
Sciatica After Pregnancy: Causes, Symptoms, and Management
Pregnancy is a profound transformation journey, bringing about a myriad of physical and emotional changes. While the birth of a child is a joyous occasion, the postpartum period can sometimes usher in unexpected challenges.
One such challenge that often remains under-discussed is sciatica after pregnancy. This condition, characterized by a sharp, radiating pain down one leg, can be both surprising and debilitating for new mothers.
In this article, we'll delve into the causes of post-pregnancy sciatica, its tell-tale symptoms, and the various management strategies to help mothers easily navigate this discomfort and return to their daily routines.
Table of Contents
Understanding Sciatica
Pregnancy is a time of profound physical and hormonal changes, and while it brings the joy of impending motherhood, it can also introduce various discomforts. One such discomfort that some expectant mothers may encounter is sciatica.
Sciatica is not a condition but a symptom of an underlying issue affecting the sciatic nerve. This nerve is the longest in the human body, originating in the lower spine, passing through the buttocks, and extending down to the feet. When this nerve is compressed or irritated, it can lead to the characteristic symptoms of sciatica.
Understanding the relationship between sciatica and pregnancy can help better manage and potentially prevent this painful condition.
Deep Dive into the Causes of Sciatica After Pregnancy
Pregnancy is a transformative period marked by significant physiological and hormonal changes in a woman's life. While it's a time of joy and anticipation, it can also be accompanied by various discomforts, one of which is sciatica.
Understanding the causes of sciatica after pregnancy can help prevent and manage it.

1. Hormonal Changes:
- Relaxin's Prolonged Impact: While relaxin is crucial during pregnancy for loosening the pelvic ligaments in preparation for childbirth, its effects can linger postpartum. This continued ligament laxity can lead to spinal instability, potentially causing misalignment and subsequent pressure on the sciatic nerve.
- Estrogen and Progesterone: These hormones, which see fluctuating levels during and after pregnancy, can influence fluid retention and muscle tone, both of which can indirectly affect the sciatic nerve.
2. Weight Gain and Postural Changes:
- Postpartum Postural Adjustments: The body doesn't immediately return to its pre-pregnancy state after childbirth. The shifted center of gravity during pregnancy might have led to postural habits that persist postpartum, exerting strain on the spine and potentially the sciatic nerve.
- Pelvic Floor Strain: The strain on the pelvic floor muscles during childbirth can sometimes lead to muscle imbalances in the postpartum period. These imbalances can affect the alignment of the pelvis and spine, contributing to sciatica.
3. Birth Trauma:
- Delivery Interventions: Using forceps, vacuum extraction, or other interventions can sometimes lead to trauma in the pelvic region, potentially affecting the sciatic nerve.
- Positional Strain: Prolonged labor in certain positions can exert significant pressure on the pelvis and lower back, potentially leading to postpartum sciatic symptoms.
4. Expansion of the Uterus:
The uterus, a central organ in pregnancy, undergoes significant changes in size and position as it accommodates the growing fetus. While its expansion is a natural and essential part of pregnancy, it can have implications for the surrounding anatomical structures, including the potential to influence sciatica.
Even after childbirth, the uterus doesn't immediately return to its original size. This continued expansion can still exert pressure on nearby structures, including the sciatic nerve, especially if there's postpartum swelling.
5. Fluid Retention:
During pregnancy, the body produces approximately 50% more blood and body fluids to meet the needs of the developing fetus. However, this fluid doesn't disappear immediately after delivery; it takes time for the body to readjust and eliminate the excess.
Fluid retention, medically known as edema, is common during and after pregnancy. It involves the accumulation of excess fluids in the body's tissues, leading to swelling. This phenomenon can directly or indirectly impact the onset or exacerbation of sciatica in the postpartum period.
6. Pre-existing Spinal Issues:
The spine is a complex structure, and any pre-existing issues or abnormalities can become more pronounced during and after pregnancy, potentially leading to sciatica.
The physical demands of pregnancy, including weight gain, altered posture, and hormonal changes, can exacerbate underlying spinal conditions. Conditions like herniated discs, lumbar spinal stenosis, or spondylolisthesis might have been asymptomatic or mildly symptomatic before pregnancy.
The physical stresses of pregnancy and childbirth can exacerbate these conditions, leading to postpartum sciatica.
Symptoms of Sciatica: Beyond the Basics
While many are familiar with the hallmark pain of sciatica, the postpartum period can introduce nuances to these symptoms. The physical and hormonal changes accompanying pregnancy and childbirth can influence the manifestation and experience of sciatica.
Let's delve deeper into the more intricate aspects of post-pregnancy sciatica symptoms:
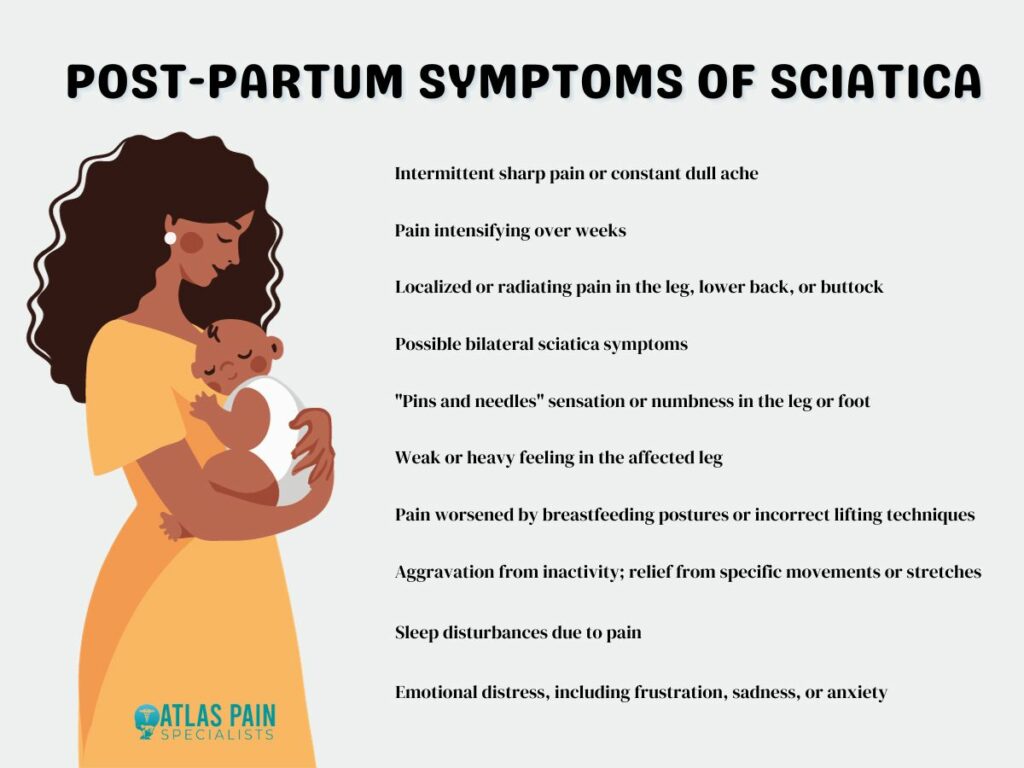
1. Nature of Pain:
- Intermittent vs. Constant: Some new mothers might experience sharp, jolting bouts of pain that come and go, while others might grapple with a persistent, dull ache.
- Evolution Over Time: Initially, the pain might be mild and infrequent, but it can intensify over weeks, especially without intervention or due to postural habits while caring for the baby.
2. Location and Spread:
- Localized vs. Radiating: While classic sciatica often presents as pain radiating down the leg, postpartum sciatica might sometimes feel more localized, especially in the initial stages, focusing on the lower back or buttock.
- Unilateral vs. Bilateral: Typically, sciatica affects one side of the body. However, in rare postpartum cases, if there's significant spinal stress or bilateral issues, symptoms might appear on both sides.
3. Associated Sensations:
- Tingling and Numbness: Beyond pain, some mothers describe a sensation akin to "pins and needles" or even complete numbness in certain areas of the leg or foot.
- Muscle Weakness: The affected leg might feel weak or heavy, making tasks like climbing stairs or even walking more challenging.
4. Aggravating and Alleviating Factors:
- Breastfeeding Postures: Certain positions while breastfeeding or bottle-feeding can exacerbate the pain, especially if the mother is not well-supported or if she sits in the same position for extended periods.
- Lifting the Baby: Incorrect postures while lifting or carrying the baby can strain the back further, intensifying sciatic symptoms.
- Rest and Movement: While rest is essential, prolonged inactivity can sometimes worsen symptoms. Gentle movements or specific stretches might offer relief.
5. Other Considerations:
- Sleep Disruptions: The pain and discomfort can disrupt sleep, a precious commodity for new mothers. This lack of rest can, in turn, affect the body's healing processes and pain perception.
- Emotional Impact: Chronic pain can influence mood, potentially leading to feelings of frustration, sadness, or anxiety. This emotional toll and typical postpartum hormonal fluctuations can be particularly challenging.
Understanding the nuanced symptoms of post-pregnancy sciatica is crucial for effective management and intervention. Recognizing these subtleties ensures that new mothers receive the tailored care they need, allowing them to focus on their recovery and the joys of motherhood.
Comprehensive Management Strategies
Managing sciatica after pregnancy requires a multifaceted approach that addresses both the physical and emotional challenges faced by new mothers. Here's a comprehensive guide to managing post-pregnancy sciatica:
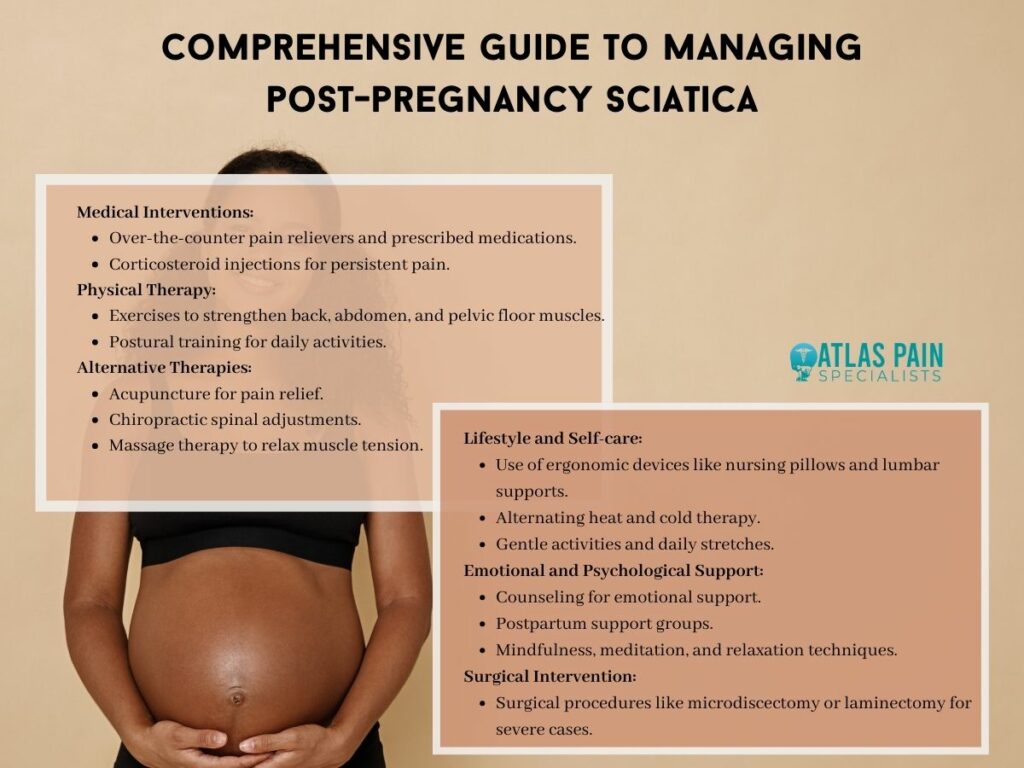
1. Medical Interventions:
- Medication: Over-the-counter pain relievers like ibuprofen can help reduce inflammation and pain. For more severe pain, doctors might prescribe stronger painkillers, muscle relaxants, or nerve pain medications. Always consult with a healthcare professional before taking any medications, especially if breastfeeding.
- Corticosteroid Injections: For persistent pain, corticosteroid injections around the nerve root area can help reduce inflammation and pain. However, their benefits are temporary, and there's a limit to how many can be given due to potential side effects.
2. Physical Therapy:
- Targeted Exercises: A physical therapist can guide new mothers through exercises that strengthen the back, abdomen, and pelvic floor muscles, providing better support to the spine and alleviating sciatic symptoms.
- Postural Training: Therapists can also teach proper postures for breastfeeding, lifting the baby, and other daily activities to reduce strain on the back.
3. Alternative Therapies:
- Acupuncture: This traditional Chinese medicine technique can help alleviate sciatic pain by stimulating specific points in the body.
- Chiropractic Care: Adjustments by a chiropractor can help improve spinal alignment and potentially relieve nerve compression.
- Massage Therapy: Regular massages can relax muscle tension, improve blood flow, and provide relief from sciatic pain.
4. Lifestyle and Self-care:
- Ergonomic Considerations: Using supportive devices like nursing pillows, ergonomic baby carriers, and lumbar supports can reduce strain on the back.
- Heat and Cold Therapy: Cold packs can reduce inflammation, while heat can relax muscles. Alternating between the two can offer relief.
- Regular Movement: Gentle activities like walking or swimming can help alleviate symptoms and prevent stiffness.
- Stretching: Daily stretches, especially for the lower back and hamstrings, can help relieve tension and reduce sciatic pain.
5. Emotional and Psychological Support:
- Counseling: Chronic pain can lead to feelings of frustration or sadness. Talking to a counselor or therapist can provide emotional support and coping strategies.
- Support Groups: Joining a postpartum support group can provide a platform to share experiences and learn from others facing similar challenges.
- Mindfulness and Relaxation: Techniques like meditation, deep breathing exercises, and progressive muscle relaxation can help manage pain and reduce stress.
6. Surgical Intervention:
While most cases of post-pregnancy sciatica resolve with conservative treatments, severe cases with significant nerve compression might require surgical intervention. Procedures like microdiscectomy or laminectomy can be considered if other treatments fail to provide relief.
Conclusion
The journey of motherhood, while filled with unparalleled joys, can also present unexpected physical challenges, with post-pregnancy sciatica being a notable concern for many. This condition, stemming from various physiological and hormonal shifts, can significantly impact a new mother's daily life.
However, with a comprehensive understanding of its causes and symptoms and a multifaceted approach to management, it's possible to navigate this discomfort effectively.
By prioritizing self-care, seeking timely medical interventions, and embracing both traditional and alternative therapies, mothers can find relief and fully immerse themselves in the joys and responsibilities of their new role.
About Dr. Sean Ormond