Exploring Different Types of Pain: Nociceptive vs. Neuropathic
Hello there, ready to explore pain and learn together? We're about to dive into a fascinating world that we've all experienced but rarely stop to ponder – pain. Yes, that unmistakable sensation that ranges from a pesky paper cut to the throbbing discomfort of a toothache. But did you know that not all pain is created equal?
In this blog, we will peel back the layers of pain to reveal its two main protagonists: Nociceptive vs. Neuropathic pain. They might sound like scientific jargon, but understanding their differences can be a game-changer when managing and dealing with discomfort.
Nociceptive Pain
Pain, in all its forms, is a universal human experience. It's our body telling us that something isn't quite right. Yet, not all pain is created equal. In this segment, we will explore one of the two primary categories of pain - nociceptive pain. Let's dive in!
Definition and Explanation
Nociceptive pain arises from activating nociceptors, specialized nerve endings designed to detect harmful or potentially damaging stimuli. These stimuli can come in many forms, including mechanical, thermal, or chemical. When nociceptors sense these stimuli, they send signals to the brain, alerting us to the potential threat.
To put it simply, nociceptive pain is like an alarm system. When something potentially harmful happens to your body, these alarms go off to warn you, "Hey, something is not quite right here!"
Common Causes and Examples
Nociceptive pain can have various causes, and it's important to distinguish between them for effective treatment. Here are some common examples:
- Somatic Nociceptive Pain: This type of pain originates from the musculoskeletal system and is often described as aching or throbbing. It can result from fractures, sprains, or muscle strains.
- Visceral Nociceptive Pain: This originates from internal organs; visceral pain can be dull, crampy, or aching. Conditions like appendicitis or kidney stones can lead to visceral nociceptive pain.
- Superficial Nociceptive Pain: This type involves the skin and mucous membranes. Think of the pain from a sunburn, insect bite, or a cut on your finger.
How the Body Processes Nociceptive Pain
Understanding how the body processes nociceptive pain is crucial for grasping its impact on our well-being. When a harmful stimulus is detected by nociceptors, a series of events unfolds:
- Transduction: This is the initial step where nociceptors convert the noxious stimulus into an electrical signal.
- Transmission: The electrical signal travels along the nerves towards the spinal cord and then to the brain.
- Perception: In the brain, the signal is perceived as pain, alerting us to a potential threat.
- Modulation and Reaction: The brain can also modulate the perception of pain. For instance, the release of endorphins can lessen the pain's intensity.
Neuropathic Pain
Pain, in its many manifestations, is a shared human experience, serving as our body's signal that something may be amiss. However, it's important to recognize that not all pain falls into the same category. In this segment, we'll look closely at one of the primary types of pain - neuropathic pain. Let's delve in!
Definition and Explanation
Neuropathic pain is quite different from nociceptive pain. It stems from a dysfunction in the nervous system itself rather than an external threat. Nerves that misfire or send erratic signals can cause neuropathic pain. This type of pain is often described as burning, shooting, or electric shock-like sensations.
Common Causes and Examples of Neuropathic Pain
Neuropathic pain stems from abnormalities or damage to the nervous system, generating pain signals without an actual external threat. Here are some common causes and examples of neuropathic pain:
- Nerve Injury: Physical nerve injuries, such as compression, entrapment, or direct trauma, can result in neuropathic pain. A classic example is sciatica, where a herniated disc compresses the sciatic nerve, causing shooting pain down the leg.
- Diabetic Neuropathy: People with diabetes can develop neuropathic pain due to high blood sugar levels damaging nerve fibers. Symptoms often include burning or tingling sensations, typically in the extremities.
- Post-Herpetic Neuralgia: Following an episode of shingles, certain individuals may persistently experience intense burning or stabbing pain in the region where the shingles rash originally occurred.
- Phantom Limb Pain: This occurs in people who have undergone amputations. They may continue to feel pain, itching, or other sensations in the missing limb.
How the Body Processes Neuropathic Pain
Understanding the mechanisms of neuropathic pain is essential to comprehend its persistence and chronic nature. Unlike nociceptive pain, where the pain signals arise from external injuries or threats, neuropathic pain is characterized by abnormal signaling within the nervous system itself:
- Nerve Damage or Dysfunction: Neuropathic pain starts with nerve damage or dysfunction. This can result from physical trauma, diseases, or conditions affecting the nerves.
- Erratic Signaling: In neuropathic pain, damaged nerves send incorrect and erratic pain signals to the brain. This means that even non-painful stimuli can trigger pain sensations, resulting in symptoms like shooting, burning, or electrical shock-like pain.
- Central Sensitization: The brain's perception of pain becomes altered due to central sensitization. The brain may become more sensitive to pain signals, amplifying the perception of discomfort.
- Neuroplasticity: Over time, the nervous system may change in response to chronic pain, a phenomenon known as neuroplasticity. These changes can perpetuate and intensify the perception of pain.
- Chronicity: Neuropathic pain often becomes chronic because of these changes in nerve signaling, central sensitization, and neuroplasticity. Even after the initial cause of the pain is resolved, the pain signals can persist.
Key Differences Between Nociceptive and Neuropathic Pain
Understanding the key differences between nociceptive and neuropathic pain is crucial for effective management and treatment. These differences encompass the origin, characteristics, and diagnostic methods employed by healthcare professionals.
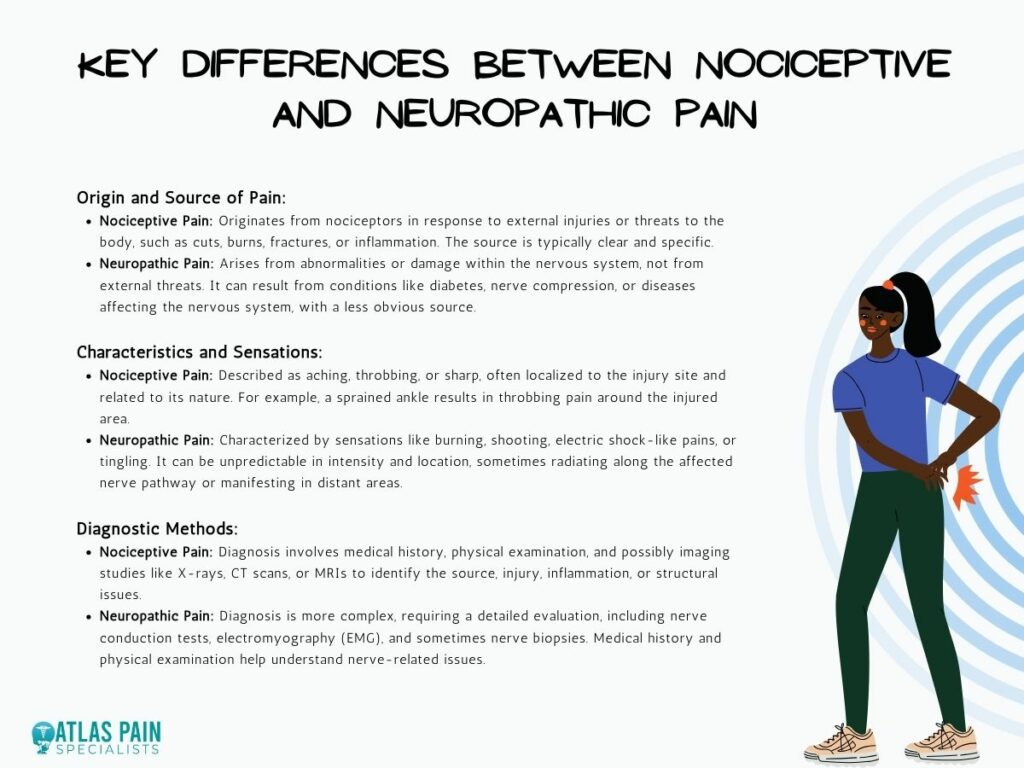
Origin and Source of Pain
- Nociceptive Pain: Nociceptive pain originates from activating nociceptors, specialized nerve endings designed to detect harmful or potentially damaging stimuli. This pain is typically a response to external injuries or threats to the body, such as cuts, burns, fractures, or inflammatory conditions. The source of nociceptive pain is usually clear and can be traced back to a specific injury or issue.
- Neuropathic Pain: In contrast, neuropathic pain stems from abnormalities or damage within the nervous system. It doesn't arise from external threats but from malfunctions or nerve injuries. The source of neuropathic pain can be less obvious and may result from conditions like diabetes, nerve compression, or diseases affecting the nervous system.
Characteristics and Sensations
- Nociceptive Pain: Nociceptive pain is typically described as aching, throbbing, or sharp. It often feels like a localized discomfort, and the sensation is in direct relation to the injury's location and nature. For example, a sprained ankle results in throbbing pain around the injured area.
- Neuropathic Pain: Neuropathic pain is characterized by sensations such as burning, shooting, electric shock-like pains, or tingling. Unlike nociceptive pain, neuropathic pain can be unpredictable in intensity and location. It may radiate along the affected nerve pathway or even manifest in areas distant from the source of nerve damage.
Diagnostic Methods
- Nociceptive Pain: Diagnosing nociceptive pain involves a thorough medical history, physical examination, and, in some cases, imaging studies like X-rays, CT scans, or MRIs to identify the source of the pain. Medical professionals may assess the injury, inflammation, or structural issues to make an accurate diagnosis.
- Neuropathic Pain: The diagnosis of neuropathic pain is often more complex. It requires a detailed medical evaluation, including nerve conduction tests, electromyography (EMG), and sometimes more specialized studies like nerve biopsies. The aim is to identify nerve dysfunction or damage as the source of the pain. Additionally, healthcare providers consider a patient's medical history and conduct a thorough physical examination to understand the extent of nerve-related issues.
Diagnosing and Identifying Nociceptive and Neuropathic Pain
Healthcare professionals typically begin with a comprehensive medical evaluation when diagnosing nociceptive and neuropathic pain. They take into account the patient's medical history, the onset and duration of the pain, and any underlying health conditions.
In the case of nociceptive pain, they focus on identifying external injuries or inflammatory processes, while for neuropathic pain, the emphasis is on understanding nerve function and possible damage.
Accurate diagnosis is paramount for effective pain management. Nociceptive and neuropathic pain require different treatment approaches, and misdiagnosis can lead to ineffective or even harmful treatments. Proper identification of the pain type ensures that patients receive interventions targeted at the root cause of their discomfort.
Treatment Approaches
Managing nociceptive pain involves addressing the underlying cause, reducing inflammation, and relieving the discomfort. Here are some common strategies:

- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can help alleviate pain and inflammation. Depending on the severity of the pain, over-the-counter options like ibuprofen or prescription medications may be recommended.
- R.I.C.E. Protocol: For injuries like sprains or strains, the Rest, Ice, Compression, and Elevation (R.I.C.E.) protocol can be effective. It reduces swelling and promotes healing.
- Physical Therapy: For chronic nociceptive pain, physical therapy can improve strength, flexibility, and mobility. It's often used after surgery or to rehabilitate an injury.
- Surgical Intervention: In cases of severe nociceptive pain caused by structural issues like a herniated disc or fractures, surgery may be necessary to correct the problem.
Neuropathic pain management is more complex, focusing on addressing nerve-related dysfunction. Treatment options include:
- Medications: Neuropathic pain is often managed with medications such as anticonvulsants, antidepressants, or opioids, depending on the severity and nature of the pain. These drugs can help modulate nerve signaling.
- Nerve Blocks: In some cases, nerve blocks, which involve injecting anesthetic or anti-inflammatory medications near the affected nerves, can provide relief.
- Neurostimulation: Techniques like spinal cord stimulation or peripheral nerve stimulation use electrical currents to interfere with pain signals and alleviate neuropathic pain.
- Physical Therapy: In some cases, physical therapy can help improve nerve function and reduce pain, especially when neuropathic pain is due to entrapment or compression.
Complementary and Alternative Therapies
Complementary and alternative therapies can be beneficial for both nociceptive and neuropathic pain:
- Acupuncture: Acupuncture involves the insertion of fine needles into specific points of the body to stimulate natural pain-relief mechanisms.
- Massage Therapy: Massage can promote relaxation and reduce muscle tension, which can be helpful for nociceptive pain, especially in cases of muscle strain.
- Meditation and Relaxation Techniques: Mindfulness meditation and relaxation exercises can help manage pain by reducing stress and promoting overall well-being.
Living with Nociceptive and Neuropathic Pain
Living with chronic pain, whether nociceptive or neuropathic, can be challenging. Coping strategies include:
- Pain Journal: Keeping a pain journal to track symptoms, triggers, and pain levels can help you and your healthcare team identify patterns and tailor your treatment plan accordingly.
- Physical Activity: Regular, gentle exercise can help manage pain by maintaining mobility, strength, and flexibility.
- Mental Health Support: Seeking support from mental health professionals or support groups can assist in managing the emotional toll of chronic pain.
Support Networks and Resources
Building a strong support network is crucial for those living with pain. This can include:
- Healthcare Providers: Develop a collaborative relationship with your healthcare team, including doctors, physical therapists, and pain management specialists.
- Family and Friends: Inform loved ones about your pain and ask for their support. Having a strong support system can make a significant difference.
- Support Groups: Consider joining local or online support groups where you can connect with others facing similar challenges.
Conclusion
Managing pain, whether nociceptive or neuropathic, involves a combination of medical treatments, complementary therapies, and coping strategies. Working closely with healthcare professionals to develop a personalized pain management plan that addresses your specific needs and improves your overall well-being is important.
Remember that you're not alone; resources and support are available to help you navigate the challenges of living with chronic pain.
About Dr. Sean Ormond