
The Link Between Mental Health and Chronic Pain
Have you ever felt like your mind and body are tangled in a mysterious dance of discomfort and distress? It's a journey many people silently navigate every day, yet its significance often remains overlooked or underestimated.
Today, we're delving into the intricate relationship between mental health and chronic pain. It's a link that's not always apparent at first glance, but once understood, it sheds light on the complexities of human experience and opens doors to holistic approaches in healthcare.
The Impact of Chronic Pain on Mental Health
Chronic pain, characterized by persistent discomfort lasting for more than three months, not only affects physical well-being but also takes a toll on mental health. The relentless presence of pain can lead to various psychological challenges, exacerbating existing conditions or even giving rise to new ones.
Understanding the profound impact of chronic pain on mental health is crucial for effective management and holistic care. Here are some key ways chronic pain affects mental well-being:

- Increased Stress Levels: Chronic pain triggers a heightened stress response in the body, leading to increased levels of cortisol, the stress hormone. This ongoing stress contributes to a vicious cycle, exacerbating both physical pain and mental distress.
- Depression and Anxiety Disorders: Living with chronic pain significantly increases the risk of developing depression and anxiety disorders. The relentless nature of pain, coupled with limitations in daily activities, social isolation, and fear of the future, can erode mental resilience and lead to profound feelings of sadness and apprehension.
- Substance Use Disorders: Individuals experiencing chronic pain may turn to substances like alcohol or opioids in an attempt to alleviate their symptoms or cope with the emotional distress caused by pain. However, reliance on such substances can quickly spiral into addiction, further complicating both the pain management process and mental health.
- Sleep Disturbances and Fatigue: Persistent pain often disrupts sleep patterns, leading to insomnia or fragmented sleep. Sleep disturbances not only exacerbate physical discomfort but also contribute to mental fatigue, irritability, and impaired cognitive function, perpetuating the cycle of pain and mental distress.
- Difficulty Concentrating and Decreased Appetite: The cognitive impact of chronic pain can manifest as difficulty concentrating, memory problems, and decreased mental clarity. Additionally, the emotional toll of pain may result in a loss of interest in food or decreased appetite, further compromising nutritional intake and overall well-being.
- Mood Changes and Frustration: Living with chronic pain can lead to frequent mood swings, irritability, and feelings of frustration or hopelessness. The inability to engage in activities once enjoyed, and the constant struggle to manage pain can erode emotional resilience and exacerbate feelings of helplessness.
Managing the Impact: Strategies and Support
Acknowledging the profound interplay between chronic pain and mental health is the first step towards effective management and support. Integrated approaches that address both physical and psychological aspects of pain management are essential. These may include:
- Multidisciplinary Treatment Plans: Collaborative efforts involving healthcare professionals from various disciplines, including pain specialists, psychologists, and physical therapists, can provide comprehensive care tailored to individual needs.
- Cognitive Behavioral Therapy (CBT): CBT techniques help individuals develop coping strategies, challenge negative thought patterns, and improve emotional regulation, enhancing resilience in the face of chronic pain.
- Support Groups and Peer Counseling: Connecting with others facing similar challenges can provide invaluable support, validation, and coping strategies.
- Medication Management: Judicious use of medications, including pain relievers, antidepressants, and anti-anxiety medications, under the guidance of healthcare professionals can help alleviate symptoms and improve overall well-being.
- Lifestyle Modifications: Incorporating stress-reduction techniques, regular exercise, adequate sleep hygiene, and healthy dietary habits can complement medical interventions and promote holistic well-being.
Prevalence of Mental Health Conditions in Those with Chronic Pain
Chronic pain affects millions of people worldwide, significantly impacting not only physical health but also mental well-being. The co-occurrence of mental health conditions in individuals with chronic pain is a well-documented phenomenon, shedding light on the complex interplay between physical and psychological factors.
Understanding the prevalence of these mental health conditions is crucial for providing comprehensive care and support to those living with chronic pain. Here's an overview of the prevalence of mental health conditions in individuals with chronic pain:
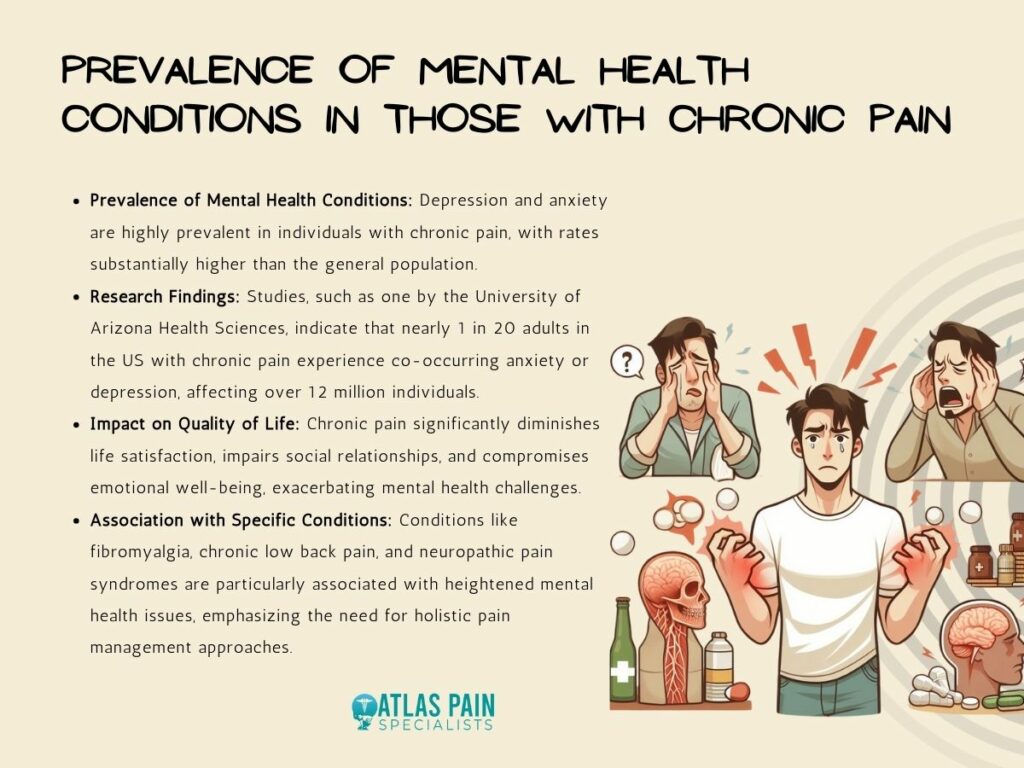
Depression and Anxiety in People with Chronic Pain
Depression and anxiety are among the most prevalent mental health conditions experienced by individuals with chronic pain.
Research suggests that the prevalence of depression and anxiety disorders is substantially higher in individuals with chronic pain compared to the general population. For example, a study by the University of Arizona Health Sciences found that nearly 1 in 20 adults in the United States experience the co-occurrence of chronic pain and anxiety or depression, affecting over 12 million adults.
The constant experience of pain, coupled with functional limitations and social isolation, can contribute to the development or exacerbation of these mood disorders.
Impact of Chronic Pain on Quality of Life
Chronic pain exerts a profound impact on the overall quality of life for individuals affected by it. Beyond the physical discomfort, chronic pain can lead to diminished satisfaction with life, impaired social relationships, and compromised emotional well-being.
The persistent struggle to manage pain and engage in daily activities can erode one's sense of purpose and fulfillment, further exacerbating mental health challenges.
Specific Conditions and Their Association with Mental Health Issues
Certain chronic pain conditions are particularly associated with heightened mental health issues. For example, fibromyalgia, characterized by widespread musculoskeletal pain, is often accompanied by significant psychological distress, including depression, anxiety, and decreased quality of life.
Similarly, chronic low back pain and neuropathic pain syndromes have been linked to an increased prevalence of mental health conditions, highlighting the importance of addressing both physical and psychological aspects of pain management.
Table: Prevalence of Mental Health Conditions in Chronic Pain
| Mental Health Condition | Prevalence in Chronic Pain Patients |
| Depression | Higher prevalence compared to the general population |
| Anxiety | Elevated rates, often co-occurring with depression |
| Decreased Quality of Life | Universally reported across various chronic pain conditions |
Treatment and Therapies for Chronic Pain and Mental Health
Effective management of chronic pain requires a comprehensive approach that addresses both physical discomfort and associated mental health challenges. Integrating treatments and therapies targeting mental well-being alongside traditional pain management strategies can significantly improve outcomes and enhance the overall quality of life for individuals living with chronic pain. Here are key treatment modalities for chronic pain and mental health:
A. Antidepressant Medications
Antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs), are commonly prescribed to individuals with chronic pain, particularly those experiencing co-occurring depression or anxiety.
These medications not only alleviate mood symptoms but also have analgesic properties, helping to reduce pain intensity and improve overall functioning.
B. Talk Therapy (Psychotherapy)
Talk therapy, also known as psychotherapy, is a valuable treatment modality for addressing both chronic pain and mental health issues. Cognitive-behavioral therapy (CBT) is particularly effective in helping individuals develop coping strategies, challenge negative thought patterns, and improve pain management skills.
Through regular sessions with a trained therapist, individuals can gain insight into the interplay between their thoughts, emotions, and pain experiences, leading to enhanced resilience and improved overall well-being.
C. Stress-Reduction Techniques, Physical Activity, Exercise, Meditation, Journaling, and Coping Skills
Incorporating stress-reduction techniques, physical activity, exercise, meditation, journaling, and coping skills into daily life can significantly improve both physical and mental well-being for individuals with chronic pain. These self-care practices promote relaxation, improve mood, and enhance overall quality of life.
Engaging in regular physical activity and exercise not only helps to strengthen muscles and improve flexibility but also releases endorphins, natural pain-relieving chemicals in the brain, leading to reduced pain perception and improved mood.
Similarly, mindfulness-based practices such as meditation and journaling can help individuals cultivate greater awareness of their thoughts and emotions, leading to reduced stress and enhanced emotional regulation.
D. Pain Rehabilitation Programs
Pain rehabilitation programs offer comprehensive, interdisciplinary approaches to chronic pain management, addressing both physical and psychological aspects of the condition. These programs typically involve a combination of medical interventions, physical therapy, occupational therapy, and psychological support. Through structured, goal-oriented interventions, individuals participating in pain rehabilitation programs learn to improve functional abilities, develop effective coping strategies, and optimize overall quality of life.
E. Importance of Mental Health Screening in Chronic Pain Treatment
Routine mental health screening is essential in the management of chronic pain to identify and address underlying psychological issues effectively. Early detection and intervention for depression, anxiety, and other mental health conditions can significantly improve treatment outcomes and promote holistic well-being.
By incorporating mental health screening into routine clinical assessments, healthcare providers can better understand the individual needs of patients with chronic pain and tailor treatment plans accordingly.
Table: Treatment and Therapies for Chronic Pain and Mental Health
| Treatment/Therapy | Description |
| Antidepressant Medications | SSRIs and TCAs alleviate mood symptoms and have analgesic properties, reducing pain intensity and improving functioning. |
| Talk Therapy (Psychotherapy) | CBT helps individuals develop coping strategies, challenge negative thought patterns, and improve pain management skills. |
| Stress-Reduction Techniques | Techniques such as meditation, exercise, and journaling promote relaxation, improve mood, and enhance overall well-being. |
| Pain Rehabilitation Programs | Interdisciplinary programs combine medical interventions, physical therapy, occupational therapy, and psychological support. |
| Mental Health Screening | Routine screening identifies underlying psychological issues, enabling early intervention and improved treatment outcomes. |
Integrated Solutions for Chronic Pain and Mental Health
Addressing the complex interplay between chronic pain and mental health requires integrated solutions that recognize the multifaceted nature of these conditions. Drawing insights from global mental health, transdiagnostic approaches, cultural idioms of distress, and person-centered care can enhance chronic pain management and promote holistic well-being. Here are key components of integrated solutions for chronic pain and mental health:
A. Lessons from Global Mental Health for Chronic Pain Management
Global mental health initiatives offer valuable lessons for chronic pain management, emphasizing the importance of contextually relevant, community-based interventions. Collaborative models involving healthcare providers, community leaders, and individuals affected by chronic pain can help identify culturally sensitive approaches to pain management and mental health support.
By leveraging existing infrastructure and resources, global mental health frameworks provide insights into enhancing access to care and reducing disparities in chronic pain management.
B. Transdiagnostic Approaches and Social Determinants
Transdiagnostic approaches recognize common underlying mechanisms across various mental health conditions and chronic pain, emphasizing shared vulnerability factors and treatment strategies.
Addressing social determinants of health, such as socioeconomic status, access to healthcare, and environmental factors, is crucial for improving outcomes in chronic pain and mental health. By adopting transdiagnostic frameworks and addressing social determinants, healthcare providers can better tailor interventions to individual needs and promote equitable care.
C. Cultural Idioms of Distress and Traditional Healing Practices
Acknowledging cultural idioms of distress and traditional healing practices is essential for providing culturally competent care to individuals with chronic pain and mental health concerns. Cultural beliefs and practices surrounding pain and illness influence help-seeking behaviors and treatment preferences.
Integrating traditional healing modalities, such as acupuncture, herbal medicine, and spiritual rituals, alongside evidence-based treatments can enhance treatment engagement and effectiveness. By fostering trust and collaboration, healthcare providers can honor diverse cultural perspectives and promote healing within communities.
D. Person-Centered Care and Shared Decision-Making
Person-centered care emphasizes collaboration between healthcare providers and individuals with chronic pain, prioritizing individual preferences, values, and goals. Shared decision-making empowers individuals to actively participate in treatment decisions, leading to greater satisfaction and improved outcomes.
By fostering open communication, mutual respect, and trust, healthcare providers can co-create personalized care plans that address both physical and psychological aspects of chronic pain. Person-centered approaches promote autonomy, dignity, and empowerment, fostering resilience and promoting recovery.
Conclusion
Understanding the deep connection between chronic pain and mental health unveils a pathway to holistic care. By recognizing how pain affects emotions and vice versa, we pave the way for integrated treatments that address both physical discomfort and psychological distress. With collaborative efforts and personalized approaches, we can improve the well-being of individuals living with chronic pain, enhancing their quality of life and promoting resilience.
About Dr. Sean Ormond



