Understanding The Complex Regional Pain Syndrome (CRPS)
A small but considerable segment of the population suffers from the confusing and sometimes misdiagnosed chronic pain disease known as Complex Regional Pain Syndrome (CRPS). It typically manifests as severe, prolonged pain in one or more limbs, accompanied by sensory, motor, and autonomic abnormalities.
Despite its relatively low prevalence, CRPS can have profound and far-reaching effects on the physical, emotional, and social well-being of those afflicted, often leading to disability, reduced quality of life, and significant healthcare costs. Understanding CRPS is essential for healthcare professionals, patients, caregivers, and the broader community.
The condition's complex nature, varied presentations, and lack of definitive diagnostic tests pose challenges to accurate diagnosis and effective management. Moreover, the unpredictable course of CRPS and its potential to worsen over time underscore the need for comprehensive, multidisciplinary approaches to treatment and care.
What is CRPS?
Complex Regional Pain Syndrome (CRPS) is a multifaceted chronic pain condition that presents with a wide array of symptoms, often affecting one or more extremities. This condition is characterized by disproportionate and continuous pain that is typically more severe than expected based on the initial injury or inciting event.
CRPS is often divided into two subtypes, each with its own distinct characteristics and diagnostic criteria, which we will explore in detail.
1. CRPS Type I (formerly known as Reflex Sympathetic Dystrophy, RSD)
CRPS Type I is the most common form of the condition, accounting for approximately 90% of cases. It typically occurs following an injury or trauma, such as a fracture, sprain, or surgical procedure, although the severity of the initial injury may not correlate with the intensity of the subsequent pain.
This subtype of CRPS is characterized by the absence of detectable nerve damage or injury on diagnostic tests, making its diagnosis primarily based on clinical findings. Despite the lack of identifiable nerve damage, CRPS Type I is associated with dysregulation of the ANS (autonomic nervous system), leading to symptoms such as changes in skin color, temperature, texture, and abnormal sweating and swelling.
Additionally, individuals with CRPS Type I may experience sensory disturbances, including hyperalgesia (increased sensitivity to pain), allodynia (pain in response to non-painful stimuli), motor dysfunction, and muscle weakness in the affected limb.
2. CRPS Type II (formerly known as causalgia)
CRPS Type II, also referred to as causalgia, differs from Type I in that it is characterized by identifiable nerve damage or injury. This subtype typically occurs following a nerve injury, such as laceration, crush injury, or nerve entrapment, and is often associated with more severe and persistent pain compared to Type I.
Despite the presence of nerve damage, the pain experienced in CRPS Type II may still be disproportionate to the extent of the initial injury. In addition to the hallmark features of CRPS, individuals with Type II may exhibit signs of nerve injury, such as sensory loss, weakness, and abnormal nerve conduction studies.
The presence of demonstrable nerve damage in CRPS Type II underscores the involvement of both peripheral and central nervous system mechanisms in the pathophysiology of the condition.
Who Does CRPS Affect?
Complex Regional Pain Syndrome (CRPS) can affect individuals of any age, gender, or ethnicity, although certain demographic and clinical factors may influence the likelihood of developing the condition.
A risk factor is an attribute or pattern of behavior that is more common in people with an illness or in people who are more likely to have a disease than in those without risk factor. A person does not automatically develop a condition because they do not have a risk factor, and vice versa.
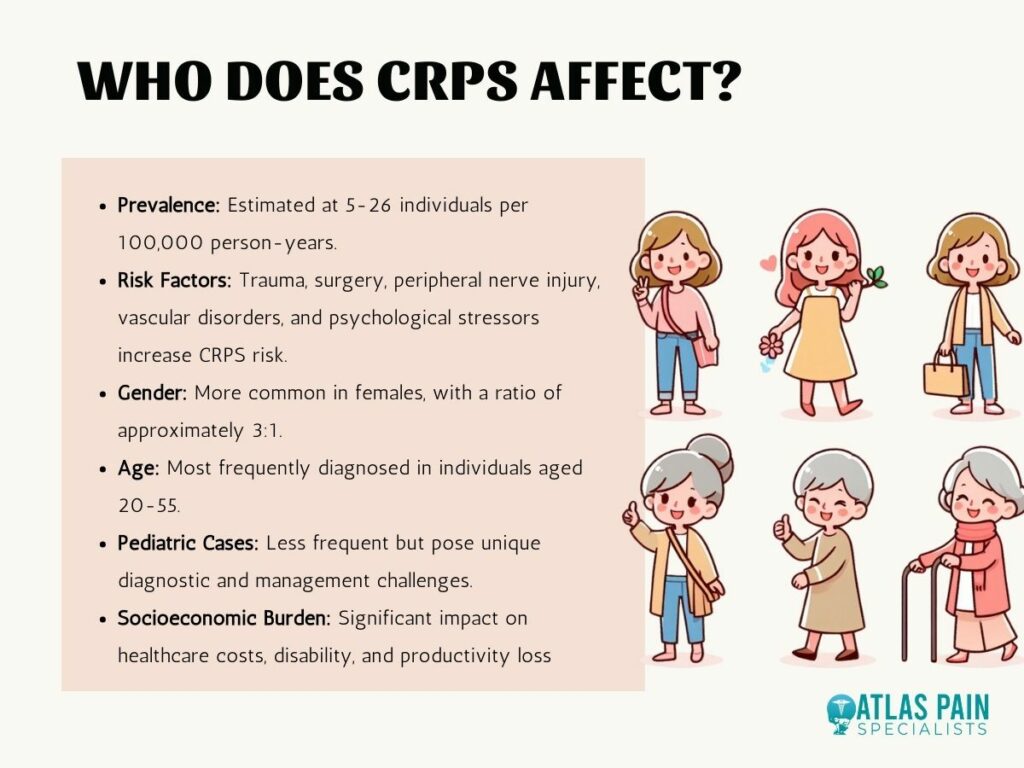
1. Demographics of CRPS
CRPS affects both genders, although it is more commonly observed in females than males, with some studies suggesting a female-to-male ratio of approximately 3:1. The condition can occur at any age. Still, it is most frequently diagnosed in individuals between 20 and 55.
However, CRPS can also affect children and adolescents, albeit less frequently, presenting unique challenges in diagnosis and management in pediatric populations.
2. Prevalence and Incidence
The exact prevalence and incidence of CRPS are difficult to ascertain due to variations in diagnostic criteria, healthcare utilization patterns, and underreporting of cases. However, estimates suggest that CRPS affects anywhere from 5 to 26 individuals per 100,000 person-years, with higher rates reported in certain populations, such as those with prior trauma or surgery.
Despite its relatively low prevalence, CRPS can have a significant socioeconomic burden, with implications for healthcare costs, disability, and loss of productivity.
3. Risk Factors for CRPS
Although the exact etiology of CRPS is still unknown, several risk factors have been found to raise the chance of developing the condition. Trauma or injury, such as fractures, sprains, or surgical procedures, is a well-established trigger for CRPS, particularly in cases of CRPS Type I.
Other predisposing factors include peripheral nerve injury, vascular disorders, and psychological stressors, although the exact mechanisms by which these factors contribute to the development of CRPS are not fully understood. Additionally, certain genetic predispositions and susceptibility factors may influence an individual's risk of developing CRPS, highlighting the complex interplay between genetic, environmental, and psychosocial factors in the pathogenesis of the condition.
Symptoms of CRPS
Complex Regional Pain Syndrome (CRPS) is characterized by a diverse array of symptoms that can vary in severity and presentation among affected individuals. The quality of life and outcomes for patients with this difficult chronic pain syndrome can be enhanced by healthcare teams by treating the complex and complex nature of CRPS symptoms with a thorough and multidisciplinary approach.
It is important to note that the symptoms of CRPS can vary widely among individuals and may change over time. Some individuals may experience fluctuations in symptom severity, while others may develop progressive worsening of symptoms. Additionally, the presentation of CRPS may differ depending on the subtype (Type I or Type II) and other factors such as age, comorbidities, and response to treatment.

1. Chronic Pain
Chronic, persistent pain is the hallmark symptom of CRPS, often described as burning, throbbing, or shooting in nature. The pain is typically localized to the affected limb but may spread to adjacent areas over time.
Individuals with CRPS often report that the pain is disproportionate to the inciting event or injury and may worsen with movement or touch.
2. Sensory Disturbances
CRPS can cause a range of sensory abnormalities, including hyperalgesia, which is an increased sensitivity to painful stimuli, and allodynia, which is a pain in response to normally non-painful stimuli, such as light touch or gentle pressure.
Other sensory disturbances may include tingling, numbness, or a feeling of pins and needles in the affected limb.
3. Motor Dysfunction
Motor dysfunction is common in CRPS and may manifest as weakness, tremors, or involuntary muscle contractions (dystonia). Individuals with CRPS may experience difficulty moving the affected limb, as well as limitations in coordination and fine motor skills.
Muscle atrophy and weakness may occur due to disuse or immobilization of the limb secondary to pain. Simple tasks such as dressing, grooming, and household chores may become challenging or impossible, leading to dependency on caregivers and reduced independence.
4. Autonomic Symptoms
Dysregulation of the autonomic nervous system is a hallmark feature of CRPS and can manifest in various ways. Changes in skin temperature, color, and texture are commonly observed, with the affected limb appearing either warmer or cooler than the unaffected limb.
Additionally, individuals with CRPS may experience abnormal sweating (either excessive sweating or absence of sweating) and swelling (edema) in the affected limb.x
Causes and Triggers of CRPS
Complex Regional Pain Syndrome (CRPS) can be triggered by a variety of factors, ranging from traumatic injuries to medical procedures. It is important to recognize that not all individuals who experience trauma or injury will develop CRPS, highlighting the role of individual susceptibility factors in the pathogenesis of the condition.
1. Traumatic Injuries
Trauma or injury is one of the most common triggers for CRPS, particularly in cases of CRPS Type I. Fractures, sprains, contusions, and surgical procedures can all precipitate the onset of CRPS, although the severity of the initial injury may not always correlate with the subsequent development or severity of symptoms.
The exact mechanisms by which trauma leads to CRPS are not fully understood but may involve neurogenic inflammation, peripheral sensitization, and dysregulation of the sympathetic nervous system.
2. Surgical Procedures
Surgeries, particularly those involving orthopedic or peripheral nerve procedures, carry a risk of triggering CRPS, either as a complication of the surgery itself or as a result of postoperative pain and inflammation.
CRPS can develop following relatively minor surgical interventions, such as carpal tunnel release or arthroscopic procedures, highlighting the importance of vigilant monitoring and early intervention in high-risk individuals.
3. Peripheral Nerve Injury
Injuries to peripheral nerves, either from trauma or compression, can predispose individuals to developing CRPS, particularly in cases of CRPS Type II. Nerve injuries disrupt normal nerve signaling and can lead to aberrant pain processing, sensory disturbances, and motor dysfunction characteristic of CRPS.
Identifying and addressing nerve injuries promptly through surgical decompression or neurolysis may help prevent or mitigate the development of CRPS in susceptible individuals.
4. Vascular Disorders
Vascular abnormalities, such as vasospasm, ischemia-reperfusion injury, and endothelial dysfunction, have been implicated as potential triggers for CRPS. Changes in blood flow and microcirculation observed in CRPS may result from sympathetic nervous system dysregulation, leading to tissue hypoxia, inflammation, and neuropathic pain.
Individuals with pre-existing vascular conditions, such as Raynaud's phenomenon or peripheral vascular disease, may be at increased risk for developing CRPS following vascular insults or procedures.
Diagnosis and Treatment
Accurate diagnosis and effective treatment of Complex Regional Pain Syndrome (CRPS) require a multidisciplinary approach that addresses the complex interplay of neurologic, inflammatory, and psychosocial factors underlying the condition. Timely recognition of CRPS and prompt initiation of appropriate interventions are essential for improving outcomes and quality of life for affected individuals.
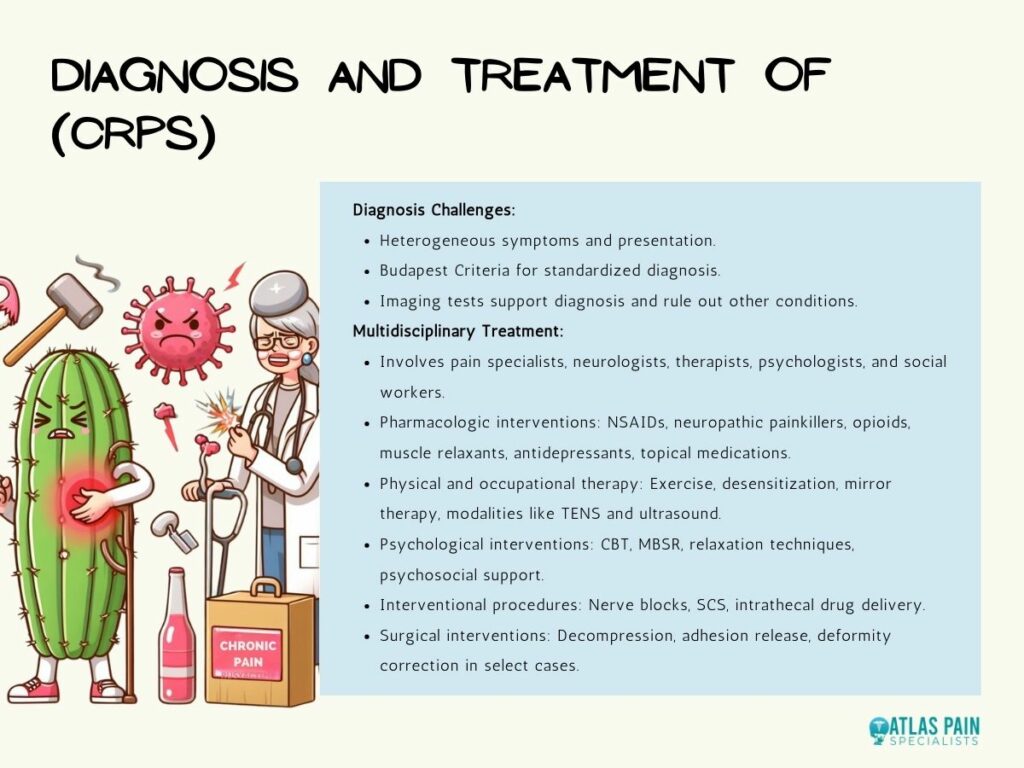
1. Challenges in Diagnosis
Diagnosing CRPS can be challenging due to the heterogeneity of symptoms, variability in presentation, and lack of definitive diagnostic tests. The Budapest Criteria, established by the International Association for the Study of Pain (IASP), provides a standardized framework for diagnosing CRPS based on clinical signs and symptoms, including pain, sensory disturbances, motor dysfunction, and autonomic changes.
Although results from imaging tests, such as MRIs, bone scans, and X-rays, are frequently nonspecific, they can be used to support the diagnosis of CRPS and rule out other illnesses.
2. Multidisciplinary Treatment Approaches
The management of CRPS typically involves a multidisciplinary team of healthcare professionals, including pain specialists, neurologists, physical therapists, occupational therapists, psychologists, and social workers. Treatment approaches for CRPS are aimed at addressing pain, improving function, and enhancing quality of life through a combination of pharmacologic, physical, psychological, and interventional modalities.
- Pharmacologic Interventions: Pharmacologic therapies for CRPS aim to relieve pain, reduce inflammation, and improve function. Nonsteroidal anti-inflammatory drugs (NSAIDs), neuropathic painkillers (pregabalin, gabapentin, etc.), opioid analgesics, muscle relaxants, and antidepressants are among the most often utilized pharmaceuticals. Topical medications like capsaicin cream or lidocaine patches may also relieve regional pain.
- Physical and Occupational Therapy: Physical and occupational therapy play a critical role in managing CRPS by addressing motor dysfunction, restoring function, and promoting independence. Therapeutic interventions may include gentle exercise, stretching, desensitization techniques, mirror therapy, and graded motor imagery. Modalities such as transcutaneous electrical nerve stimulation (TENS), ultrasound, and hydrotherapy may also be used to alleviate pain and improve mobility.
- Psychological Interventions: Psychological interventions, such as cognitive-behavioral therapy (CBT), mindfulness-based stress reduction (MBSR), and relaxation techniques, can help individuals with CRPS cope with pain, manage stress, and improve psychological well-being. Psychosocial support, education, and counseling are essential components of comprehensive CRPS management and may address underlying emotional distress, maladaptive coping strategies, and social isolation.
- Interventional Procedures: Interventional procedures, such as nerve blocks, sympathetic ganglion blocks, intrathecal drug delivery, and spinal cord stimulation (SCS), may be considered for individuals with refractory CRPS who have not responded to conservative therapies. These minimally invasive procedures aim to modulate pain signals, interrupt sympathetic nervous system activity, and improve function.
- Surgical Interventions: In select cases of CRPS with significant nerve compression or structural abnormalities, surgical interventions may be considered to decompress nerves, release adhesions, or correct deformities. Surgical procedures should be approached cautiously and reserved for individuals who have failed conservative treatments and have identifiable anatomical lesions amenable to surgical correction.
New Treatment for CRPS
Ongoing research into the pathophysiology of CRPS and the development of novel treatment modalities hold promise for improving outcomes and expanding therapeutic options for affected individuals. Participating in clinical trials and staying informed about advances in CRPS research may offer new hope for individuals living with this challenging condition.
Read on on New Treatment for CPRS to find out more about emerging therapies. These include monoclonal antibodies targeting inflammatory cytokines, gene therapy, regenerative medicine approaches, and neuromodulation techniques, which are being investigated in preclinical and clinical studies.
A comprehensive and cooperative approach that tackles the wide range of symptoms and underlying mechanisms causing the condition is necessary for the comprehensive management of CRPS. Through the integration of customized care plans, evidence-based treatments, and continuous support, medical professionals can improve patient outcomes and quality of life for those with CRPS.
About Dr. Sean Ormond