
The Role of Inflammation in Chronic Pain Conditions
Chronic pain is a complex and pervasive health issue affecting millions worldwide, often debilitating individuals and hindering their quality of life. While acute pain serves as a vital warning signal indicating tissue damage or injury, chronic pain persists long after the initial injury has healed, becoming a condition in its own right.
Effective management and treatment of chronic pain depend on an understanding of its underlying causes. Inflammation is one important component linked to the persistence of chronic pain.
Inflammation, typically considered a protective response by the body to injury or infection, involves a cascade of biochemical processes aimed at removing harmful stimuli and initiating tissue repair. Let's look at the role of inflammation in chronic pain conditions.
What is Inflammation?
Inflammation is a fundamental biological response triggered by the body's immune system in response to injury, infection, or irritation. It is a complex process involving various cells, signaling molecules, and biochemical pathways, orchestrated to eliminate harmful stimuli and initiate tissue repair.
Definition and Basic Physiology
In essence, inflammation can be understood as the body's attempt to defend itself against harmful stimuli and promote healing. This process involves a series of coordinated events, starting with the recognition of the threat by the immune system, followed by the recruitment of immune cells to the site of injury or infection.
Key players in the inflammatory response include:
- White blood cells, such as neutrophils and macrophages
- Signaling molecules like cytokines and chemokines.
These cells and molecules work together to remove pathogens, clear damaged tissue debris, and initiate tissue repair processes.
From a physiological standpoint, inflammation is characterized by hallmark signs and symptoms, including redness, swelling, heat, pain, and loss of function, reflecting the underlying changes occurring at the site of inflammation.
Types of Inflammation: Acute vs. Chronic
Inflammation can be broadly classified into two main types: acute and chronic.
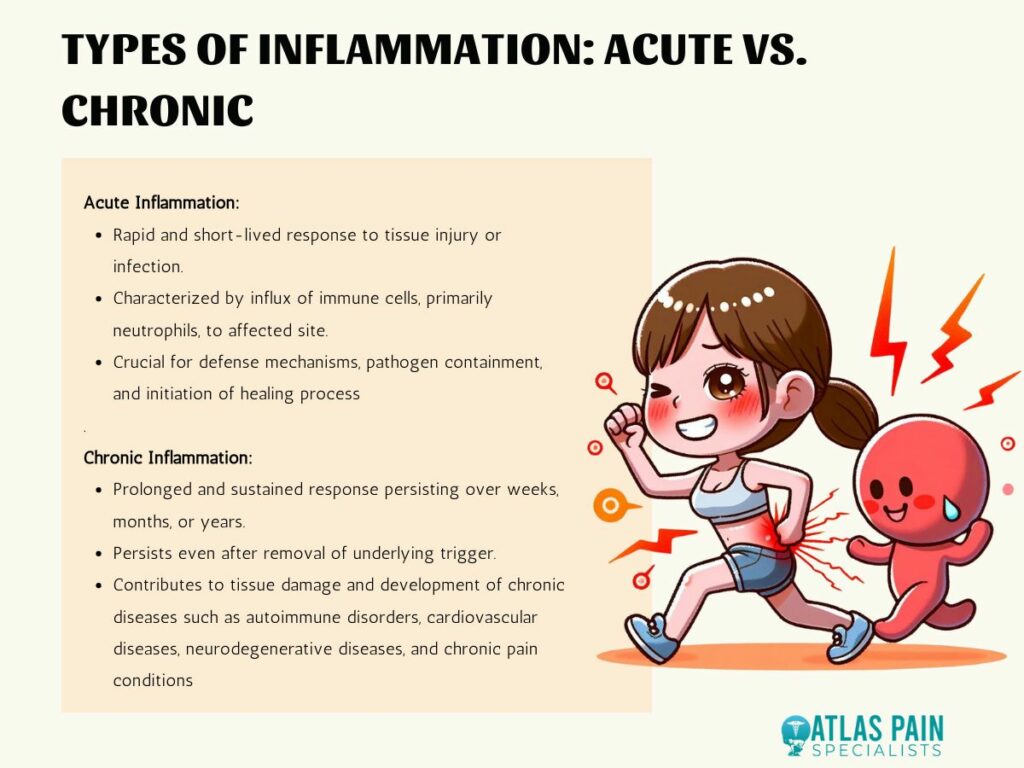
- Acute inflammation
Acute inflammation is a rapid and short-lived response that typically occurs in response to tissue injury or infection. It is characterized by the influx of immune cells, primarily neutrophils, to the affected site, leading to the classic signs of inflammation mentioned earlier.
Acute inflammation is a crucial part of the body's defense mechanisms and is essential for containing and eliminating pathogens, as well as initiating the healing process. In contrast,
- Chronic inflammation
Chronic inflammation is a prolonged and sustained response that persists over weeks, months, or even years. Unlike acute inflammation, which resolves once the underlying trigger is removed, chronic inflammation can persist even in the absence of an apparent threat.
This chronic activation of the immune system can lead to tissue damage and contribute to the development of various chronic diseases, including autoimmune disorders, cardiovascular diseases, neurodegenerative diseases, and chronic pain conditions.
Causes of Inflammation
Inflammation can be triggered by a variety of factors, including infections, tissue injuries, autoimmune reactions, exposure to irritants or allergens, and metabolic dysregulation.
- Infections, caused by bacteria, viruses, fungi, or parasites, can trigger inflammation by activating the immune system's innate and adaptive responses to eliminate the invading pathogens.
- Tissue injuries, such as cuts, burns, or trauma, can lead to inflammation as the body responds to repair the damaged tissue and prevent further harm.
- Autoimmune reactions occur when the immune system mistakenly attacks the body's own tissues, leading to chronic inflammation and tissue damage.
- Exposure to irritants or allergens, such as pollutants, chemicals, or certain foods, can trigger inflammatory responses in susceptible individuals, leading to conditions like asthma, allergic rhinitis, or contact dermatitis.
- Metabolic dysregulation, such as obesity, insulin resistance, or dyslipidemia, can promote chronic low-grade inflammation, contributing to the development of metabolic disorders and cardiovascular diseases.
The Relationship Between Inflammation and Chronic Pain
The connection between inflammation and chronic pain is multifaceted, involving intricate interactions between immune cells, inflammatory mediators, and sensory nerves. While inflammation is a natural response aimed at protecting the body from harm, chronic inflammation can contribute to the development and persistence of chronic pain conditions through various mechanisms.
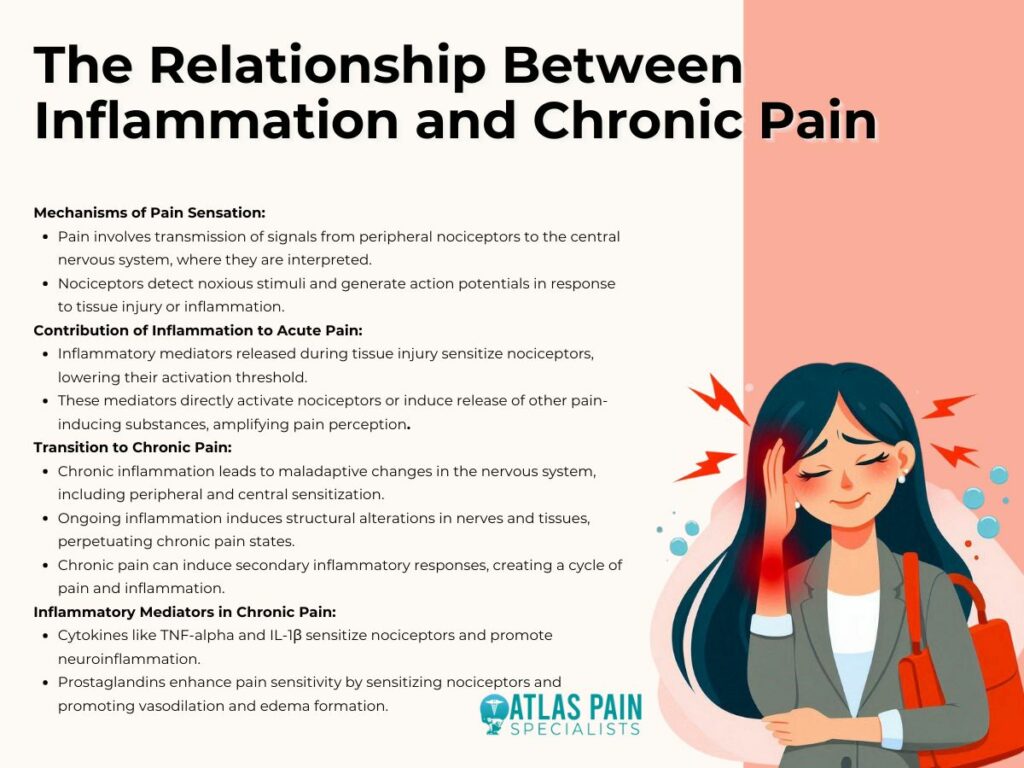
Mechanisms of Pain Sensation in the Body
Pain sensation is a complex physiological process involving the transmission of signals from peripheral nociceptors (pain receptors) to the central nervous system (CNS), where they are processed and interpreted as pain. Nociceptors are specialized sensory neurons located throughout the body, capable of detecting noxious stimuli, such as tissue injury, temperature extremes, or chemical irritants.
When activated, nociceptors generate action potentials that travel along nerve fibers to the spinal cord and brain, where they are integrated and perceived as pain. In addition to nociceptive pain, which arises from tissue damage or inflammation, other types of pain, such as neuropathic pain (caused by nerve damage or dysfunction) and inflammatory pain (caused by inflammation), contribute to the overall experience of chronic pain.
How Inflammation Contributes to Acute Pain
In acute pain conditions, such as tissue injury or inflammation, the inflammatory response plays a crucial role in sensitizing nociceptors and amplifying pain signals.
- Injured tissues release various inflammatory mediators, including prostaglandins, cytokines, and bradykinin, which sensitize nociceptors and lower their activation threshold, making them more responsive to stimuli.
- Inflammatory mediators can also directly activate nociceptors or induce the release of other pain-inducing substances, further enhancing pain perception.
This heightened sensitivity of nociceptors contributes to the characteristic symptoms of acute pain, including localized pain, tenderness, swelling, and redness, serving as a protective mechanism to prevent further injury and promote healing.
Transition from Acute to Chronic Pain
While acute pain serves a protective function and typically resolves once the underlying cause is addressed, chronic pain can develop when the inflammatory response becomes dysregulated or persists beyond the normal healing process.
- Chronic inflammation can lead to maladaptive changes in the nervous system, including peripheral sensitization (increased responsiveness of nociceptors) and central sensitization (heightened excitability of spinal cord neurons), resulting in persistent pain amplification and hypersensitivity.
- Ongoing inflammation can also induce structural alterations in nerves and tissues, leading to neuronal damage, synaptic remodeling, and neuroinflammation, which further perpetuate chronic pain states.
- Chronic pain itself can induce secondary inflammatory responses, creating a vicious cycle of pain and inflammation that contributes to the maintenance of chronic pain conditions.
Inflammatory Mediators Involved in Chronic Pain Conditions
Various inflammatory mediators have been implicated in the pathophysiology of chronic pain conditions, including cytokines, chemokines, prostaglandins, and neurotrophic factors. These molecules are released during the inflammatory response and can modulate neuronal excitability, synaptic transmission, and neuroinflammatory processes, contributing to the development and maintenance of chronic pain states.
For example,
- Cytokines such as tumor necrosis factor-alpha (TNF-alpha) and interleukin-1 beta (IL-1β) have been shown to sensitize nociceptors and promote neuroinflammation in chronic pain conditions like rheumatoid arthritis and neuropathic pain.
- Prostaglandins, produced by cyclooxygenase (COX) enzymes in response to tissue injury or inflammation, can enhance pain sensitivity by sensitizing nociceptors and promoting vasodilation and edema formation.
Role of Inflammatory Markers in Diagnosis and Treatment
Inflammatory markers play a crucial role in the diagnosis, monitoring, and treatment of chronic pain conditions associated with inflammation. These biomarkers provide valuable insights into the underlying inflammatory processes, helping clinicians assess disease activity, monitor treatment response, and guide therapeutic decision-making.
Advancements in diagnostic techniques and biomarker profiling have enabled the development of personalized treatment strategies aimed at targeting specific inflammatory pathways and improving patient outcomes.
Biomarkers of Inflammation in Chronic Pain Conditions
Various inflammatory markers are utilized in the assessment of chronic pain conditions to evaluate the presence and severity of inflammation, as well as to monitor disease progression and treatment response. Common inflammatory markers include
- Acute-phase reactants, such as C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR), which are elevated in response to systemic inflammation and tissue damage.
Elevated levels of CRP and ESR are often observed in conditions associated with acute and chronic inflammation, such as rheumatoid arthritis, systemic lupus erythematosus, and inflammatory bowel disease. Pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-alpha), interleukin-6 (IL-6), and interleukin-1 beta (IL-1β), play a central role in mediating inflammatory responses and are implicated in the pathogenesis of various chronic pain conditions.
Measurement of these cytokines in serum or synovial fluid provides valuable information about the inflammatory status of patients and may guide treatment decisions in diseases like rheumatoid arthritis and psoriatic arthritis.
Diagnostic Tests and Imaging Techniques
In addition to blood-based inflammatory markers, diagnostic tests, and imaging techniques are utilized to assess inflammation and tissue damage in chronic pain conditions. Imaging modalities such as ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT) scans enable the visualization of anatomical structures and the detection of inflammatory changes in joints, soft tissues, and organs.
These imaging techniques allow clinicians to identify joint erosions, synovitis, effusions, and other structural abnormalities associated with inflammatory arthritis, facilitating early diagnosis and treatment initiation.
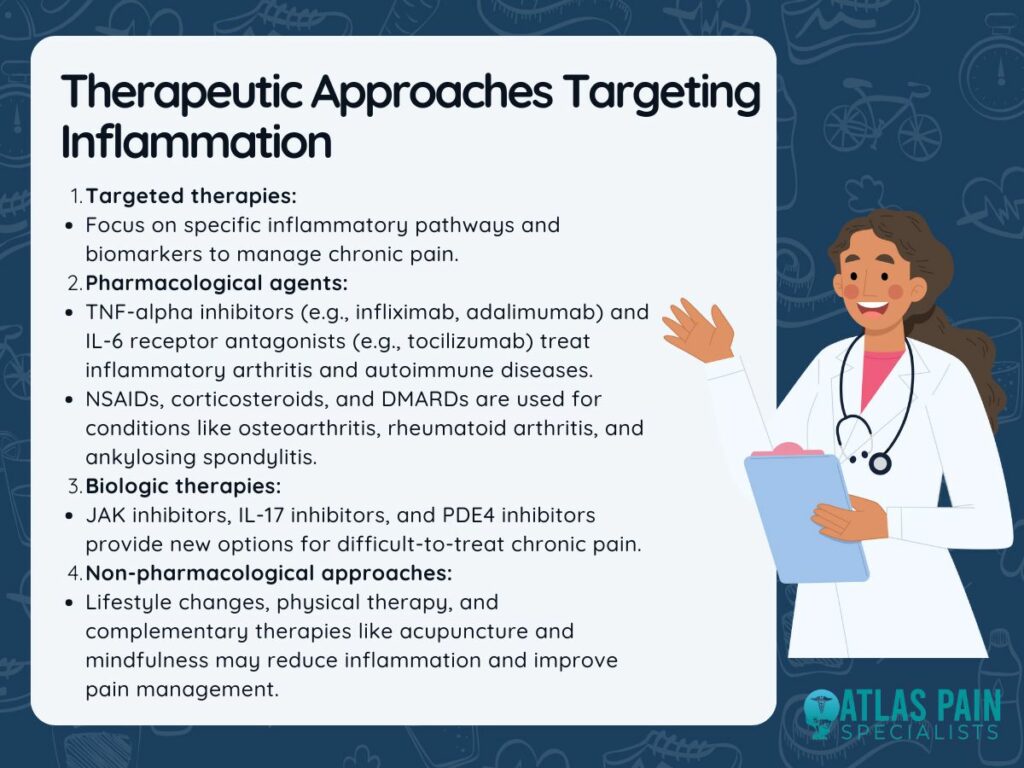
Therapeutic Approaches Targeting Inflammation
The identification of specific inflammatory pathways and biomarkers has paved the way for the development of targeted therapeutic interventions aimed at modulating inflammation and alleviating pain in chronic pain conditions.
- Pharmacological agents targeting pro-inflammatory cytokines, such as TNF-alpha inhibitors (e.g., infliximab, adalimumab) and IL-6 receptor antagonists (e.g., tocilizumab), have revolutionized the treatment of inflammatory arthritis and other autoimmune diseases by suppressing disease activity and preventing joint damage.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs) are commonly used to alleviate pain and inflammation in various chronic pain conditions, including osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis.
- Biologic therapies targeting specific inflammatory pathways, such as Janus kinase (JAK) inhibitors, interleukin-17 (IL-17) inhibitors, and phosphodiesterase-4 (PDE4) inhibitors, offer new treatment options for patients with refractory or inadequately controlled chronic pain conditions.
- Lifestyle modifications, physical therapy, and complementary therapies, such as acupuncture and mindfulness-based stress reduction, may help reduce inflammation and improve pain management in chronic pain patients.
Importance of Multimodal Treatment Approaches
While targeting inflammation is central to the management of chronic pain conditions, a multimodal treatment approach that addresses the multifactorial nature of pain is often necessary to achieve optimal outcomes. In addition to pharmacological interventions targeting inflammation, multimodal treatment strategies may include:
- Physical therapy
- Exercise
- Cognitive-behavioral therapy
- Dietary modifications
- Complementary therapies
Understanding Opioid Therapy for Chronic Pain
Knowing how inflammation and chronic pain correlate reveals an important part of pain pathophysiology that underlies many crippling conditions. The necessity of tailored and focused methods to pain management is highlighted by the understanding of the role that inflammatory markers play in diagnosis and treatment.
Biomarker profiling and advanced imaging techniques empower clinicians to assess disease activity, monitor treatment response, and tailor therapeutic interventions to individual patients. In the broader context of chronic pain management, understanding the limitations and risks associated with opioid therapy becomes significant.
While opioids can provide effective pain relief, their potential for addiction, overdose, and diversion necessitates a cautious and judicious approach to prescribing.
About Dr. Sean Ormond



