
Dorsal Root Ganglion Stimulation Procedure: How It Works
Living with chronic nerve pain can affect how you move, sleep, and manage daily responsibilities, including caring for your home and family. When pain becomes constant, knowing your treatment options becomes part of protecting your quality of life and long-term well-being.
You may have heard about different nerve stimulation options and felt unsure about what actually separates one from another. Confusion often comes from treatments being grouped together, even though they work in very different ways and target pain at different points in the nervous system.
Many people assume nerve stimulation treatments are either experimental or meant only as a last resort, which leads to confusion and hesitation. Others believe all stimulation therapies work the same way, without realizing how much precision can matter for certain types of pain. Let's look at how the dorsal root ganglion stimulation procedure.
- What the dorsal root ganglion does in your body
Your nervous system controls how pain reaches your brain, even when the source feels small or localized. When pain lingers or feels out of proportion, the issue often lies in how those signals travel rather than where they start.
This part of the body rarely gets attention because you cannot see or feel it directly. Still, it plays a major role in why certain pain stays sharp, focused, and difficult to manage with common treatments.
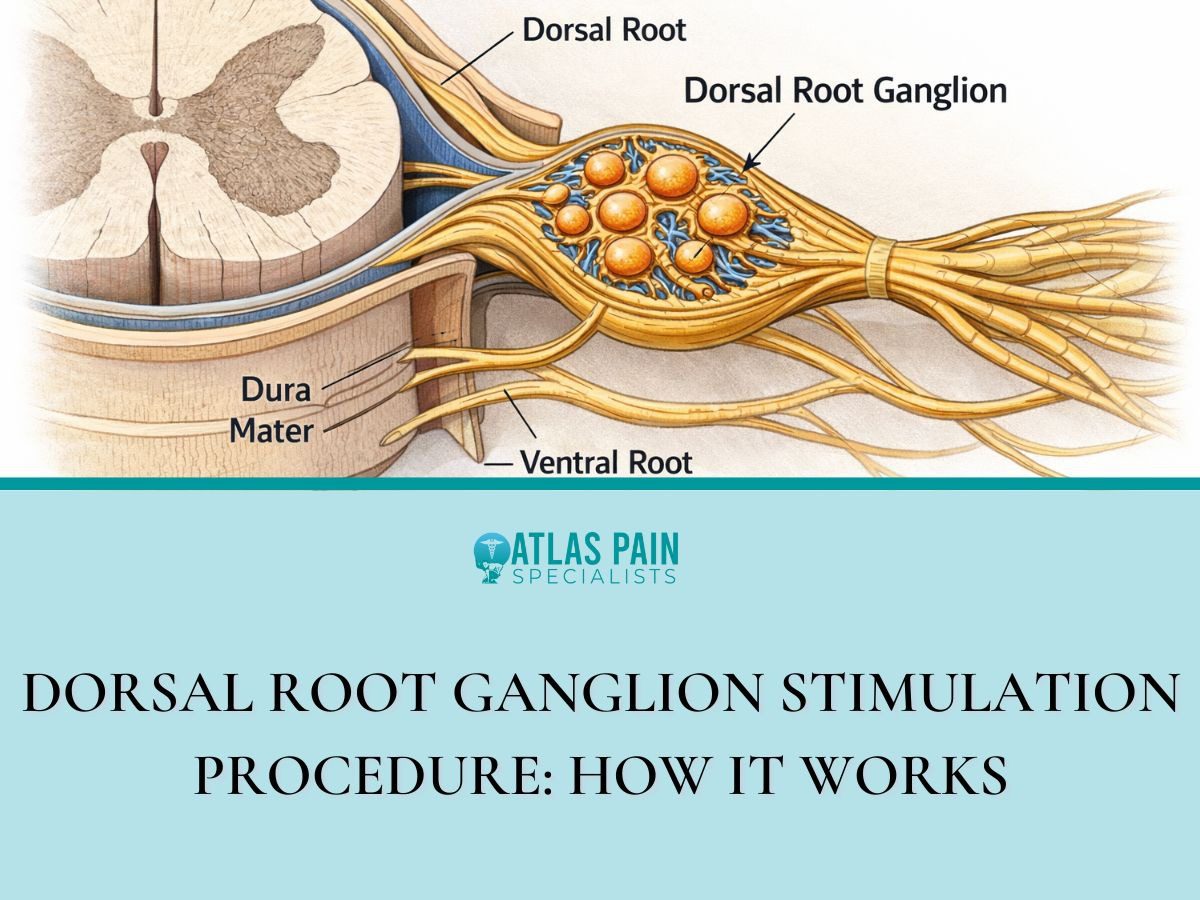
What the dorsal root ganglion actually is
The dorsal root ganglion is a small cluster of nerve cells located just outside the spinal cord. It acts as a checkpoint where sensory information, including pain, enters the central nervous system.
Because many pain signals pass through this area, even minor disruption here can change how strongly pain registers. When this checkpoint stays overactive, pain can feel constant or exaggerated.
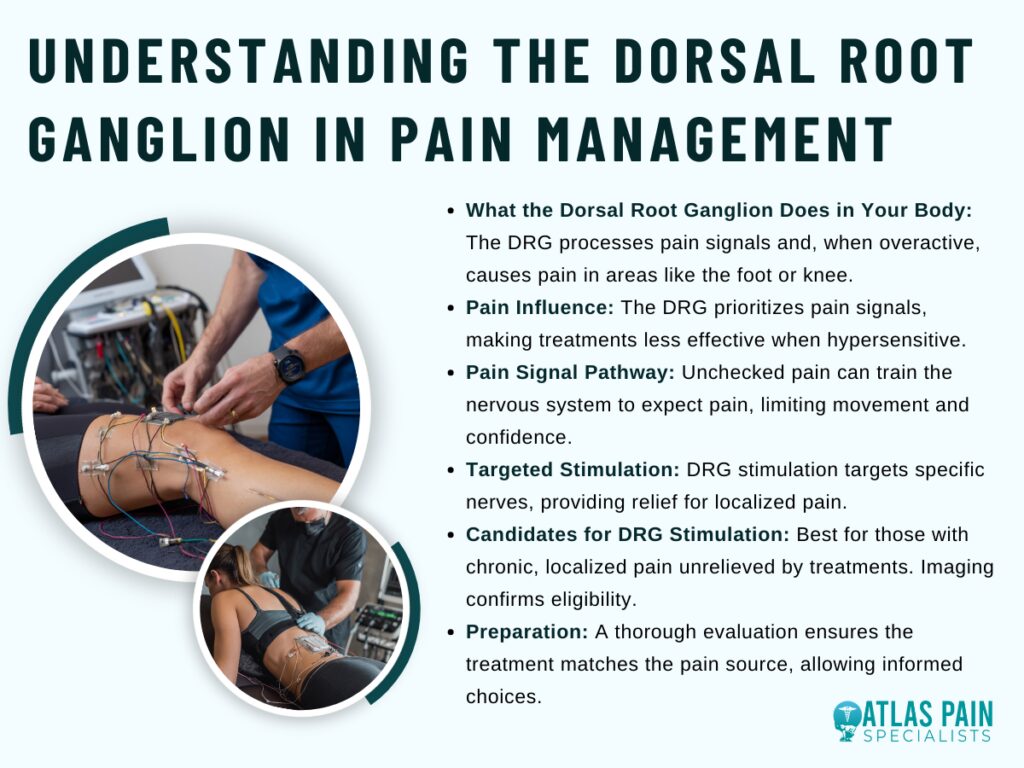
Why it influences pain more than other nerve areas
This structure handles very specific sensory input from defined parts of your body. That specificity means pain does not spread randomly but stays locked into certain regions like a foot, knee, or groin.
When the dorsal root ganglion becomes hypersensitive, those signals gain priority over others. Ignoring this mechanism often leads to treatments that dull sensation broadly but never fully address the source.
What happens when pain signals pass through unchecked
Pain signals that move freely through this area reach the brain without interruption. Over time, that steady input can train your nervous system to expect pain even during normal movement.
This response can limit mobility and confidence, even when tissue damage remains minimal. Addressing the signal pathway itself can reduce that cycle instead of masking it.
- Why this therapy is different from other nerve pain treatments
Different types of nerve pain respond differently to different treatments, and that can feel frustrating when options start to blur together. Targeted approaches exist because broad solutions often leave certain pain patterns untouched.
You may have tried treatments that helped briefly or reduced pain in some areas but not others. This difference usually comes down to how precisely the therapy interacts with the nerve pathways involved.
How targeted stimulation changes the approach
This therapy focuses on influencing pain signals at a very specific entry point into the nervous system. Instead of affecting wide regions of the spine, it concentrates on the exact nerves responsible for your pain.
That focus allows relief without numbing surrounding areas. When pain stays localized, precision often matters more than strength.
How it compares to traditional spinal cord stimulation
Traditional spinal cord stimulation works by covering larger nerve regions to reduce pain perception. While that method helps many people, it can struggle with pain that remains sharp and confined.
This therapy offers more control over where stimulation occurs. Without that control, certain pain patterns continue despite multiple adjustments.
Why precision can lead to more consistent relief
Precise placement allows stimulation to stay aligned with your pain even as you move. That consistency can reduce the ups and downs often felt with broader treatments.
When therapy shifts with posture or activity, relief becomes unpredictable. Addressing the signal at its source can create steadier results over time.
- Who may be a good candidate for DRG stimulation
Chronic pain does not follow one pattern, which makes choosing the right treatment feel overwhelming. Some approaches work best when pain stays focused in one area rather than spreading or changing day to day.
Knowing who this therapy tends to help can save time, cost, and frustration. It also allows you to have a more productive conversation with a specialist instead of trying options through trial and error.
Pain types that often respond well to this therapy
This therapy commonly helps pain that stays confined to a specific region of the body. Conditions involving nerve injury or nerve sensitivity in areas like the foot, knee, groin, or lower leg often fit this profile.
Because the pain remains localized, targeted stimulation can address it directly. Treating this kind of pain with broad methods can leave relief incomplete.
When other treatments have not provided lasting relief
Many candidates reach this option after medications, injections, or physical therapy fail to provide consistent improvement. Temporary relief often signals that the pain pathway itself remains active.
This therapy addresses that pathway rather than symptoms alone. Continuing the same treatments despite limited results can delay meaningful progress.
Health and evaluation factors that influence eligibility
Your overall health, prior procedures, and pain history play a role in determining suitability. Imaging and nerve mapping help confirm whether the pain pathway aligns with this approach.
Careful evaluation reduces the risk of unnecessary procedures. Skipping this step can lead to treatment that never fully matches your condition.
- What happens before the procedure
Preparing for this procedure involves more than scheduling a date and showing up. The steps beforehand shape how effective the therapy can be and help avoid surprises later.
Taking time to evaluate your pain and your goals allows the care team to tailor the approach to you. This phase also gives you space to ask questions and decide with confidence rather than pressure.
How your pain is evaluated and mapped
Your provider reviews where your pain starts, how it feels, and what makes it better or worse. Imaging and nerve assessments help connect your symptoms to specific nerve pathways.
This process clarifies whether the pain aligns with the area this therapy targets. Skipping detailed evaluation can lead to treatment that misses the true source.
Why a trial stimulation is part of the process
A trial allows you to experience the therapy before committing to a permanent device. Temporary leads test how well targeted stimulation reduces your pain during normal activity.
This step helps confirm benefit in real-life conditions rather than theory. Moving forward without a trial increases uncertainty about results.
Planning and preparation before the implant
Once the trial shows improvement, planning focuses on lead placement and device positioning. Instructions before the procedure help reduce infection risk and support smoother recovery.
Clear preparation also sets expectations for activity and follow-up. Poor planning often leads to unnecessary delays or complications.
- What happens before the procedure
Before anything physical takes place, the focus stays on clarity and alignment. This stage exists to make sure the treatment fits your pain pattern and your expectations, not just a diagnosis on paper.
Time spent preparing often determines how confident you feel moving forward. It also reduces the chance of pursuing a solution that does not truly match what your body needs.
How your pain story gets carefully reviewed
Your provider starts by listening to how your pain shows up in daily life, not just where it hurts. Details like consistency, triggers, and past treatments help narrow the nerve pathway involved.
Imaging and clinical findings then support that picture. Without this level of review, treatment can aim at the wrong target.
Why a trial phase comes before anything permanent
The trial phase gives you firsthand experience with how targeted stimulation affects your pain. Temporary leads allow you to test relief during normal movement and routine activities.
This step confirms real-world benefit rather than relying on assumptions. Skipping a trial increases the risk of committing to something that feels right in theory but not in practice.
How planning and preparation shape the outcome
Once the trial shows meaningful improvement, planning becomes more specific. Placement strategy, timing, and pre-procedure instructions all factor into how smoothly things progress.
Proper preparation supports comfort and reduces avoidable complications. Rushing this phase can limit the long-term success of the therapy.
- Step by step look at the DRG stimulation procedure
Going into the procedure can feel intimidating if you only picture surgery or hospital visits. Knowing the steps beforehand can help you feel more in control and prepared for what actually happens.
The procedure itself is designed to be precise while minimizing disruption to your daily life.
How the procedure begins and what to expect
You arrive at the facility after following pre-procedure instructions, such as fasting or adjusting medications. Sedation or local anesthesia helps you stay comfortable while remaining aware enough to respond if needed.
The team ensures the environment is sterile and that monitoring is in place. Attention to these details keeps the process safe and focused.
Placement of the leads and device
Leads are carefully guided to the area near the dorsal root ganglion where pain signals enter the nervous system. Imaging tools confirm the precise location, and adjustments happen as needed.
Once the leads sit correctly, the device is positioned and secured. Accurate placement is crucial for consistent pain relief.
Testing and final adjustments during the procedure
After placement, stimulation is tested to confirm that the targeted area responds as expected. Minor adjustments can be made on the spot to optimize relief.
The team observes your response closely before completing the procedure. Taking this step seriously improves the chances of long-term success.
- How the stimulation actually reduces pain
The therapy works by interrupting the way pain signals travel from your body to your brain. Instead of affecting large areas, it focuses on the specific nerves causing the discomfort, which can make relief more precise and consistent.
This targeted approach allows you to regain control over movements that previously triggered sharp or persistent pain. By managing the signals before they reach your brain, daily activities can feel less limited and more predictable.
How electrical signals interact with the dorsal root ganglion
Leads deliver mild electrical pulses directly to the nerve cluster responsible for your pain. These pulses adjust how the nerves communicate, reducing the intensity of the signals that reach your brain.
When the signals are tempered, you experience less discomfort during everyday motion. Ignoring this mechanism can leave traditional therapies less effective.
Why targeting a specific nerve cluster matters
Pain often follows predictable paths along certain nerves, and the dorsal root ganglion handles input from a defined area of your body. By focusing stimulation on this cluster, relief can stay localized rather than affecting unrelated regions.
This precision matters for chronic or sharp pain that does not respond well to broader therapies. Without targeted intervention, pain may continue despite multiple treatment attempts.
How consistent stimulation supports long-term relief
Keeping the stimulation aligned with the affected nerves allows pain control to remain steady over time. Adjustments can be made to match changes in activity or posture, maintaining effectiveness throughout the day.
This steady control helps prevent sudden flare-ups and supports more predictable daily function. Neglecting regular adjustments can reduce the therapy’s benefit.
What is Spinal Cord Stimulation and How Can It Relieve Pain?
Dorsal root ganglion stimulation can give you more confidence in managing chronic nerve pain. This therapy focuses on the precise pathways where pain signals travel, which often makes relief more targeted and consistent than broader approaches.
Spinal cord stimulation relates closely to this process because it also targets nerve signals to reduce pain, but it works over a broader area rather than focusing on a single nerve cluster. By comparing the two, you can see how the choice of therapy depends on the type and location of your pain.
Thinking about how targeted nerve therapies function connects directly to practical outcomes, like improving your ability to perform everyday tasks without constant discomfort. When you understand the mechanisms behind both dorsal root ganglion and spinal cord stimulation, you can communicate more effectively with your provider and track your progress.
About Dr. Sean Ormond



