
Five Things You Didn't Know About Nerve Burning For Back Pain
Back pain is one of the most common complaints in the United States, affecting millions of adults each year. It disrupts sleep, limits work, and changes how people go about everyday life. While physical therapy, medications, and exercise often help, many people find that these measures only go so far. For those who live with persistent discomfort, a treatment called radiofrequency ablation—often nicknamed “nerve burning” sometimes enters the conversation. The name alone can be enough to spark anxiety, yet the reality of the procedure is different than most imagine. Nerve burning is not a destructive act but a carefully planned therapy designed to reduce pain signals and improve daily function.
Below are five things most people do not know about this treatment, explained in detail to show where it fits into modern back pain care.
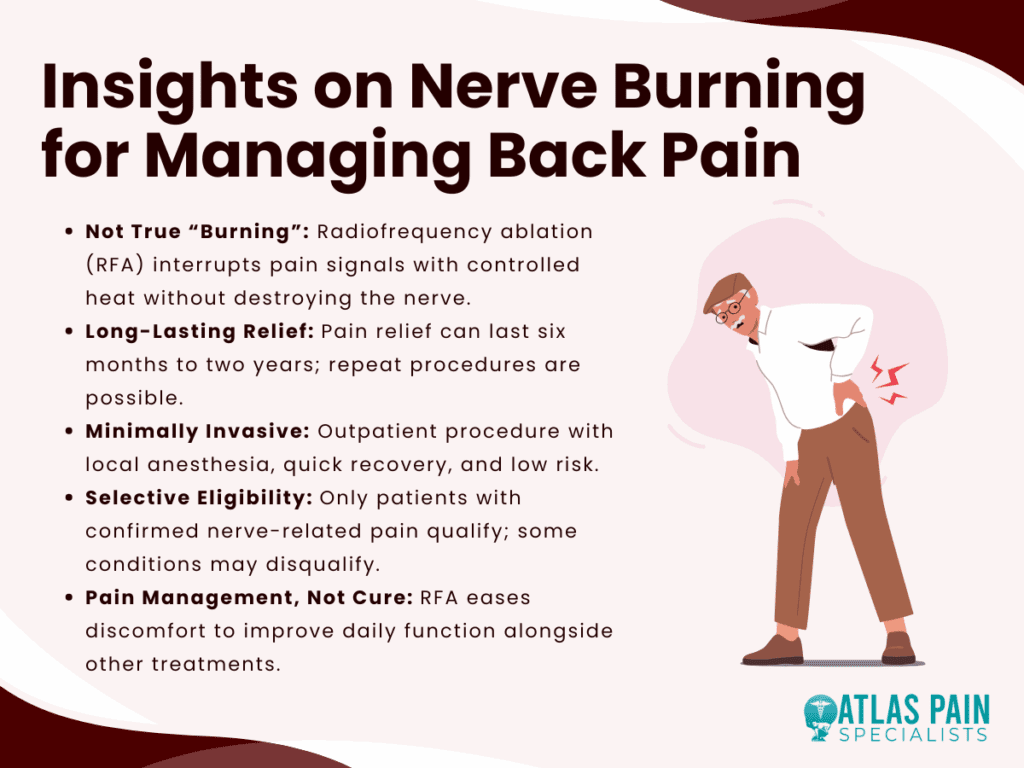
1. It’s Not Actually “Burning” in the Way You Think
The name “nerve burning” paints a dramatic picture, but the truth is far more refined. The medical term for the procedure is radiofrequency ablation, or RFA. During the treatment, a doctor inserts a thin probe through the skin to reach the nerve suspected of carrying pain signals. Imaging technology like fluoroscopy is used to ensure accurate placement. Once in position, radio waves generate heat at the tip of the probe, interrupting the nerve’s ability to transmit pain.
What happens is not the fiery destruction of tissue but a controlled interference in communication between the nerve and the brain. This interference reduces the sensation of pain without eliminating the nerve completely. Over time, the nerve often regenerates, which is why the procedure can be repeated when needed.
Precision Targeting of Nerves
A fascinating detail is the precision behind the therapy. Doctors use test stimulations before applying radiofrequency, ensuring the correct nerves are targeted. This method spares surrounding muscles and tissue from unnecessary damage. Compared with surgery, which physically alters structure-
s of the spine, this targeted approach is gentler, reversible, and far less risky.
A Misunderstood Name
The term “burning” has stuck partly because of the heat involved, but it has led to misunderstandings. Many patients initially fear the idea of scorched nerves, only to be surprised when their physician explains the subtlety of the treatment. Understanding this distinction helps patients approach the procedure with more confidence and less apprehension.
2. Relief Can Last Longer Than You’d Expect
Some people assume nerve burning only offers a short-term reprieve, similar to an injection that wears off quickly. In reality, the results often last far longer. On average, pain relief ranges from six months to two years. This wide window reflects differences in health, age, the underlying condition, and lifestyle habits.
Radiofrequency ablation acts as a middle ground between quick fixes like steroid shots and major steps like surgery. It gives patients time to regain control of their lives without committing to the permanent changes and risks of invasive operations.
Why Relief Varies
The longevity of relief depends on how quickly the nerve regenerates. In some individuals, regrowth may occur sooner, while in others, the benefits last years. Factors such as arthritis severity, physical activity, and weight can also play roles. For example, someone with advanced degenerative disc disease may find that relief lasts closer to the shorter end of the spectrum, while someone with localized facet joint pain may enjoy longer results.
The Value of Repeat Procedures
Another underappreciated advantage is the ability to repeat the procedure. Once a patient responds well the first time, doctors are usually confident about offering another session when pain returns. This creates a cycle of relief that can be maintained over the years, reducing reliance on heavy medications or more invasive treatments.
3. It’s Minimally Invasive with a Quick Recovery
For people already tired of constant pain, the last thing they want is a long hospital stay or a difficult recovery. Radiofrequency ablation avoids this problem entirely. The procedure is performed in an outpatient setting and usually takes less than an hour. Patients receive local anesthesia and sometimes mild sedation but rarely require general anesthesia.
Recovery is quick, with most people returning to their usual activities within a few days. Some even go back to work the next day, depending on their comfort level. This ease surprises many who expected weeks of downtime.
Comparing Recovery with Surgery
When compared with spinal surgery, the difference is stark. Back operations often require weeks or months of rehabilitation, with risks such as infection, scarring, or long-term stiffness. By contrast, RFA leaves only a small puncture at the site of needle insertion. Discomfort afterward is usually mild soreness, which resolves quickly.
Risks and Safety Considerations
Every medical procedure carries risks, but RFA’s are relatively low. Infection and bleeding are rare, and serious complications like permanent nerve damage are uncommon. Most patients find the risks acceptable given the potential rewards, especially when compared with the side effects of long-term pain medications.
4. Not Everyone Qualifies for the Procedure
Despite its benefits, nerve burning is not offered to every patient with back pain. Physicians must first confirm that the pain originates from the nerves RFA is designed to target. To do this, they use a test called a diagnostic nerve block. A small amount of anesthetic is injected near the suspected nerve. If pain decreases significantly for the duration of the anesthetic’s effect, it suggests that RFA would be helpful.
This step ensures that only patients with nerve-related pain undergo the procedure, improving success rates and preventing unnecessary interventions.
Who May Not Qualify
Certain groups may not be good candidates. People with bleeding disorders or active infections are usually advised against the procedure. Those with pacemakers or other implantable devices may need special precautions. Additionally, patients whose pain stems mainly from muscle strain, herniated discs, or systemic illness may not benefit.
The Importance of Specialist Evaluation
Because back pain can have many sources, a thorough evaluation is vital. Pain specialists, interventional radiologists, or anesthesiologists trained in this therapy are best equipped to determine eligibility. Their expertise helps ensure that the right patients receive the right treatment.
5. It Doesn’t Cure Back Pain but Manages It Effectively
One of the biggest misconceptions about nerve burning is that it offers a permanent cure. While the relief can be dramatic, it does not stop the underlying condition that caused the pain in the first place. Arthritis, disc degeneration, and spinal stenosis remain even after nerves are quieted.
What RFA does is buy patients the freedom to live more comfortably while addressing their condition through other means. This makes it a powerful tool in a comprehensive plan rather than a standalone solution.
Combining RFA with Other Therapies
For many patients, the procedure creates an opportunity to re-engage in physical therapy or exercise programs that were impossible when pain was overwhelming. Improved movement allows for muscle strengthening, weight management, and healthier posture. These changes support long-term back health and can extend the benefits of the procedure.
Quality of Life Matters
Even when pain eventually returns, many people report that the months or years of relief transformed their lives. Being able to sleep without constant discomfort, walk without frequent stops, or work with fewer limitations are meaningful improvements that restore independence and well-being. In this sense, the measure of success is not a cure but a life lived more fully.
Comparing Nerve Burning to Other Back Pain Treatments
When looking at the landscape of back pain treatment, it becomes clear where radiofrequency ablation fits. It is more effective and longer-lasting than steroid injections, less invasive than surgery, and more immediate than physical therapy.
| Treatment | Invasiveness | Recovery Time | Duration of Relief | Ideal Use |
| Radiofrequency Ablation | Minimally invasive | A few days | 6 months to 2 years | Chronic nerve-related pain |
| Steroid Injections | Minimally invasive | 1–2 days | Weeks to months | Pain linked to inflammation |
| Physical Therapy | Non-invasive | Ongoing | Long-term with consistency | Mobility and strength building |
| Surgery | Highly invasive | Weeks to months | Potentially permanent but higher risks | Severe structural conditions |
| Medications | Non-invasive | None | Hours to days | Temporary symptom relief |
The table highlights how nerve burning balances effectiveness with safety. It does not replace other therapies but holds a distinct place as a middle-ground option for patients who need more than conservative care but want to avoid the risks of surgery.
Conclusion
Chronic back pain affects far more than the spine; it reshapes daily routines, limits independence, and erodes quality of life. Radiofrequency ablation, often misunderstood as a destructive treatment, offers a safe and precise way to reduce pain without major surgery. By quieting pain signals, it gives patients the breathing room to rebuild strength, reclaim mobility, and enjoy meaningful relief that lasts months or even years.
Although not everyone qualifies and it is not a cure, nerve burning stands as an important option within the spectrum of back pain management. Understanding its true nature helps patients and families make informed choices, moving from fear of the term “burning” to appreciation of its role in improving lives.
About Dr. Sean Ormond