Spinal Cord Stimulation
In Phoenix Arizona
What is Spinal Cord Stimulation?
SCS is particularly beneficial for patients with persistent nerve pain, such as those caused by failed back surgery syndrome, complex regional pain syndrome (CRPS), and neuropathic pain conditions. It offers a customizable approach, allowing patients and physicians to adjust stimulation levels based on individual needs. Many patients experience a significant reduction in pain and an improved quality of life, regaining mobility and independence that was previously limited by chronic pain.

Benefits of
Spinal Cord Stimulation
Significant Pain Relief
Minimally Invasive Procedure
Reduces Dependence on Medications
Customizable Pain Management

Conditions Treated with Spinal Cord Stimulation
Purpose
Limitations
Risks
Process
Types
Purpose of Spinal Cord Stimulation
The primary goal of Spinal Cord Stimulation is to reduce or block pain signals before they reach the brain, helping patients regain control over their pain without relying on excessive medication. SCS is not a cure for the underlying condition, but it is an effective tool for managing chronic pain that has not responded to physical therapy, injections, or prior surgeries. Many patients who undergo SCS report improved mobility, reduced stress and anxiety related to pain, and enhanced overall well-being. By masking pain with gentle electrical pulses, SCS allows individuals to focus on daily activities rather than being constantly burdened by discomfort.
Limitations of Spinal Cord Stimulation
While SCS can be a life-changing treatment, it isn’t for everyone. It is most effective for nerve-related pain and may not be as beneficial for mechanical or inflammatory pain conditions. Some patients experience partial relief rather than complete pain elimination, and effectiveness can vary from person to person. Additionally, the device requires ongoing management, including periodic adjustments and battery replacements for rechargeable systems.
Another limitation is that insurance coverage may vary, requiring patients to undergo a trial period before permanent implantation. While the treatment can significantly reduce pain, it does not treat the underlying cause of the pain, meaning some conditions may continue to progress despite symptom relief.

Potential Risks of Spinal Cord Stimulation
As with any medical procedure, SCS carries some risks, though complications are rare. Some potential risks include:
- Infection – Though uncommon, an infection at the implant site may require removal of the device.
- Lead Migration – The electrodes may shift over time, leading to reduced effectiveness and requiring adjustment or repositioning.
- Device Malfunction – Though rare, mechanical failures in the device may require replacement.
- Tissue Irritation – Some patients experience mild discomfort or sensitivity around the implant site.
- Inconsistent Pain Relief – While many patients experience significant relief, results can vary, and some may not achieve the expected level of improvement.
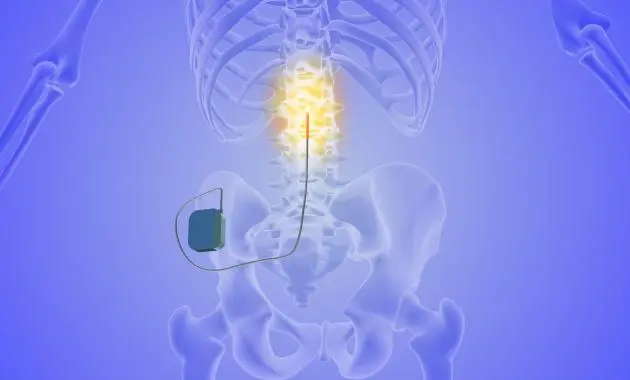
The Spinal Cord Stimulation Process
The SCS procedure involves two main phases: the trial phase and the permanent implant.
- Trial Phase – A temporary SCS device is implanted using a minimally invasive technique. The patient wears an external stimulator for about a week to determine if the therapy provides significant pain relief.
- Evaluation – If the trial is successful (typically at least 50% pain reduction), the patient moves on to permanent implantation.
- Permanent Implantation – A small pulse generator is implanted under the skin, typically near the lower back or abdomen, and connected to leads placed near the spinal cord.
- Device Programming – The device is programmed to deliver customized electrical impulses, which the patient can adjust based on their pain levels.
- Recovery & Follow-Up – Patients typically return to light activity within a few days and receive regular follow-ups to optimize the device’s settings.

Types of Spinal Cord Stimulators
There are different types of SCS devices, each designed to meet the unique needs of the patient:
- Traditional Spinal Cord Stimulators – Deliver mild electrical impulses that replace pain signals with a tingling sensation (paresthesia).
- Burst Stimulation Devices – Use burst pulses to mimic natural nerve firing patterns, often reducing pain without causing a tingling sensation.
- High-Frequency Stimulators – Offer pain relief without paresthesia, making them ideal for patients who find tingling sensations uncomfortable.
- Rechargeable vs. Non-Rechargeable Devices – Rechargeable models provide longer battery life and more flexibility, while non-rechargeable versions require replacement every 5-10 years.
Each patient’s condition, preferences, and lifestyle determine which type of SCS system will provide the best long-term pain relief.
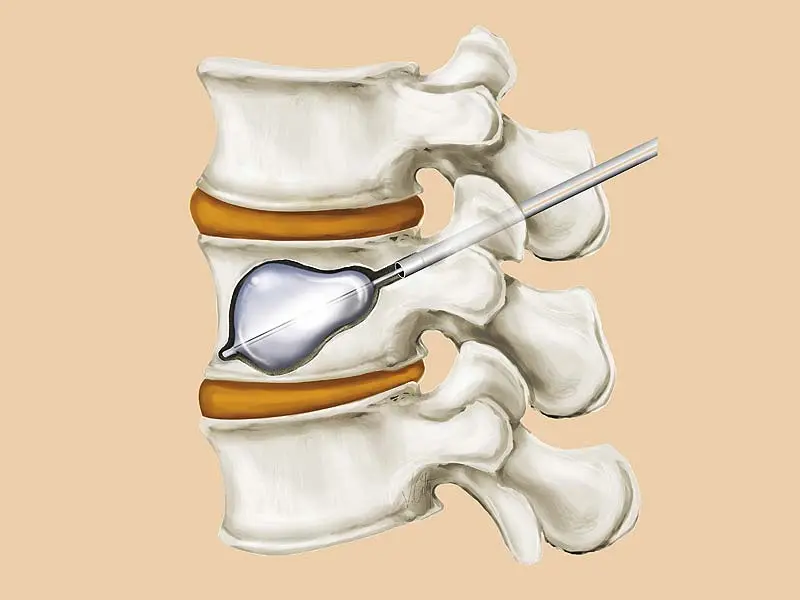
Types of Vertebral Compression Fractures Treated with Kyphoplasty
Kyphoplasty is most effective for acute or subacute compression fractures, meaning fractures that are relatively recent and still causing pain. Some of the common types include:
- Wedge fractures: The front of the vertebra collapses, creating a wedge-like shape and leading to kyphosis (hunchback posture).
- Biconcave fractures: The middle of the vertebra collapses, causing the bone to become concave in appearance.
- Crush fractures: The entire vertebra collapses uniformly, which can lead to severe instability.
The type and severity of the fracture determine whether kyphoplasty or another treatment approach is best.
Ask us anything, or
schedule a same day
appointment.
