

Understanding the Causes and Symptoms of Leg Cramps
Leg cramps, commonly referred to as muscle spasms or Charley horses, are abrupt and often agonizing occurrences that catch individuals off guard, leaving them in search of immediate relief. While generally harmless, comprehending the causes and symptoms of leg cramps is crucial for effectively managing and preventing their onset.
In this article, we will explore the various factors contributing to leg cramps, ranging from dehydration to underlying health conditions, and identify the telltale signs that indicate a leg cramp is imminent. Additionally, we will discuss strategies for managing and preventing leg cramps, empowering individuals to take proactive measures to alleviate discomfort and improve their overall well-being.
Causes of Leg Cramps
Leg cramps, characterized by sudden and involuntary muscle contractions, can be attributed to various factors. Understanding these causes is essential for effectively managing and preventing leg cramps. Here are the common reasons behind the occurrence of leg cramps:

- Dehydration
Insufficient fluid intake can lead to dehydration, causing electrolyte imbalances in the body. This imbalance, particularly in potassium, magnesium, and calcium levels, can trigger muscle cramps, including those in the legs.

- Electrolyte Imbalance
Inadequate levels of essential minerals like potassium, magnesium, and calcium in the body can disrupt muscle function, increasing the likelihood of leg cramps. Electrolyte imbalances may result from factors such as excessive sweating, poor diet, or certain medical conditions.
- Overexertion
Engaging in intense physical activity or exercising without proper warm-up and stretching can strain the muscles, leading to fatigue and susceptibility to cramps. Overexertion can occur during sports, workouts, or repetitive movements in daily activities.

- Poor Blood Circulation
Conditions that impede blood flow to the legs, such as peripheral artery disease (PAD) or sitting in a cramped position for extended periods, can cause muscle cramps. Reduced blood circulation deprives muscles of oxygen and nutrients, leading to cramping.

- Muscle Fatigue
Prolonged or repetitive use of muscles, especially without adequate rest, can result in fatigue and increased susceptibility to cramps. Muscle fatigue may occur due to prolonged standing, walking, or physical labor.

- Certain Medications
Some medications, such as diuretics, statins, and antipsychotics, may have muscle cramps listed as a side effect. These medications can disrupt electrolyte balance or affect muscle function, contributing to the occurrence of leg cramps.
- Underlying Health Conditions
Certain medical conditions can predispose individuals to leg cramps. These include diabetes, thyroid disorders, nerve compression syndromes (e.g., sciatica), kidney disease, and neurological disorders (e.g., Parkinson's disease)



(e.g. Sciatica)


(e.g Parkinson's disease)
- Pregnancy
Pregnant women commonly experience leg cramps, especially during the later stages of pregnancy. Hormonal changes, increased weight, and changes in circulation can contribute to cramping in the legs and feet.

- Age
Older adults are more prone to leg cramps due to factors such as decreased muscle mass, reduced flexibility, and changes in circulation. Age-related conditions like arthritis or peripheral neuropathy can also increase the risk of cramps.

- Footwear and Posture
Wearing ill-fitting shoes or maintaining poor posture can put undue stress on the muscles of the legs and feet, leading to cramping.


Understanding these underlying causes of leg cramps can help individuals adopt preventive measures and lifestyle changes to reduce the frequency and severity of cramping episodes. Strategies such as staying hydrated, maintaining proper nutrition, avoiding overexertion, and addressing underlying health conditions can contribute to managing leg cramps effectively.
Symptoms of Leg Cramps
Understanding the factors contributing to leg cramps and recognizing their telltale signs empowers individuals to take proactive measures to alleviate discomfort and minimize the impact of these episodes on their daily lives.
Here are the common symptoms associated with leg cramps:
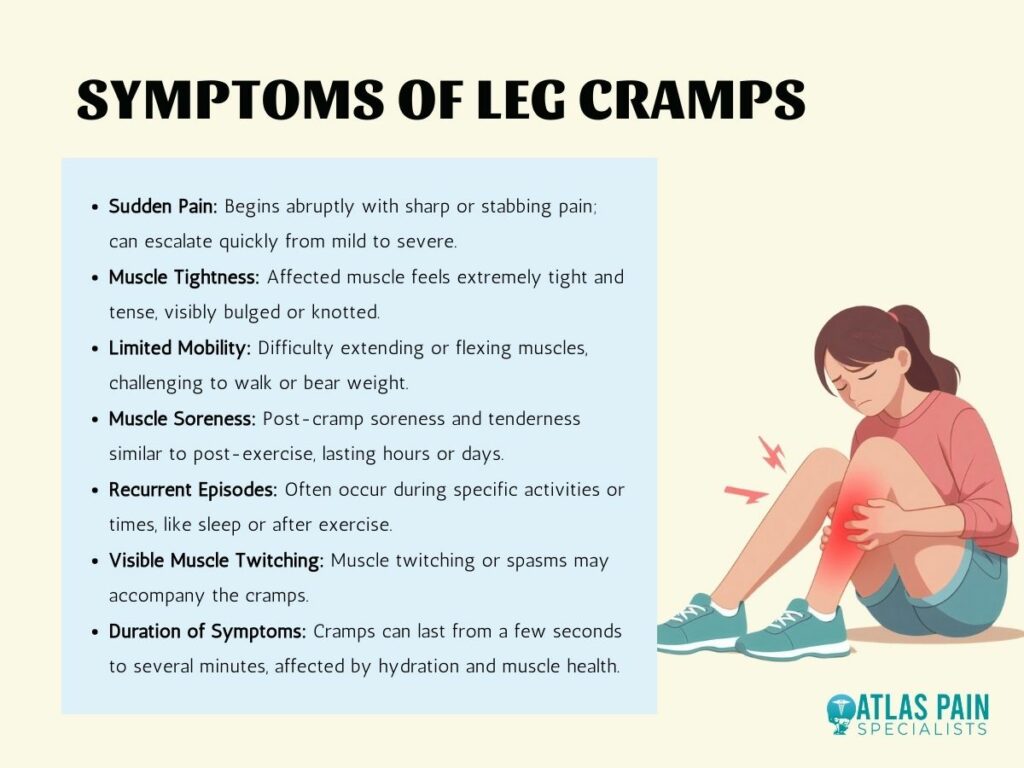
- Sudden Pain
Leg cramps typically begin abruptly with a sharp or stabbing pain in the affected muscle. This pain can range from mild to severe and may intensify rapidly.
- Muscle Tightness
During a leg cramp, the affected muscle may feel extremely tight and tense, as though it is contracting uncontrollably. This tightness can be visibly noticeable, with the muscle appearing visibly bulged or knotted.
- Limited Mobility
Leg cramps can restrict movement in the affected leg, making it challenging to extend or flex the muscles. Individuals may experience difficulty walking or bearing weight on the affected leg during a cramp.
- Muscle Soreness
After the leg cramp subsides, the affected muscle may continue to feel sore and tender for some time. This soreness is similar to the feeling of post-exercise muscle soreness and can persist for several hours or even days.
- Recurrent Episodes
Individuals who experience leg cramps may have recurrent episodes, particularly during certain activities or at specific times, such as during sleep or after vigorous exercise.
- Visible Muscle Twitching
In some cases, muscle twitching or spasms may accompany leg cramps, adding to the sensation of discomfort and tightness in the affected area.
- Duration of Symptoms
The duration of leg cramp symptoms can vary, with some cramps lasting only a few seconds while others persist for several minutes. The intensity and duration of symptoms may depend on the underlying cause of the cramp and individual factors such as hydration levels and muscle health.
Recognizing these symptoms can help individuals differentiate leg cramps from other types of muscle pain or discomfort and take appropriate measures to alleviate the symptoms.
Managing and Preventing Leg Cramps
Several strategies can help manage and prevent the occurrence of leg cramps effectively. By implementing these measures, individuals can alleviate discomfort and improve overall muscle health.
Here are some tips for managing and preventing leg cramps:

- Stay Hydrated
Proper hydration is essential for maintaining electrolyte balance and muscle function. Ensure adequate fluid intake throughout the day, particularly during physical activity or in hot weather. Water and electrolyte-rich beverages like sports drinks can help replenish fluids and prevent dehydration-induced cramps.
- Maintain Electrolyte Balance
Consume a balanced diet rich in potassium, magnesium, and calcium to support muscle health. Include foods such as bananas, leafy greens, nuts, seeds, dairy products, and fortified foods in your diet. If needed, consider supplements under the guidance of a healthcare professional, especially if you have known deficiencies or increased nutrient needs.
- Regular Stretching
Incorporate stretching exercises into your daily routine, focusing on the muscles prone to cramping, such as the calves, hamstrings, and quadriceps. Perform gentle stretches before and after physical activity and during breaks throughout the day. Stretching helps improve muscle flexibility and reduces the risk of cramps.
- Moderate Physical Activity
Engage in regular, moderate-intensity exercise to promote overall muscle health and circulation. Aim for a combination of aerobic activities (e.g., walking, swimming, cycling) and strength training exercises to strengthen muscles and improve endurance. Avoid sudden or excessive increases in activity intensity, which can increase the risk of cramps.
- Improve Blood Circulation
Practice activities that promote healthy blood flow to the legs, such as walking, cycling, or gentle leg exercises. Avoid prolonged periods of sitting or standing in one position, and take breaks to stretch and move around regularly. Elevating your legs while resting can also help improve circulation and reduce the risk of cramps.
- Review Medications
If you suspect that certain medications may be contributing to leg cramps, consult with your healthcare provider. They can review your medication regimen and make adjustments if necessary. In some cases, switching to alternative medications or adjusting dosages can help alleviate cramping symptoms.
- Treat Underlying Conditions
If you have underlying health conditions such as diabetes, peripheral artery disease, or thyroid disorders, work with your healthcare provider to manage these conditions effectively. Proper management of underlying health issues can help reduce the frequency and severity of leg cramps.
- Footwear and Posture
Wear comfortable, supportive footwear that fits well and provides adequate arch support. Avoid high heels and shoes with narrow-toe boxes, as they can strain the muscles and contribute to cramping. Practice good posture and avoid prolonged periods of standing or sitting in awkward positions.
Management strategies such as stretching, hydration, and maintaining electrolyte balance can help prevent and reduce the frequency of leg cramps, improving overall comfort and mobility. By incorporating these strategies into your daily routine, you can effectively manage and prevent leg cramps, improving your overall comfort and mobility.
Conclusion
In conclusion, leg cramps, characterized by sudden and involuntary muscle contractions, can be a challenging and uncomfortable experience for many individuals. However, by understanding the underlying causes and implementing preventive measures, it is possible to manage and reduce the occurrence of leg cramps effectively.
Strategies such as staying hydrated, maintaining electrolyte balance, regular stretching, engaging in moderate physical activity, improving blood circulation, reviewing medications, addressing underlying health conditions, and paying attention to footwear and posture can all contribute to alleviating discomfort and improving overall muscle health.
It is important to remember that while occasional leg cramps are common and generally harmless, frequent or severe cramps may indicate an underlying medical issue that requires further evaluation by a healthcare professional. Individuals can enhance their quality of life and maintain optimal muscle function and mobility by taking proactive steps to manage and prevent leg cramps.
About Dr. Sean Ormond



