers.
Symptoms of Deep Vein Thrombosis (DVT)
It's important to note that DVT can occur without any noticeable symptoms. Therefore, being aware of the risk factors and preventive measures is crucial, especially for individuals with a high risk of developing blood clots.
DVT symptoms can vary from subtle to pronounced, and in some cases, the condition may be asymptomatic. However, when symptoms do occur, they typically manifest in the affected limb and may include the following:
Common Symptoms
- Swelling: One of the most noticeable signs of DVT is swelling in the leg, ankle, or foot on one side. It can come on gradually or suddenly, depending on the size and location of the clot.
- Pain: DVT can produce pain that feels like cramps or soreness and frequently begins in the calf. When walking or standing, the pain could get greater.
- Warmth: The skin around the painful area may feel warmer to the touch compared to surrounding areas.
- Red or Discolored Skin: The affected leg may show redness or a noticeable discoloration, which is a sign of inflammation and reduced blood flow.
- Enlarged Veins: Veins near the skin's surface may become more visible or feel firm or enlarged.
Signs That Require Immediate Medical Attention
- Severe Swelling and Pain: Sudden and severe swelling and pain in the leg, especially if accompanied by the symptoms listed above, necessitate prompt medical evaluation to rule out DVT.
- Difficulty Breathing: Pulmonary embolism is a condition marked by abrupt dyspnea, fast heartbeat, disorientation, and chest pain that may get worse with deep breathing if a clot breaks free and goes to the lungs. This is a medical emergency that has to be treated right away.
- Coughing Blood: Coughing up blood is a severe symptom that can indicate a pulmonary embolism, and urgent medical care is essential.
Diagnosis of Deep Vein Thrombosis (DVT)
Diagnosing Deep Vein Thrombosis (DVT) involves a combination of clinical assessment, imaging studies, and laboratory tests. Accurate diagnosis allows for timely and appropriate treatment to prevent the progression of the clot and reduce the risk of complications.
Here’s an overview of the diagnostic process for DVT:
1. Clinical Assessment
- Patient History: The initial step involves a thorough review of the patient's medical history, including any previous episodes of DVT, family history of blood clots, and potential risk factors such as recent surgeries, immobility, or underlying health conditions.
- Physical Examination: A physical examination is conducted to check for signs of DVT, such as swelling, warmth, redness, and tenderness along the vein's path. However, these symptoms can be similar to other conditions, making further diagnostic testing necessary for confirmation.
2. Imaging Studies
- Ultrasound: The most common imaging test for diagnosing DVT, an ultrasound uses sound waves to create images of blood flow in the veins. A Doppler ultrasound can specifically detect irregularities in the flow of blood, indicative of a clot.
- Venography: Although less commonly used today due to the invasiveness of the procedure, venography can be employed in complex cases. A contrast dye is injected into a large vein in the foot or ankle, and X-rays are taken to visualize the veins in the legs
3. Laboratory Tests
- D-dimer Test: A D-dimer test measures a substance that is released when a blood clot breaks down. High levels of D-dimer in the blood can indicate the presence of an active clotting process. However, elevated D-dimer levels can be caused by various factors other than DVT, making the test non-specific. Therefore, a positive D-dimer test is usually followed by imaging studies for confirmation of DVT.
Other Diagnostic Tests
In some cases, when ultrasound results are inconclusive and the patient's clinical probability of DVT is high, additional imaging tests may be required. These could include:
- MRI (Magnetic Resonance Imaging): MRI can provide detailed images of the veins and may be used in cases where ultrasound is inconclusive, particularly for pelvic or abdominal veins.
- CT Venography: For detecting clots in the pelvis and abdomen, CT venography can be an option, involving the injection of contrast material and CT imaging.
Treatment Options for Deep Vein Thrombosis (DVT)
The treatment of Deep Vein Thrombosis (DVT) is aimed at preventing the clot from growing and reducing the risk of complications, such as a pulmonary embolism. Treatment strategies can vary based on the location of the clot, the patient's overall health, and the presence of any underlying conditions.
Here are the primary treatment options for DVT:
1. Anticoagulants (Blood Thinners)
Anticoagulants, commonly called blood thinners, decrease the blood's ability to clot. They don't break up existing clots but can prevent clots from getting bigger and reduce the risk of additional clots forming.
Anticoagulants include warfarin (Coumadin) and direct oral anticoagulants (DOACs) such as rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa). The choice of medication depends on the individual's specific situation, with DOACs offering the advantage of not requiring regular blood monitoring.
2. Thrombolytics (Clot Busters)
In severe cases of DVT, especially when there is a significant threat to limb viability, thrombolytics may be used. These drugs can dissolve blood clots quickly but are associated with a higher risk of bleeding than anticoagulants.
Thrombolytic therapy is typically reserved for life-threatening situations, such as a severe pulmonary embolism or phlegmasia cerulea dolens (a rare form of DVT that threatens limb loss).
3. Compression Stockings
Compression stockings are designed to prevent swelling and reduce the chance of complications of DVT. By applying pressure to the lower legs, they help maintain blood flow and decrease the risk of post-thrombotic syndrome.
They are often recommended for at least two years after a DVT diagnosis to manage symptoms and prevent long-term complications.
4. Inferior Vena Cava (IVC) Filters
An IVC filter can be an alternative for patients who are medically unable to take anticoagulants. Blood clots are prevented from reaching the lungs by placing this tiny device into the inferior vena cava, a major vein that returns blood from the lower body to the heart.
IVC filters are generally used as a temporary measure, and in some cases, they may be removed once the risk of pulmonary embolism decreases.
5. Lifestyle and Home Remedies
- Physical Activity: Staying active and moving around as soon as possible after surgery or during prolonged bed rest can help prevent clots from forming.
- Hydration: Drinking plenty of fluids can prevent dehydration, which is a risk factor for DVT.
6. Surgical and Other Procedures
- Catheter-directed thrombolysis: This minimally invasive procedure involves threading a catheter to the site of the clot and delivering thrombolytic drugs directly to dissolve it.
- Venous thrombectomy: In rare cases, surgery might be necessary to remove a large vein clot, particularly if it's causing significant symptoms and other treatments aren't effective.
The Role of Physical Therapy in Pain Management
Deep Vein Thrombosis (DVT) represents a significant health concern with potential for serious complications, emphasizing the importance of early detection, effective treatment, and diligent management. The process of learning about DVT fundamentals and working through treatment and prevention choices highlights how difficult it is to manage the condition.
Central to this journey is the integration of medical interventions, lifestyle modifications, and supportive therapies tailored to individual needs. For patients recovering from DVT, physical therapy offers a targeted approach to alleviate pain, improve circulation, and restore function in the affected limb.
Through personalized exercise programs, patients can safely engage in activities designed to enhance venous return, reduce swelling, and prevent the stiffness and discomfort often associated with DVT and its aftermath, such as post-thrombotic syndrome (PTS).
About Dr. Sean Ormond