
How to Treat Menopause Joint Pain
Menopause joint pain is best managed through a mix of healthy lifestyle habits, targeted exercise, balanced nutrition, and, when needed, medical treatments like hormone therapy or anti-inflammatory medication. Combining movement, an anti-inflammatory diet, and proper hydration can help reduce discomfort and improve mobility.
This guide explains how to treat menopause joint pain. We will look at why menopause can trigger joint pain, its common symptoms, risk factors and effective relief options from supplements and natural remedies to medical care. You’ll also learn when it’s time to consult a doctor for lasting joint health.
The Connection: Why Menopause Causes Joint Pain
During menopause, many women experience new or worsening joint discomfort. This is not just a normal part of aging — hormonal changes play a major role in how the joints feel and function.
1. Declining Estrogen Levels
Estrogen helps reduce inflammation, maintain cartilage, and keep joints lubricated. When levels drop during menopause, the protective effect weakens, making joints more prone to stiffness, swelling, and pain.
2. Loss of Muscle Mass and Bone Density
Aging and hormonal changes can lead to sarcopenia (muscle loss) and osteoporosis, which reduce joint support and increase the risk of wear-and-tear injuries. This can make everyday movements more taxing on the joints.
3. Increased Inflammation and Weight Gain
Lower estrogen levels can trigger a rise in inflammatory chemicals in the body. Combined with weight gain common in menopause, this puts extra pressure on weight-bearing joints like the knees and hips.
Understanding these connections can help women take proactive steps — from targeted exercise to hormone management — to protect joint health and ease discomfort during menopause.
Treatment Approaches for Menopause Joint Pain
Managing menopause joint pain often requires a multi-faceted approach that combines lifestyle adjustments, nutritional support, natural therapies, and, when needed, medical care. The aim is to reduce inflammation, strengthen the body’s support structures, and prevent long-term joint damage.
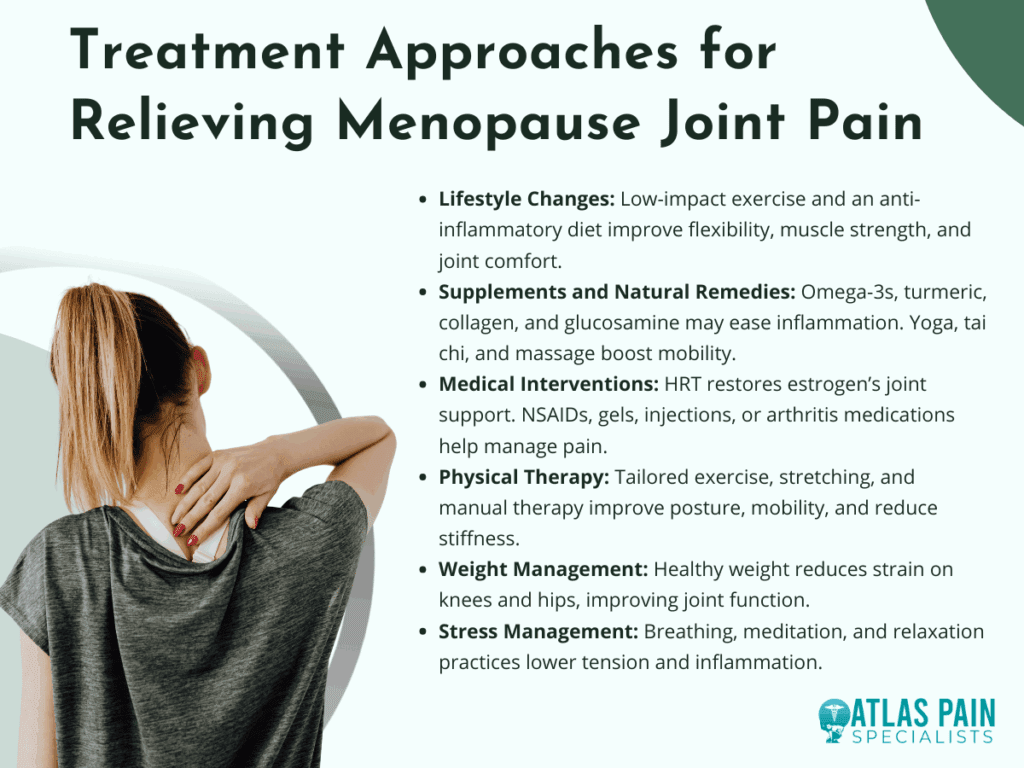
1. Lifestyle Changes
Regular low-impact exercises such as swimming, walking, Pilates, or cycling help maintain flexibility and strengthen the muscles that protect joints. Coupling physical activity with an anti-inflammatory diet rich in vegetables, omega-3s, and lean proteins can improve mobility and reduce discomfort.
2. Supplements and Natural Remedies
Omega-3 fatty acids, turmeric, collagen peptides, and glucosamine may support joint structure and decrease inflammation. Complementary therapies like acupuncture, yoga, tai chi, and massage can improve circulation, flexibility, and overall comfort.
3. Medical Interventions
Hormone Replacement Therapy (HRT) may help restore estrogen’s anti-inflammatory benefits and protect cartilage health. For pain management, doctors may recommend NSAIDs, topical anti-inflammatory gels, corticosteroid injections, or medications for arthritis-related conditions.
4. Physical Therapy and Rehabilitation
A physical therapist can create a tailored exercise plan to strengthen joint-supporting muscles, improve posture, and enhance mobility. Targeted stretching and manual therapy can also help reduce stiffness and pain.
5. Weight Management
Maintaining a healthy weight reduces the load on weight-bearing joints like the knees and hips, easing discomfort. Even modest weight loss can significantly improve mobility and joint function.
6. Stress Management
Chronic stress can increase inflammation and make pain feel more intense. Techniques such as deep breathing, meditation, and progressive muscle relaxation can help reduce tension and support overall joint health.
By combining these strategies, women can take control of menopause-related joint pain, improve daily comfort, and protect their mobility well into the future.
Symptoms to Watch For
Menopause joint pain can develop gradually or appear suddenly, often affecting daily comfort and mobility. Recognizing early warning signs helps in addressing the problem before it becomes more severe.
1. Morning Stiffness
Many women notice their joints feel tight and difficult to move upon waking. This stiffness typically eases with gentle activity but may return after periods of inactivity.
2. Joint Swelling and Tenderness
Reduced estrogen can lead to inflammation, causing joints to appear puffy or feel warm to the touch. Swelling often makes movement uncomfortable and can limit range of motion.
3. Clicking or Grinding Sensations
Loss of cartilage or changes in joint lubrication can cause cracking or popping sounds during movement. While not always painful, these sensations may signal early joint wear.
4. Reduced Flexibility and Range of Motion
Joints may feel less mobile, making activities like climbing stairs or bending more difficult. This stiffness can progress without targeted stretching or exercise.
5. Persistent Aching or Pain
Discomfort may occur during activity or at rest, affecting knees, hips, shoulders, or smaller joints in the hands. Over time, this can interfere with sleep and daily tasks.
Identifying these symptoms early allows for quicker treatment, which can help preserve joint function and prevent long-term damage. Monitoring changes in your body is key to managing menopause-related joint issues effectively.
Risk Factors for Menopause-Related Joint Pain
Certain factors can increase the likelihood of experiencing joint pain during menopause. Understanding these risks can help you take preventive steps and make lifestyle choices that protect joint health.
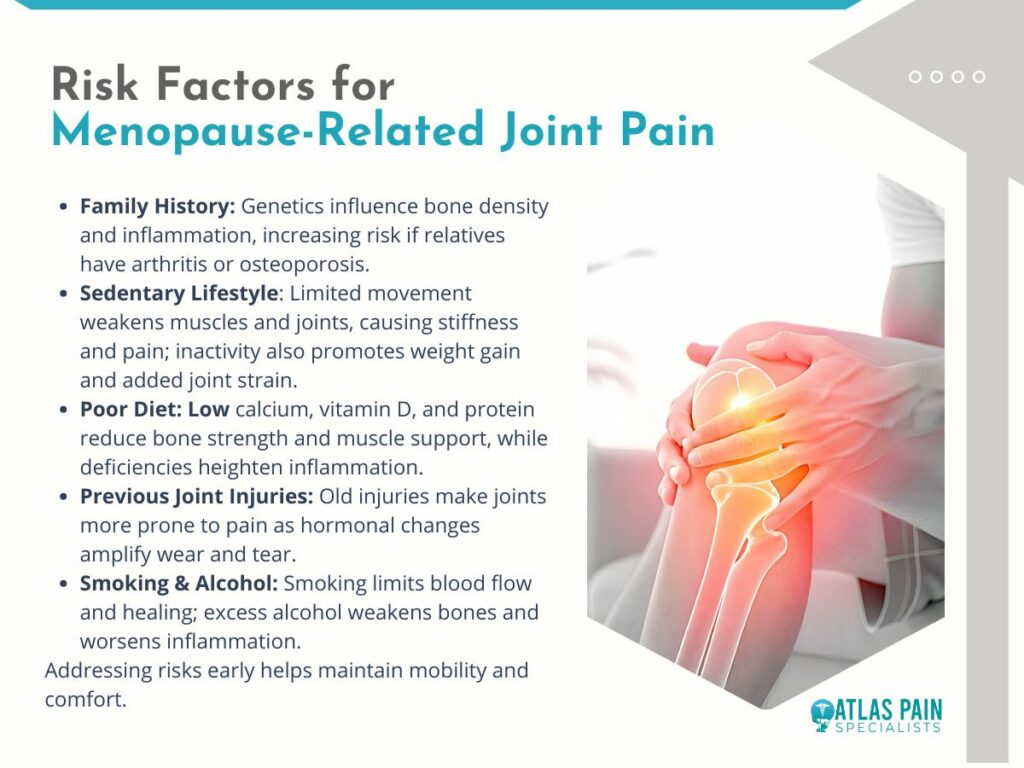
1. Family History of Arthritis or Osteoporosis
Genetics can play a strong role in joint health, influencing cartilage strength, bone density, and inflammatory responses. If close relatives have these conditions, your risk may be higher during menopause.
2. Sedentary Lifestyle
Lack of regular movement weakens muscles and reduces joint flexibility, making them more vulnerable to stiffness and pain. A sedentary routine can also contribute to weight gain, adding extra strain to joints.
3. Poor Diet Lacking Essential Nutrients
Diets low in calcium, vitamin D, and protein can weaken bones and muscles, reducing the body’s ability to support and protect joints. Nutrient deficiencies may also increase inflammation.
4. Previous Joint Injuries
Old injuries can leave joints more susceptible to wear and tear over time. Menopause-related changes may worsen discomfort or stiffness in these areas.
5. Smoking and Excessive Alcohol Use
Smoking reduces blood flow to joints, slowing healing and increasing inflammation. Excess alcohol intake can also weaken bones and contribute to poor joint health.
Recognizing your risk factors is the first step toward prevention. By addressing lifestyle habits early, you can reduce your chances of experiencing severe menopause joint pain and protect your mobility for years to come.
Natural and Alternative Remedies
Natural and alternative approaches can complement medical treatment for menopause joint pain, helping to reduce inflammation, improve flexibility, and support overall well-being. These options often focus on whole-body balance and gentle, non-invasive care.
1. Acupuncture
This traditional Chinese therapy involves inserting fine needles into specific points to stimulate healing and reduce inflammation. Many women report improved mobility and less joint discomfort after regular sessions.
2. Massage Therapy
Targeted massage can relieve muscle tension around affected joints, improve blood flow, and promote relaxation. Regular sessions may also help reduce stiffness and improve range of motion.
3. Yoga and Tai Chi
These gentle, low-impact practices improve flexibility, strengthen muscles, and promote better posture. They also enhance mindfulness, which can help manage the perception of pain.
4. Herbal Supplements
Turmeric, ginger, and Boswellia are known for their natural anti-inflammatory properties. When taken appropriately, they may reduce swelling and joint discomfort, though consultation with a healthcare provider is advised.
5. Heat and Cold Therapy
Applying heat can relax muscles and improve circulation, while cold packs help reduce swelling and numb sharp pain. Alternating between the two may offer additional relief.
Integrating natural remedies into your routine can provide extra support in managing menopause joint pain, especially when combined with healthy lifestyle habits and medical guidance. Always consult a professional before starting new treatments to ensure they’re safe for your individual needs.
Medical Treatment Options
When lifestyle changes and natural remedies are not enough, medical treatments can help address the root causes of menopause joint pain and provide stronger symptom relief. These approaches are best tailored to each individual’s health needs and risk factors.
1. Hormone Replacement Therapy (HRT)
HRT can help restore estrogen levels, reducing inflammation and supporting joint health. It may also relieve other menopause symptoms, though it’s important to discuss potential risks and benefits with a healthcare provider.
2. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Over-the-counter options like ibuprofen or naproxen can ease pain and reduce swelling. They are useful for flare-ups but should be taken as directed to avoid side effects.
3. Topical Anti-Inflammatory Treatments
Gels or creams containing diclofenac or capsaicin can be applied directly to painful joints. These provide targeted relief with fewer systemic side effects than oral medications.
4. Corticosteroid Injections
For severe pain or inflammation, doctors may recommend steroid injections into the affected joint. These can offer fast relief, though repeated use is generally limited due to potential joint damage.
5. Prescription Medications for Arthritis
If menopause symptoms overlap with arthritis, disease-specific medications may be prescribed. These help manage inflammation and slow joint damage progression.
Medical interventions can be highly effective when used alongside healthy lifestyle habits. Working closely with a healthcare provider ensures you choose the safest and most effective options for your situation.
When to Seek Urgent Medical Care
While most menopause-related joint pain can be managed with lifestyle changes and regular care, certain symptoms may indicate a more serious condition. Prompt medical attention can prevent complications and ensure proper treatment.
- Sudden, Severe Joint Pain - Intense pain that comes on quickly could signal a serious injury, infection, or inflammatory flare-up requiring immediate evaluation.
- Visible Joint Deformity - Any sudden change in joint shape or alignment may indicate dislocation, fracture, or advanced arthritis that needs urgent care.
- Signs of Infection - Redness, warmth, swelling, and fever around a joint can point to a joint infection, which is a medical emergency.
- Unexplained Fever with Joint Pain - This combination can indicate an underlying inflammatory or infectious condition that requires prompt testing and treatment.
- Loss of Mobility or Function - Inability to bear weight or move a joint normally may mean structural damage or severe inflammation that needs immediate attention.
If you notice any of these symptoms, seek medical care right away to prevent long-term damage and address potential underlying health issues.
Bottom Line
Menopause joint pain may be a natural result of hormonal changes, but it doesn’t have to limit your quality of life. With the right mix of lifestyle adjustments, natural remedies, and medical care, it’s possible to reduce discomfort, improve mobility, and protect joint health for the long term.
Listening to your body, addressing symptoms early, and working closely with a healthcare provider are key to effective management. By taking proactive steps, you can stay active, independent, and pain-free well beyond menopause.
About Dr. Sean Ormond



