
Understanding Irritable Bowel Syndrome (IBS) and Abdominal Pain
Understanding Irritable Bowel Syndrome (IBS) and abdominal pain, IBS is a common yet often misunderstood condition affecting millions globally Characterized predominantly by abdominal pain and irregular bowel habits, IBS can significantly impact daily life. But what underpins this disorder, and why is abdominal discomfort so central to its diagnosis?
In this article, we'll delve deep into the intricacies of IBS, demystifying the condition and shedding light on the complex relationship between IBS and abdominal pain. Whether you're a patient seeking clarity or simply curious, journey with us as we navigate the nuances of this prevalent yet often misunderstood disorder.
Etiology: What Causes Irritable Bowel Syndrome (IBS)?
The etiology, or cause, of Irritable Bowel Syndrome (IBS) is multifaceted and not fully understood. However, several factors have been identified that may contribute to developing or exacerbating IBS.
Here's a more detailed look into these factors:
Brain-Gut Interaction
The gut and brain are intricately connected through the gut-brain axis, a bidirectional communication system. Disturbances in this axis may lead to the symptoms of IBS. For some patients, the gut can be hypersensitive to changes that would not cause symptoms in others.
Gut Motility Issues
The movement of the muscles in the intestines (motility) can be affected by IBS. Overactive intestinal contractions can lead to diarrhea, whereas slow movement can lead to constipation.
Intestinal Inflammation
Some IBS patients show increased immune cells in their intestines, suggesting mild inflammation. This inflammation might be linked to pain and diarrhea.
Bacterial Imbalance (Dysbiosis)
The gut houses trillions of bacteria, collectively known as the microbiota. An imbalance or change in the composition of this microbiota, termed dysbiosis, is thought to be associated with IBS in some patients. This imbalance can lead to symptoms like gas, bloating, and changes in bowel habits.
Infections
There's a type of IBS known as post-infectious IBS. Some people develop IBS symptoms after suffering from a severe bout of gastroenteritis, often caused by bacteria or viruses. This suggests that the infection might trigger a lasting inflammatory response in the gut.
Food Intolerance
Although IBS is not the same as a food allergy, certain foods or ingredients can exacerbate symptoms in some individuals. Some common culprits include foods high in FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols). These are specific types of carbohydrates that some people find hard to digest.
Mental Health Factors
There's a well-documented link between mental health and IBS. Stress, anxiety, and depression can exacerbate IBS symptoms. Conversely, the chronic nature of IBS can also contribute to psychological distress.
Genetics
Some studies suggest IBS might run in families, indicating a potential genetic predisposition. However, the specific genes involved are not yet clearly identified.
Hormones
Some women find that their IBS symptoms are more pronounced around their menstrual periods, suggesting hormonal changes might play a role in IBS.
Gut Permeability
Sometimes referred to as "leaky gut," increased gut permeability means that the barrier function of the intestines might be compromised, allowing substances to pass from the gut into the bloodstream that typically wouldn't. This can lead to an immune response and symptoms of IBS.
Previous Medical Procedures
Rarely procedures like surgeries can affect the gut flora or the structure of the intestines, potentially leading to IBS.
It's worth noting that while we have made strides in understanding IBS, the exact cause may vary from person to person, and in many cases, it's likely that multiple factors combine to lead to the condition.
Abdominal Pain and Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder characterized by chronic abdominal pain and altered bowel habits without any evident structural abnormalities. Abdominal pain, a defining symptom of IBS, is often closely associated with bowel movements and is one of the primary reasons patients seek medical care.
Here's a closer look at the connection:
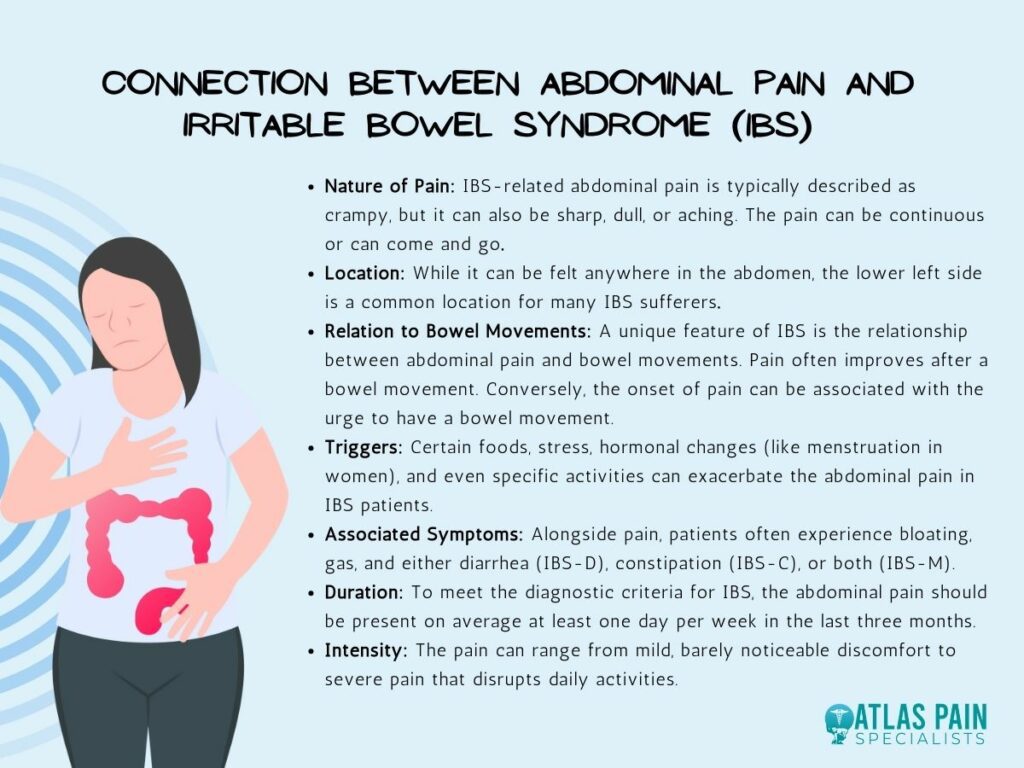
- Nature of Pain: IBS-related abdominal pain is typically described as crampy, but it can also be sharp, dull, or aching. The pain can be continuous or can come and go.
- Location: While it can be felt anywhere in the abdomen, the lower left side is a common location for many IBS sufferers.
- Relation to Bowel Movements: A unique feature of IBS is the relationship between abdominal pain and bowel movements. Pain often improves after a bowel movement. Conversely, the onset of pain can be associated with the urge to have a bowel movement.
- Triggers: Certain foods, stress, hormonal changes (like menstruation in women), and even specific activities can exacerbate the abdominal pain in IBS patients.
- Associated Symptoms: Alongside pain, patients often experience bloating, gas, and either diarrhea (IBS-D), constipation (IBS-C), or both (IBS-M).
- Duration: To meet the diagnostic criteria for IBS, the abdominal pain should be present on average at least one day per week in the last three months.
- Intensity: The pain can range from mild, barely noticeable discomfort to severe pain that disrupts daily activities.
While abdominal pain in IBS can be distressing and disrupt daily life, understanding its nature and triggers can help manage and reduce its impact. It's essential for patients to work closely with healthcare providers to tailor a treatment approach that addresses their specific symptoms.
Diagnosing Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder, meaning it's characterized by symptoms without visible structural abnormalities in the gut. Given its functional nature, diagnosing IBS can be challenging.
Here's a step-by-step approach to the diagnosis:
- Clinical Presentation: IBS presents with abdominal pain, altered bowel habits (diarrhea, constipation, or both), and often bloating.
- Diagnostic Criteria: IBS is diagnosed based on the Rome IV criteria, which consider the frequency and nature of abdominal pain and its relation to bowel movements.
- Tests: Diagnosis involves ruling out other conditions. This might include blood tests, stool tests, colonoscopy, and breath tests.
- History & Physical Examination: Detailed patient history and physical exams can highlight symptom patterns and rule out other diseases.
- Treatment Response: A positive response to IBS treatments can help confirm the diagnosis.
- Red Flags: Symptoms like unexplained weight loss, blood in stool, or onset after age 50 warrant further investigation to rule out more serious conditions.
While there's no definitive test for IBS, a combination of clinical criteria, exclusion of other diseases, and sometimes a positive response to treatment help reach a diagnosis. As with all medical conditions, a thorough and systematic approach is vital, and patients should work closely with their healthcare providers to ensure an accurate diagnosis.
Treatment for Irritable Bowel Syndrome (IBS)
The treatment of IBS is often multifaceted and tailored to the specific symptoms and triggers of the individual. Here's a summary of the main treatment approaches:
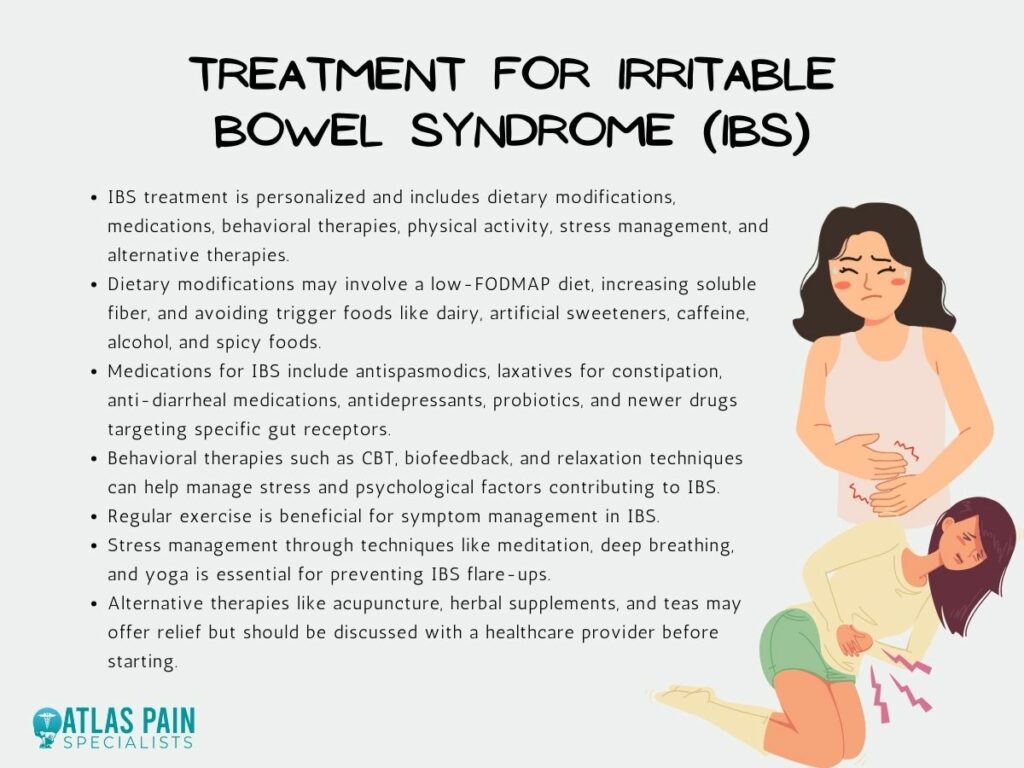
Dietary Modifications:
- Low-FODMAP Diet: This diet restricts certain carbohydrates that can be poorly absorbed in the gut and may exacerbate IBS symptoms in some people.
- Fiber: Increasing dietary fiber can help those with IBS-C (constipation-predominant). Soluble fiber (like psyllium) is often recommended.
- Limiting Problem Foods: Reducing or eliminating foods that trigger symptoms. Common culprits include dairy products, artificial sweeteners, caffeine, alcohol, and spicy foods.
Medications:
- Antispasmodics: Drugs like dicyclomine can help reduce abdominal cramping.
- Laxatives: For IBS-C, over-the-counter options like polyethylene glycol can be helpful.
- Anti-diarrheal Medications: Loperamide can help reduce diarrhea for those with IBS-D.
- SSRIs or TCAs: Low doses of certain antidepressants can help alleviate pain and bowel dysfunction.
- Probiotics: Some patients find relief with certain probiotic strains, although the evidence is still evolving.
- Newer Medications: Drugs like lubiprostone, linaclotide, and Eluxadoline target specific receptors in the gut to regulate bowel motility and pain.
Behavioral Therapies:
- Cognitive Behavioral Therapy (CBT): This can help address the stress or anxiety contributing to IBS symptoms.
- Biofeedback: Helps patients learn to control physiological functions better, potentially improving bowel habits.
- Relaxation Techniques: Techniques such as deep breathing and progressive muscle relaxation can help manage stress that may trigger IBS symptoms.
Physical Activity
Regular exercise has long been recognized for its many health benefits, including cardiovascular health and mental well-being. For those suffering from Irritable Bowel Syndrome (IBS), exercise offers specific advantages, playing a crucial role in symptom management.
Stress Management
One of the most significant contributors to IBS flare-ups is stress. Understanding this connection is vital, as it offers pathways to therapeutic interventions, such as meditation, deep breathing exercises, and yoga.
Alternative Therapies
Acupuncture, herbal supplements, and certain teas might relieve some, but it's essential to consult a healthcare provider before starting these treatments.
Given the individual nature of IBS, what works for one person might not work for another, making it essential to have open communication with healthcare providers and a willingness to try different strategies to find what's most effective.
Conclusion
As we've journeyed through the complexities of Irritable Bowel Syndrome, it's evident that IBS is more than just a passing stomach upset. Its consistent link with abdominal pain underscores the profound impact it can have on sufferers' daily lives.
Gaining clarity on this disorder is about understanding medical jargon and empathizing with the millions who navigate its challenges regularly. As research continues and treatments evolve, we hope for a future where IBS is better understood and more effectively managed.
Knowledge is power, and in understanding IBS, we move one step closer to empowering those affected and improving their quality of life.
About Dr. Sean Ormond



