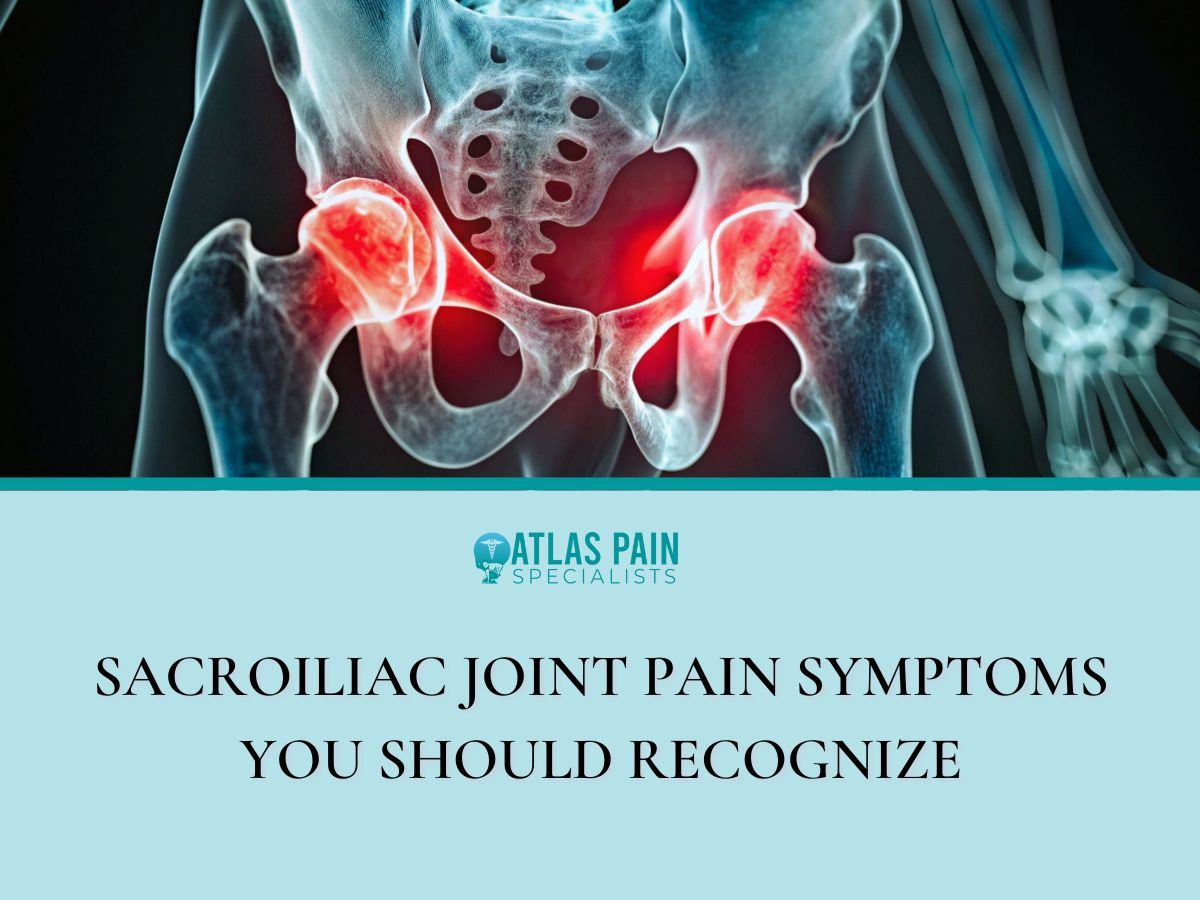
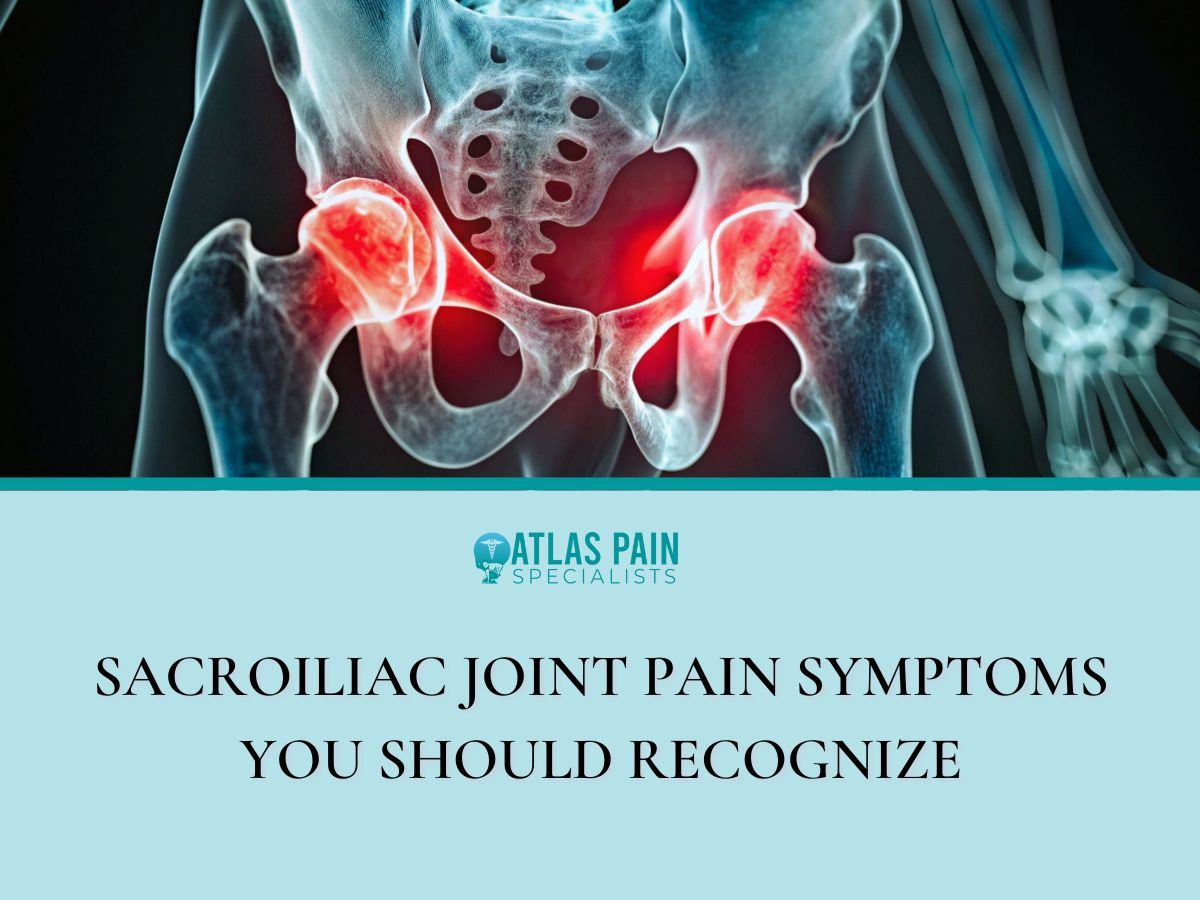
Sacroiliac Joint Pain Symptoms You Should Recognize
The sacroiliac joints form the critical mechanical link between the spine and the pelvis, transferring all gravitational forces from the upper body to the lower extremities. Their unique, limited range of motion provides essential stability for the entire lumbar-pelvic region during movement.
Despite their structural importance, these joints are a frequently underestimated source of chronic pain, commonly misattributed to lumbar disc pathology or hip osteoarthritis. Accurate recognition of the specific symptomatic pattern is the first necessary step toward effective clinical intervention.
Pain originating from these articulations presents with a distinct and reproducible set of sensory and mechanical characteristics. Identifying these clinical markers allows for differentiation from other musculoskeletal conditions with similar regional presentations. Below are sacroiliac joint pain symptoms you should recognize.
The Main Sign... Pain in a Very Specific Spot
The most reliable indicator of sacroiliac joint dysfunction is pain that localizes to a precise anatomical region. Unlike the diffuse ache of muscular strain or the radiating pain of neurogenic conditions, SI joint pain consistently presents over the joint itself.
Finding Your "Dimple Point"
Clinicians often refer to the posterior superior iliac spine, a bony landmark that correlates with the common dermal dimples found just lateral to the sacrum. The SI joints reside directly beneath this point.
This location is several centimeters lateral to the midline spinous processes of the lower lumbar vertebrae, a key distinction from central discogenic pain. Pain elicited by direct pressure over this specific landmark, particularly when it replicates the patient's primary complaint, provides strong diagnostic evidence for an SI joint etiology.
The "One-Sided" Clue
While bilateral involvement occurs, especially in systemic inflammatory conditions, mechanical SI joint dysfunction typically manifests unilaterally. This lateralized presentation stems from asymmetrical loading or a specific inciting injury that alters the mechanics of a single joint.
The resultant pain remains predominantly on the affected side, though compensatory mechanisms can sometimes create secondary discomfort on the contralateral side over time. This one-sided predominance helps differentiate it from many forms of central spinal stenosis or systemic back pain.
Pain That Stays Put
The referral pattern of SI joint pain further distinguishes it. The discomfort may radiate, but its epicenter remains anchored to the joint.
Patients can usually isolate the primary source with a single fingertip, a clinical sign known as the "finger test."
- The characteristic radiation patterns include the ipsilateral buttock, the posterior thigh, and occasionally the groin region.
- Pain that extends below the knee, or is accompanied by true neurologic symptoms like numbness or muscle weakness, suggests a different or concomitant pathology, such as lumbosacral radiculopathy.
- This stable, locatable quality contrasts sharply with the migrating or shooting pain associated with nerve root compression.
How the Pain Feels and When it Strikes
The qualitative nature of SI joint pain and its temporal relationship to specific activities form a critical part of its clinical profile. This pain is not a constant, uniform sensation but a dynamic experience defined by its mechanical triggers and variable intensity.
- A Deep, Dull Ache That Can Sharpen
Patients frequently describe a persistent, deep-seated ache within the buttock and pelvic region, which can be difficult to localize precisely at rest. This baseline discomfort originates from the joint's deep anatomical position and the surrounding ligamentous structures.
The pain characteristically transitions to a sharp, stabbing, or even gripping sensation during movements that directly load or torque the joint. This shift from a dull ache to acute pain with specific provocation is a hallmark feature, indicating mechanical stress on inflamed or dysfunctional articular and periarticular tissues.
- Pain That Worsens with Simple Activities
Aggravation by specific, common weight-bearing and transitional movements provides strong diagnostic clues.
- Standing from a Seated Position: This action places immediate, unilateral load on the SI joint as the body weight shifts. The transition often requires a forceful contraction of the gluteal muscles, which attach directly to the sacrum and ilium, further compressing the joint.
- Stair Climbing or Walking on an Incline: These activities demand repeated single-leg stances with a propulsive force, maximally engaging the kinetic chain that relies on SI joint stability.
- Prolonged Standing or Walking: Even level-ground ambulation can become problematic, as the repetitive minor rotations and shear stresses accumulate, leading to increasing pain and a consequent antalgic gait.
- Lying on the Affected Side: Direct pressure on the inflamed joint structures during sleep can provoke pain, frequently disrupting rest and causing nocturnal awakening.
The pain is often most severe during activities that create shear forces across the joint or require a single-leg stance.
- Stiffness After Rest
A period of immobility, such as prolonged sitting or sleep, often results in notable stiffness and pain upon the initial movements. This post-static stiffness occurs as the synovial fluid within the joint and the surrounding connective tissues become less pliable.
The first several steps after rising from a chair or getting out of bed in the morning are typically the most difficult and painful. This stiffness usually diminishes with gentle, progressive movement but reliably returns after another cycle of rest, forming a predictable pattern of discomfort.
The Surprising Ways the Pain Can Travel
The referral pattern of sacroiliac joint pain can complicate diagnosis, as it frequently mimics other common musculoskeletal and neurological conditions. This discomfort follows predictable pathways due to the shared nerve supply and biomechanical connections of the pelvic region, but it maintains distinguishing boundaries.
- Not Sciatica... But It Can Mimic It
A primary source of diagnostic confusion stems from the SI joint's ability to refer pain into the buttock and down the posterior thigh. This pattern arises from irritation of the lumbosacral nerve roots, which also innervate the joint itself, or from compensatory muscle spasms in the piriformis and gluteal regions.
The critical distinction lies in the nature and extent of the radiation. SI joint referral typically produces a deep, aching discomfort that rarely extends beyond the knee.
It generally lacks the sharp, electric, or burning quality of true radicular pain and is not associated with neurological deficits such as dermatomal numbness, specific muscle weakness, or loss of reflexes.
- Confusion with Hip Pain
Groin and lateral hip pain are common presentations of both SI joint dysfunction and primary hip pathology, such as osteoarthritis. The proximity of the anterior SI joint ligaments to the hip joint capsule, and the shared biomechanical role in weight-bearing, create this overlap.
A key differentiating factor is the location of maximal tenderness. Hip joint pathology typically elicits pain deep in the anterior groin, often worsened by internal rotation of the hip.
In contrast, SI joint pain centers posteriorly over the sacral sulcus, and its aggravating movements involve direct pelvic stress rather than isolated hip motion. Tests that load the SI joint without moving the hip, such as the FABER test, help clarify the source.
- Groin and Pelvic Discomfort
Referred pain can also manifest in the lower abdomen, groin, and even the upper lateral thigh due to irritation of the L2-L4 nerve roots that contribute to the SI joint's innervation. This pattern is particularly noted in cases of significant anterior SI ligament strain or inflammation.
- This discomfort is often described as a deep, vague ache rather than a sharp pain.
- It can be mistakenly attributed to visceral issues, sports hernias, or urological conditions, leading to unnecessary consultations and diagnostic tests.
- The presence of concurrent, more definitive posterior pelvic pain over the joint itself is the essential clue that points toward an SI joint origin for anterior symptoms.
Signs You Might Notice in Your Daily Movements
Beyond direct pain, sacroiliac joint dysfunction often presents with subtle, functional disturbances that manifest during routine activities. These signs reflect the joint's compromised role in providing a stable foundation for movement, leading to protective neuromuscular adaptations and a conscious avoidance of specific positions.
- Feeling "Unstable" or Like Your Leg Might Give Way
A common patient report is a subjective sensation of pelvic instability or a fear that the leg on the affected side will unexpectedly buckle during weight-bearing. This is not typically true muscular weakness detectable on manual muscle testing, but rather a proprioceptive disturbance and a neuromuscular guarding response.
The brain perceives instability in the core pelvic stabilizer, leading to a protective inhibition or altered firing pattern in the larger lower extremity muscles during dynamic tasks. Patients may describe a lack of trust in their stance on that side, especially when transitioning quickly or standing on uneven surfaces.
- Trouble Finding a Comfortable Position
Discomfort from SI joint stress is often posture-dependent, making sustained positions challenging. Patients frequently describe an inability to sit evenly, habitually shifting their weight off the painful side or perching on one buttock.
They may sit with their legs crossed in a specific pattern to unload the joint. In a supine position, lying flat on the back can sometimes increase lordotic stress on the joint, prompting individuals to place a pillow under their knees.
This constant postural adjustment is a direct effort to reduce compressive or shear forces on the inflamed articulation, and the search for relief becomes a persistent feature of daily life.
- Pain with Routine Transitions
Specific, often mundane, transitional movements become notable sources of pain due to the asymmetric loading they impose on the pelvis.
- Getting In and Out of a Car: This action requires a controlled, twisting transfer of weight with one leg fixed, placing direct rotational stress on the SI joint.
- Rolling Over in Bed: The uncoordinated, often reflexive motion of turning during sleep engages core and hip musculature that pulls on the pelvis, frequently jolting the joint and causing sharp pain that can awaken the individual.
- Bending Forward: Activities like tying shoes, washing one's face at a sink, or loading a dishwasher involve a forward flexion motion that can strain the posterior sacroiliac ligaments, especially when performed with the legs straight.
Best Sleeping Positions for Sacroiliac Joint Pain Relief
A precise diagnosis of sacroiliac joint dysfunction remains the essential prerequisite for effective long-term management, separating it from other spinal and pelvic pathologies. The unique pattern of localized pain and functional limitation directs targeted treatment strategies that address both joint inflammation and core instability.
This specific symptom profile directly informs practical adjustments in daily life, particularly during extended periods of rest. For instance, sleeping on the painful side applies compressive force to the inflamed joint, and sleeping on the back with straight legs can increase lumbar lordosis, straining the sacroiliac ligaments.
Therefore, optimizing sleep posture becomes a critical component of conservative care, aiming to minimize nocturnal irritation. Positions that maintain neutral spinal alignment and reduce shear forces across the pelvis, such as side-lying with strategic pillow support between the knees or supine with a cushion under the legs, can help prevent morning stiffness and pain flare-ups.
About Dr. Sean Ormond