
Managing Pain in Rheumatic Conditions: Treatment Approaches and Support
Living with a rheumatic condition can be a daily challenge, as these diseases often cause chronic pain and significantly impact one's quality of life. Rheumatic conditions, such as rheumatoid arthritis, lupus, and gout, are characterized by inflammation and pain in the muscles, joints, and connective tissues.
For many individuals, managing this pain is a crucial part of maintaining their overall health and well-being. Effective pain management not only alleviates discomfort but also improves mobility and reduces the risk of long-term disability. Let's look at managing pain in rheumatic conditions.
What Are Rheumatic Conditions?
Rheumatic conditions are a diverse group of diseases that primarily affect the joints, muscles, and connective tissues. They are often characterized by pain, swelling, and stiffness, which can lead to reduced mobility and function.
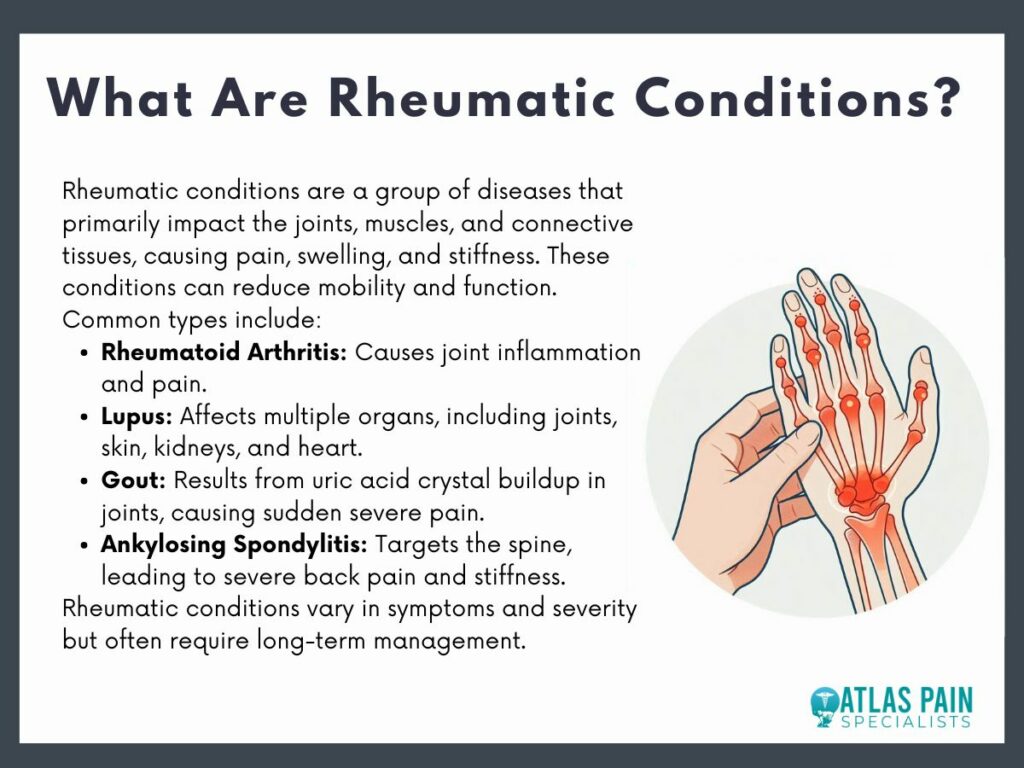
Some of the most common types of rheumatic conditions include rheumatoid arthritis, lupus, gout, and ankylosing spondylitis.
- Rheumatoid arthritis primarily affects the joints, leading to inflammation and pain.
- Lupus can affect multiple organs, including the skin, kidneys, and heart, in addition to the joints.
- Gou is caused by the buildup of uric acid crystals in the joints, leading to sudden and severe pain.
- Ankylosing spondylitis affects the spine and can cause severe back pain and stiffness.
Common Symptoms Associated with Rheumatic Conditions
The symptoms of rheumatic conditions can vary widely depending on the specific disease and its severity. However, some common symptoms include joint pain, swelling, stiffness, and decreased range of motion.
These symptoms can be persistent and may worsen over time, particularly if the condition is left untreated. In some cases, rheumatic conditions can also cause systemic symptoms such as fatigue, fever, and weight loss.
Joint pain is often the most prominent symptom, and it can range from mild to severe. Swelling and stiffness, particularly in the morning or after periods of inactivity, are also common. These symptoms can significantly impact daily activities, making it difficult to perform routine tasks.
How These Conditions Affect Pain and Mobility
Rheumatic conditions can have a profound impact on both pain and mobility. The inflammation caused by these conditions leads to joint damage, which can result in chronic pain and reduced function.
Over time, this can lead to joint deformities and loss of mobility, further affecting a person's ability to perform daily activities. Managing pain and maintaining mobility are key goals in the treatment of rheumatic conditions.
Pain in rheumatic conditions is often chronic and can be debilitating and can affect multiple joints and may fluctuate in intensity. Reduced mobility is a significant concern, as it can lead to muscle weakness and further joint damage.
Conventional Treatment Approaches
Managing rheumatic conditions often requires a multifaceted approach, combining various treatments to reduce pain, control inflammation, and improve joint function. Conventional treatments have been extensively studied and are widely used in clinical practice due to their effectiveness.
A rheumatologist, a specialist in rheumatic diseases, often leads the treatment plan, working closely with patients to monitor progress and adjust therapies as needed. The goal is to minimize symptoms, prevent joint damage, and improve the overall quality of life.
1. Medications
Medications play a central role in the management of rheumatic conditions, helping to control pain and reduce inflammation. There are several categories of medications commonly used, each with its own mechanism of action and indications.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) are often the first line of treatment, providing relief from pain and inflammation. These drugs can be over-the-counter, like ibuprofen or prescription-strength.
- Disease-Modifying Antirheumatic Drugs (DMARDs) are another critical category, particularly for conditions like rheumatoid arthritis. DMARDs work by slowing the progression of the disease and preventing joint damage.
- Methotrexate is a commonly prescribed DMARD that has been shown to be effective in many patients.
- Biologics, a newer class of DMARDs, target specific components of the immune system and are often used when traditional DMARDs are insufficient.
- Corticosteroids, such as prednisone, are powerful anti-inflammatory agents used for short-term relief of severe symptoms.
2. Physical Therapy
Physical therapy is an essential component of managing rheumatic conditions, focusing on improving mobility, strength, and function. A physical therapist designs a personalized exercise program that helps maintain joint flexibility and muscle strength.
Exercises commonly recommended include range-of-motion exercises, strengthening exercises, and low-impact aerobic activities.
- Range-of-motion exercises help keep the joints flexible while strengthening exercises build muscle strength to support the joints.
- Low-impact aerobic activities, such as swimming or walking, improve overall cardiovascular health without putting undue stress on the joints.
- Physical therapists teach patients how to use assistive devices and provide techniques to protect the joints during daily activities.
3. Surgical Options
In some cases, when medication and physical therapy are not enough to control symptoms or prevent joint damage, surgical interventions may be necessary. Surgery can help restore function, relieve pain, and improve the quality of life for individuals with severe rheumatic conditions.
Common surgical procedures include:
- Joint replacement: damaged joints are replaced with artificial ones, and joint fusion involves permanently joining two or more bones to stabilize and reduce pain.
- Arthroscopy: minimally invasive surgery that allows doctors to diagnose and treat joint problems using a small camera and specialized instruments.
These surgical options can be highly effective in managing severe cases, although they come with risks and require a recovery period.
Complementary and Alternative Therapies
While some of these treatments have a strong evidence base, others are still being studied for their efficacy and safety. Complementary and alternative therapies encompass a wide range of practices and products that can help manage pain, reduce inflammation, and promote relaxation and stress relief.
1. Acupuncture
Acupuncture is a traditional Chinese medicine practice that involves inserting thin needles into specific points on the body to balance energy flow and alleviate pain. It has gained popularity as a complementary therapy for managing pain associated with rheumatic conditions.
Research suggests that acupuncture can help reduce pain, improve joint function, and enhance overall well-being. The exact mechanism by which acupuncture works is not fully understood, but it is believed to stimulate the nervous system, release endorphins (natural painkillers), and improve blood flow.
Many patients report significant pain relief and increased mobility after acupuncture sessions. It is generally considered safe when performed by a trained practitioner, although potential risks include minor bruising or soreness at the needle insertion sites.
2. Chiropractic Care
Chiropractic care focuses on diagnosing and treating musculoskeletal disorders, particularly those affecting the spine. Chiropractors use manual manipulation and other techniques to improve alignment, reduce pain, and enhance physical function.
For individuals with rheumatic conditions, chiropractic care can help manage pain and improve mobility, particularly in the spine and other affected joints. Chiropractic treatments often involve spinal adjustments, soft tissue therapies, and exercises tailored to the patient's needs.
These treatments can help reduce pain, increase range of motion, and improve overall joint function. However, it is important for patients with rheumatic conditions to choose a chiropractor experienced in treating their specific condition and to discuss their treatment plan with their healthcare provider to avoid potential complications.
3. Herbal Supplements and Diet
Herbal supplements and dietary modifications are commonly used as complementary approaches to managing rheumatic conditions. Certain herbs and nutrients have anti-inflammatory properties that can help reduce pain and inflammation.
Popular supplements include turmeric, ginger, omega-3 fatty acids, and glucosamine. An anti-inflammatory diet, rich in fruits, vegetables, whole grains, and lean proteins, can also play a role in managing symptoms.
Such a diet emphasizes foods that reduce inflammation and excludes those that can exacerbate it, such as processed foods, sugary snacks, and red meat.
4. Massage Therapy
Massage therapy involves the manipulation of soft tissues to reduce pain, improve circulation, and promote relaxation. It can be particularly beneficial for individuals with rheumatic conditions, as it helps alleviate muscle tension, reduce stress, and enhance overall well-being.
Different types of massage, such as Swedish, deep tissue, and trigger point therapy, can be tailored to address specific needs and preferences. Regular massage sessions can improve joint flexibility, reduce pain and stiffness, and enhance mental and emotional well-being.
Lifestyle and Self-Management Strategies
Managing rheumatic conditions effectively often involves incorporating lifestyle and self-management strategies to complement medical treatments. Lifestyle and self-management strategies are tailored to each individual's unique needs and preferences.

1. Importance of Regular Exercise
Regular exercise is a cornerstone of managing rheumatic conditions, as it helps maintain joint flexibility, muscle strength, and overall physical fitness. Exercise can significantly reduce pain, improve mobility, and enhance the quality of life for individuals with rheumatic conditions.
Low-impact aerobic activities, such as swimming, walking, and cycling, are excellent options for maintaining cardiovascular health without putting excessive stress on the joints. Strength training exercises help build muscle strength, which supports the joints and reduces the risk of injury.
Flexibility exercises, such as yoga and stretching, improve joint range of motion and reduce stiffness.
2 . Stress Management Techniques
Managing stress is crucial for individuals with rheumatic conditions, as stress can exacerbate symptoms and negatively impact overall health. Stress management techniques, such as mindfulness and meditation, can help reduce stress levels and improve mental and emotional well-being.
Cognitive-behavioral therapy (CBT) is another effective stress management technique that helps individuals develop coping strategies and change negative thought patterns. CBT can improve pain management and enhance quality of life by addressing the psychological aspects of living with a chronic condition.
Other stress management practices, such as deep breathing exercises, progressive muscle relaxation, and engaging in enjoyable activities, can also help reduce stress and improve overall well-being.
3. Sleep Hygiene
Good sleep hygiene is essential for individuals with rheumatic conditions, as poor sleep can worsen pain and fatigue. Establishing healthy sleep habits can help improve sleep quality and overall health.
Creating a consistent sleep schedule, going to bed, and waking up at the same time each day helps regulate the body's internal clock and promotes better sleep. Ensuring a comfortable sleep environment, free from distractions and conducive to restful sleep, is also important.
Limiting caffeine and alcohol intake, particularly in the evening, and avoiding stimulating activities before bedtime can further improve sleep quality.
4. Nutrition and Healthy Eating
A balanced diet plays a crucial role in managing rheumatic conditions. Eating a variety of nutrient-rich foods helps reduce inflammation, maintain a healthy weight, and improve overall health.
- An anti-inflammatory diet, rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, can help manage symptoms and improve quality of life.
- Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, have anti-inflammatory properties and can help reduce joint pain and stiffness.
- Antioxidant-rich foods, such as berries, leafy greens, and nuts, help protect the body from oxidative stress and inflammation.
- Avoiding processed foods, sugary snacks, and excessive red meat can further reduce inflammation and support overall health.
Non-Pharmacological Pain Management Techniques
Managing pain in rheumatic conditions requires a comprehensive and multifaceted approach that includes both conventional and complementary treatments. Non-pharmacological pain management techniques are particularly relevant in the context of rheumatic conditions.
These techniques, which include lifestyle changes, self-management strategies, and complementary therapies, offer valuable tools for managing pain without relying solely on medications. Incorporating these approaches can help reduce the need for pharmaceuticals, minimize side effects, and provide additional avenues for pain relief and improved well-being.
These non-pharmacological techniques are essential for addressing the multifaceted nature of rheumatic pain. They provide practical, everyday strategies that individuals can use to manage their symptoms and enhance their overall health.
About Dr. Sean Ormond