Fibromyalgia and Cold Weather: Tips for Managing Symptoms
Cold weather can significantly impact individuals living with fibromyalgia, often exacerbating symptoms such as pain, stiffness, and fatigue. As temperatures drop, many report heightened discomfort due to muscle tension and reduced mobility.
The interplay of cold temperatures, humidity changes, and fluctuating barometric pressure can intensify sensitivity and lead to increased pain levels. This article will explore practical tips for coping with fibromyalgia symptoms during the winter months, helping individuals maintain their well-being despite the challenges posed by colder weather.
Understanding Fibromyalgia and the Impact of Cold Weather
Fibromyalgia is a chronic condition that affects the way the brain processes pain difficulties. While the exact cause remains unknown, researchers believe it results from a combination of genetic, environmental, and psychological factors.
One of the signals leading to widespread musculoskeletal pain, fatigue, and cognitive challenging aspects of fibromyalgia is its unpredictability—symptoms can vary from day to day, often triggered by factors such as stress, poor sleep, and weather changes
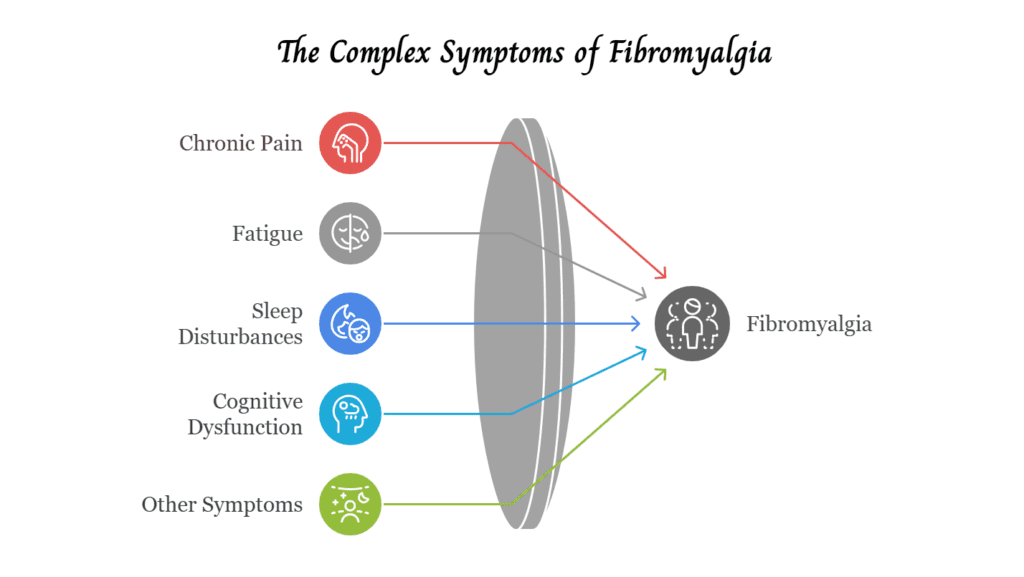
Definition and Symptoms
Fibromyalgia is characterized by widespread pain that lasts for at least three months, affecting both sides of the body and multiple muscle groups. People with fibromyalgia often describe their pain as a deep, persistent ache accompanied by burning or stabbing sensations.
Along with chronic pain, fibromyalgia causes fatigue, sleep disturbances, and cognitive dysfunction, commonly referred to as “fibro fog,” which affects memory, focus, and mental clarity. Other symptoms may include headaches, irritable bowel syndrome (IBS), tingling or numbness in the extremities, and heightened sensitivity to stimuli such as noise, light, and temperature.
Prevalence of Fibromyalgia
Fibromyalgia affects approximately 2-4% of the population, with women being disproportionately affected. Studies suggest that about 80-90% of fibromyalgia patients are women, although men and children can also develop the condition.
The onset often occurs in middle age but can begin earlier, especially after physical trauma, infections, or periods of significant stress. Since there is no definitive diagnostic test, many patients endure years of unexplained symptoms before receiving a diagnosis.
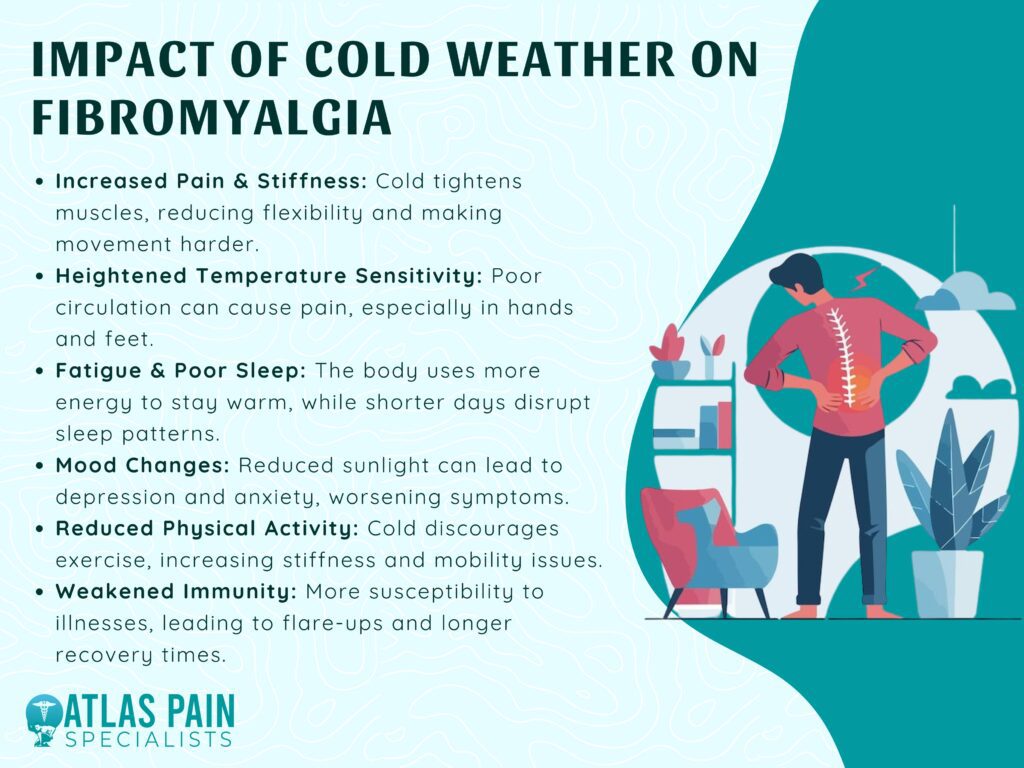
Impact of Cold Weather on Fibromyalgia
For many people with fibromyalgia, changes in the weather can significantly impact their symptoms. Cold temperatures, in particular, tend to worsen pain, stiffness, and fatigue, making winter months especially challenging.
| Weather Factor | Effect on Fibromyalgia | Common Symptoms |
|---|---|---|
| Cold Temperatures | Tightens muscles, reduces flexibility | Increased pain, stiffness, muscle cramps |
| Humidity Changes | Alters pain perception | More widespread aches, swelling |
| Lower Barometric Pressure | Expands joint tissues, increases nerve sensitivity | Deep aching pain, headaches, joint discomfort |
| Shorter Daylight Hours | Reduces serotonin & vitamin D levels | Fatigue, depression, worsened "fibro fog" |
| Winter Illnesses (Flu/Colds) | Weakened immune response | Longer recovery time, increased fatigue |
While researchers have not pinpointed an exact reason for this weather sensitivity, several factors contribute to the increased discomfort experienced by fibromyalgia patients during colder seasons.
1. Increased Muscle Stiffness and Pain
One of the most commonly reported issues during cold weather is increased muscle stiffness and joint pain. Lower temperatures can cause muscles to tighten and contract, reducing flexibility and making movement more painful.
People with fibromyalgia already experience widespread pain, and the added stiffness can make it harder to perform daily activities. Simple tasks like getting out of bed, walking, or even holding a cup of coffee can become more difficult when muscles feel tight and sore.
2. Heightened Sensitivity to Temperature Changes
People with fibromyalgia often have an altered pain perception, which extends to temperature sensitivity. Many report that their bodies struggle to regulate temperature effectively, making them feel excessively cold or warm compared to others.
Cold temperatures can trigger vasoconstriction, a narrowing of the blood vessels that reduces circulation, causing increased pain and discomfort in the hands and feet. Even minor drafts or exposure to cold air can cause discomfort, making it difficult to spend time outdoors or in air-conditioned environments.
3. Increased Fatigue and Poor Sleep Quality
Cold weather can also contribute to increased fatigue, which is already a major symptom of fibromyalgia. The body exerts more energy to keep warm in lower temperatures, leading to greater exhaustion.
Additionally, shorter daylight hours in winter can disrupt sleep patterns, as reduced sunlight exposure affects melatonin production and the body’s internal clock. Poor sleep exacerbates fibromyalgia symptoms, creating a cycle where increased fatigue leads to worse pain and cognitive fog.
4. Weather-Related Mood Changes
Seasonal changes can also impact mood and mental well-being. Seasonal Affective Disorder (SAD) is a type of depression linked to reduced sunlight exposure in colder months, and many fibromyalgia patients experience increased anxiety and depression in winter.
Stress and negative emotions can further intensify pain perception, making symptoms harder to manage. Feeling isolated indoors due to the cold can also contribute to a sense of loneliness or frustration, especially for those who rely on outdoor activities for relaxation and exercise.
5. Reduced Physical Activity
Exercise is one of the most effective ways to manage fibromyalgia symptoms, as it helps maintain muscle strength, flexibility, and overall well-being. However, cold weather often discourages physical activity.
Outdoor walking, swimming, and stretching routines may become less accessible, leading to increased stiffness and decreased mobility. The inactivity can also contribute to weight gain, which may further aggravate symptoms.
6. Immune System Challenges
Cold weather also coincides with flu season, increasing the likelihood of viral infections. Since fibromyalgia patients often have weaker immune responses, catching a cold or flu can lead to a flare-up of symptoms, including increased pain, extreme fatigue, and worsened cognitive issues.
Many report that even minor illnesses take longer to recover from, making winter illnesses a bigger challenge for those with fibromyalgia.
Coping Strategies for Managing Symptoms in Cold Weather
1. Dress in Warm, Layered Clothing
Since people with fibromyalgia are often more sensitive to temperature fluctuations, wearing warm, layered clothing can help regulate body temperature.
Opt for thermal wear, fleece, and wool fabrics that retain heat, and avoid materials that irritate the skin. Gloves, scarves, and thick socks can prevent vasoconstriction (narrowing of blood vessels) and keep hands and feet warm, reducing pain and discomfort.
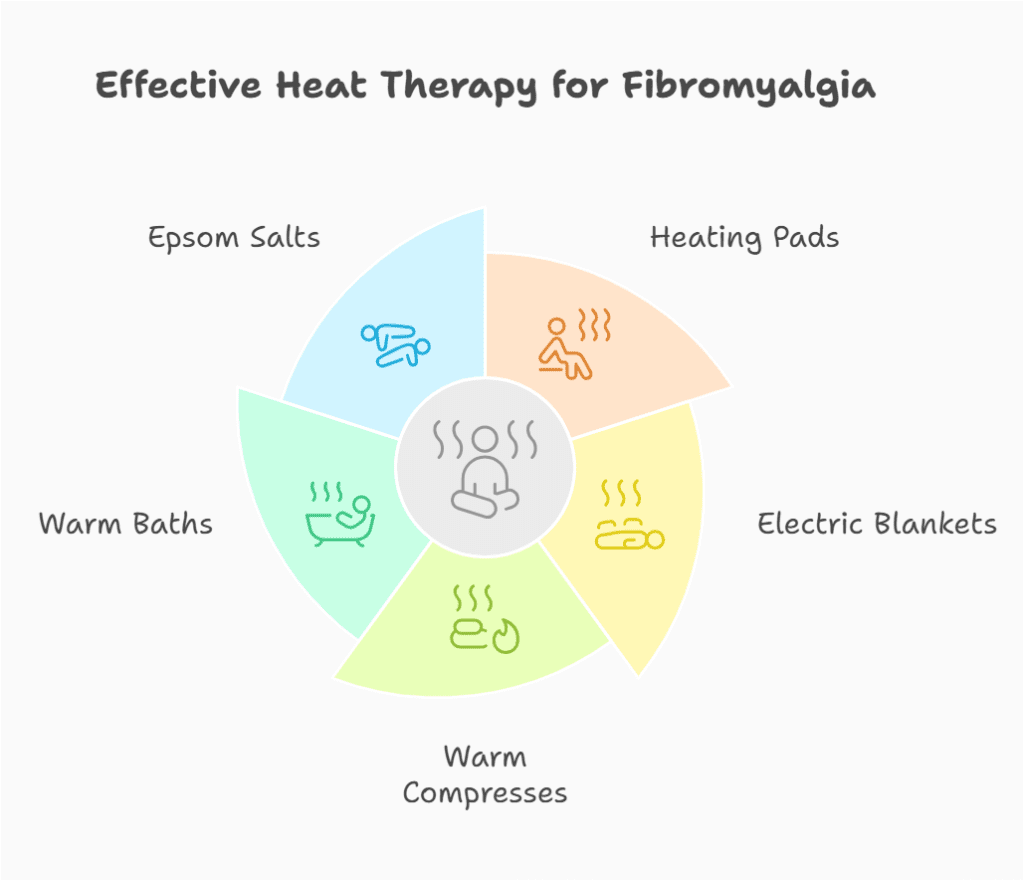
2. Use Heat Therapy
Heat therapy is one of the most effective ways to relieve fibromyalgia pain during cold weather. Applying heating pads, electric blankets, and warm compresses to sore muscles can reduce stiffness and improve circulation.
Taking warm baths or showers with Epsom salts can also relax muscles and ease joint discomfort. Heat therapy not only soothes pain but also promotes relaxation, helping to counteract stress and tension.
3. Stay Active with Gentle Exercise
While cold weather may discourage outdoor activities, staying physically active is essential for reducing stiffness, improving flexibility, and maintaining overall well-being. Low-impact exercises such as:
- Yoga
- Tai chi
- Stretching routines
- Swimming in a heated pool
- Indoor walking or cycling
These activities help prevent muscle tightness and release endorphins, which act as natural pain relievers. If possible, warming up indoors before heading outside can help minimize stiffness.
4. Maintain a Consistent Sleep Routine
Poor sleep is a common issue for individuals with fibromyalgia, and cold weather can make it even harder to rest. Establishing a consistent sleep schedule can improve sleep quality. Try:
- Using weighted blankets for warmth and comfort
- Keeping the bedroom temperature slightly warm to prevent body chills
- Avoiding blue light exposure from screens at least an hour before bedtime
- Practicing relaxation techniques like deep breathing or meditation before sleep
Good sleep hygiene can reduce fatigue and lessen fibromyalgia flare-ups.
5. Manage Stress and Mood Changes
Colder months can bring seasonal affective disorder (SAD), depression, and increased stress, which can exacerbate fibromyalgia symptoms. Managing mental well-being is just as important as physical health. Consider:
- Light therapy: Exposure to a sunlamp for 30 minutes daily can help regulate mood and energy levels.
- Meditation and mindfulness: Practicing breathing exercises can lower stress levels.
- Counseling or support groups: Talking to others who understand fibromyalgia can provide emotional relief.
6. Eat a Nutrient-Rich Diet and Stay Hydrated
Nutrition plays a key role in managing inflammation and maintaining energy levels. A balanced diet with:
- Omega-3 fatty acids (found in fish, flaxseeds, and walnuts) to reduce inflammation
- Magnesium-rich foods (spinach, almonds, bananas) to ease muscle cramps
- Vitamin D supplements if sun exposure is limited in winter months
Staying hydrated also helps prevent muscle stiffness and fatigue.
7. Plan Activities Wisely
Cold weather can make simple daily tasks more exhausting. Pacing yourself and prioritizing essential tasks can help manage energy levels. Using assistive tools like ergonomic chairs, heating pads, and voice-to-text applications can also make daily life easier.
Medications and Treatments
While lifestyle adjustments help, medications and treatments play a critical role in reducing pain, improving sleep, and enhancing quality of life for people with fibromyalgia.
| Medication Type | Purpose | Common Examples |
|---|---|---|
| Pain Relievers | Reduces inflammation and discomfort | Ibuprofen (Advil), Acetaminophen (Tylenol) |
| Nerve Pain Medications | Helps control neuropathic pain | Gabapentin (Neurontin), Pregabalin (Lyrica) |
| Antidepressants | Balances serotonin and norepinephrine | Duloxetine (Cymbalta), Amitriptyline |
| Muscle Relaxants | Relieves muscle spasms and stiffness | Cyclobenzaprine (Flexeril) |
| Sleep Aids | Improves sleep quality and reduces fatigue | Melatonin, low-dose amitriptyline |
1. Medications for Fibromyalgia
There is no single cure for fibromyalgia, but various medications help manage symptoms. Commonly prescribed options include:
A. Pain Relievers
- Over-the-counter pain relievers: Acetaminophen (Tylenol), ibuprofen (Advil), and naproxen (Aleve) can provide mild relief.
- Prescription pain medications: In some cases, duloxetine (Cymbalta) or milnacipran (Savella), which are serotonin-norepinephrine reuptake inhibitors (SNRIs), help reduce fibromyalgia-related pain.
- Anticonvulsants: Gabapentin (Neurontin) and pregabalin (Lyrica) are nerve pain medications that help with fibromyalgia symptoms.
B. Sleep Aids
Since poor sleep worsens fibromyalgia symptoms, doctors may prescribe:
- Amitriptyline or cyclobenzaprine to promote deeper sleep.
- Melatonin supplements to help regulate sleep cycles naturally.
C. Muscle Relaxants
- Cyclobenzaprine (Flexeril) is often used to reduce muscle spasms and stiffness.
D. Antidepressants
- Tricyclic antidepressants (TCAs), such as amitriptyline, can help relieve pain and improve sleep.
- Selective serotonin reuptake inhibitors (SSRIs) like fluoxetine (Prozac) may help balance brain chemicals involved in pain perception.
2. Alternative and Holistic Treatments
In addition to medications, many individuals with fibromyalgia benefit from complementary therapies, including:
- Physical Therapy: Working with a physical therapist can improve flexibility, posture, and muscle strength, helping to reduce pain and stiffness.
- Acupuncture: Acupuncture has shown promising results in reducing pain and improving overall well-being in fibromyalgia patients. It works by stimulating specific points on the body to release endorphins and improve circulation.
- Massage Therapy: Regular massage therapy can help relieve muscle tension, improve blood flow, and promote relaxation.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals reframe negative thoughts about pain and develop coping strategies to manage symptoms effectively.
3. Supplements for Fibromyalgia
Certain supplements may also provide relief for some people, including:
- Magnesium: Helps with muscle function and relaxation.
- Vitamin D: supports bone and muscle health, which is particularly important in winter.
- 5-HTP (5-Hydroxytryptophan): May help with mood regulation and pain perception.
Lifestyle Adjustments for Managing Fibromyalgia
Making lifestyle adjustments is one of the most effective ways to manage fibromyalgia symptoms, especially during colder months. Small daily changes can help reduce pain, improve energy levels, and enhance overall well-being.
1. Establish a Daily Routine
People with fibromyalgia often experience energy fluctuations, so maintaining a consistent daily routine can help manage symptoms. Setting regular times for waking up, meals, exercise, and sleep can help the body function more efficiently and reduce flare-ups.
2. Prioritize Rest and Pacing
Overexertion can worsen fatigue and pain, so it's important to listen to your body. The “pacing” technique—breaking tasks into smaller parts with rest periods—prevents exhaustion. Instead of pushing through discomfort, alternating between activity and relaxation helps maintain energy throughout the day.
3. Maintain a Fibromyalgia-Friendly Diet
Eating nutrient-dense foods can help reduce inflammation and support overall health. A balanced diet includes:
- Lean proteins (chicken, fish, tofu) for muscle health
- Anti-inflammatory foods (berries, leafy greens, nuts)
- Whole grains for sustained energy
- Omega-3 fatty acids (salmon, walnuts) to support joint and nerve health Avoiding processed foods, excessive sugar, and caffeine can help minimize symptom flare-ups.
4. Stay Hydrated
Dehydration can worsen muscle stiffness and fatigue. Drinking plenty of water throughout the day helps maintain joint and muscle function.
5. Improve Sleep Hygiene
Quality sleep is essential for managing fibromyalgia. Creating a relaxing bedtime routine, using weighted blankets, and keeping a consistent sleep schedule can improve rest and reduce fatigue.
6. Reduce Stress and Stay Positive
Managing stress is crucial. Meditation, deep breathing, light yoga, and journaling can help lower anxiety and tension, reducing the impact of fibromyalgia symptoms. Staying engaged in enjoyable activities and connecting with supportive people can also improve overall well-being.
Everything You Need to Know About Fibromyalgia
Living with fibromyalgia presents daily challenges, but understanding the condition is the first step toward effective management. We've explored various facets of fibromyalgia, from diagnosis and symptoms to treatment options and lifestyle adjustments.
Remember, you're not alone in this journey. By implementing the strategies discussed, such as maintaining a healthy lifestyle, seeking appropriate medical care, and building a strong support system, you can improve your quality of life.
About Dr. Sean Ormond