Radiofrequency Ablation
In Phoenix Arizona
What is Radiofrequency Ablation (RFA)?
RFA is particularly effective for spinal pain, arthritis-related joint pain, and nerve-related pain conditions. Since the procedure is performed on an outpatient basis with minimal downtime, many patients experience long-lasting pain relief and improved mobility within days. The effects can last anywhere from six months to over a year, making it a preferred choice for those seeking a non-surgical alternative to pain management.
Benefits of
Radiofrequency Ablation
Effective Long-Term Pain Relief
Minimally Invasive with Quick Recovery
Reduces or Eliminates the Need for Medications
Alternative to Surgery
Treats Multiple Pain Conditions
Safe and Repeatable
Conditions Treated with Radiofrequency Ablation
Purpose
Limitations
Risks
Process
Types
Purpose of Radiofrequency Ablation
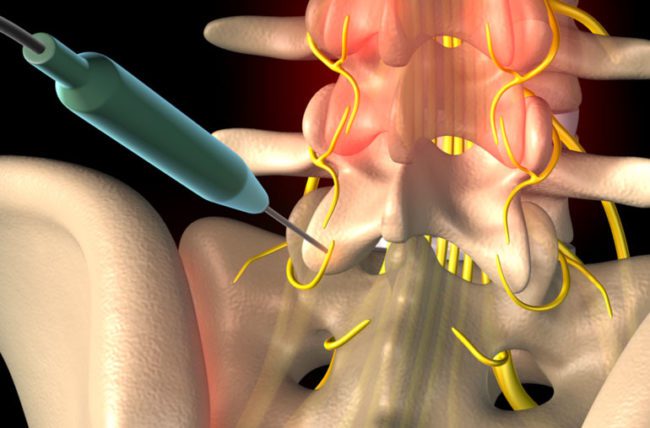
The goal of RFA is to provide long-term pain relief by disrupting pain signals at their source. Instead of relying on temporary pain relief methods like injections or medications, RFA offers a more sustainable solution for chronic pain sufferers. By applying controlled heat energy to specific nerves, the procedure stops pain transmission without affecting surrounding tissues or overall nerve function.
This procedure is often recommended for patients who have successfully responded to diagnostic nerve blocks, indicating that their pain originates from specific nerves. With minimal risks and long-lasting results, RFA helps patients return to normal activities without the burden of chronic pain.
Limitations of Radiofrequency Ablation
While RFA is highly effective, it may not be suitable for all types of pain. It works best for nerve-related pain conditions, meaning that muscle pain, mechanical back pain, or widespread conditions like fibromyalgia may not respond well. Additionally, pain relief from RFA is not permanent, as nerves can regenerate over time. Some patients may require repeat treatments to maintain long-term relief.
Another limitation is that not all nerves are suitable candidates for ablation. Some nerves play a role in essential functions like muscle movement or sensation, meaning they cannot be safely targeted for ablation. Proper diagnostic testing is crucial to determine whether RFA is the right option for a patient’s condition.
Potential Risks of Radiofrequency Ablation
RFA is considered a low-risk procedure, but like any medical treatment, it carries some potential complications. These include:
- Temporary Discomfort – Some patients may experience bruising, soreness, or mild pain at the procedure site, which typically resolves within a few days.
- Nerve Regeneration – While pain relief is long-lasting, the treated nerve may regenerate, requiring additional procedures in the future.
- Infection or Bleeding – Though rare, infection or bleeding at the injection site can occur, particularly in patients with bleeding disorders or those on blood thinners.
- Temporary Weakness or Numbness – Some patients report temporary numbness or weakness in the treated area, which usually resolves over time.
- Rare Nerve Damage – In very rare cases, incorrect placement of the needle can cause unintended nerve damage, leading to altered sensation or discomfort.
Most patients tolerate the procedure very well, and complications are uncommon when performed by an experienced specialist.
The Radiofrequency Ablation Process
The RFA procedure is performed on an outpatient basis and typically takes less than an hour. The steps include:
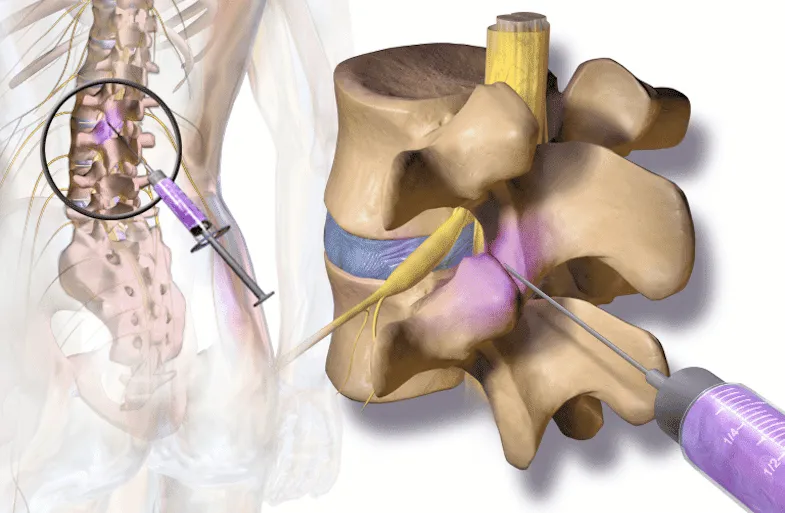
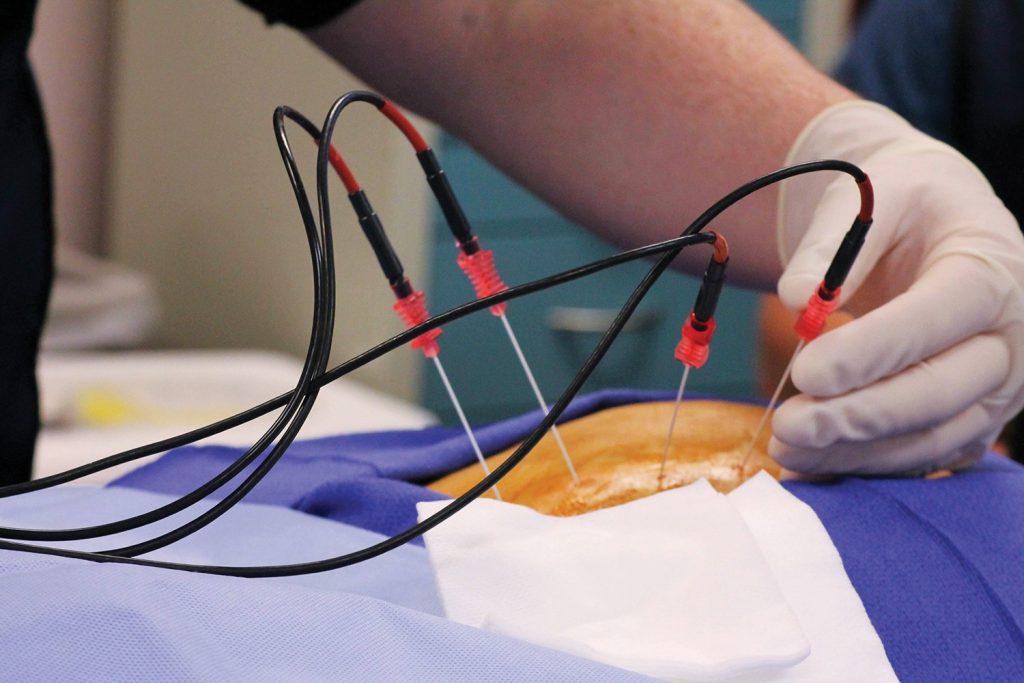
- Preparation & Anesthesia – The patient lies comfortably while the treatment area is numbed with local anesthesia.
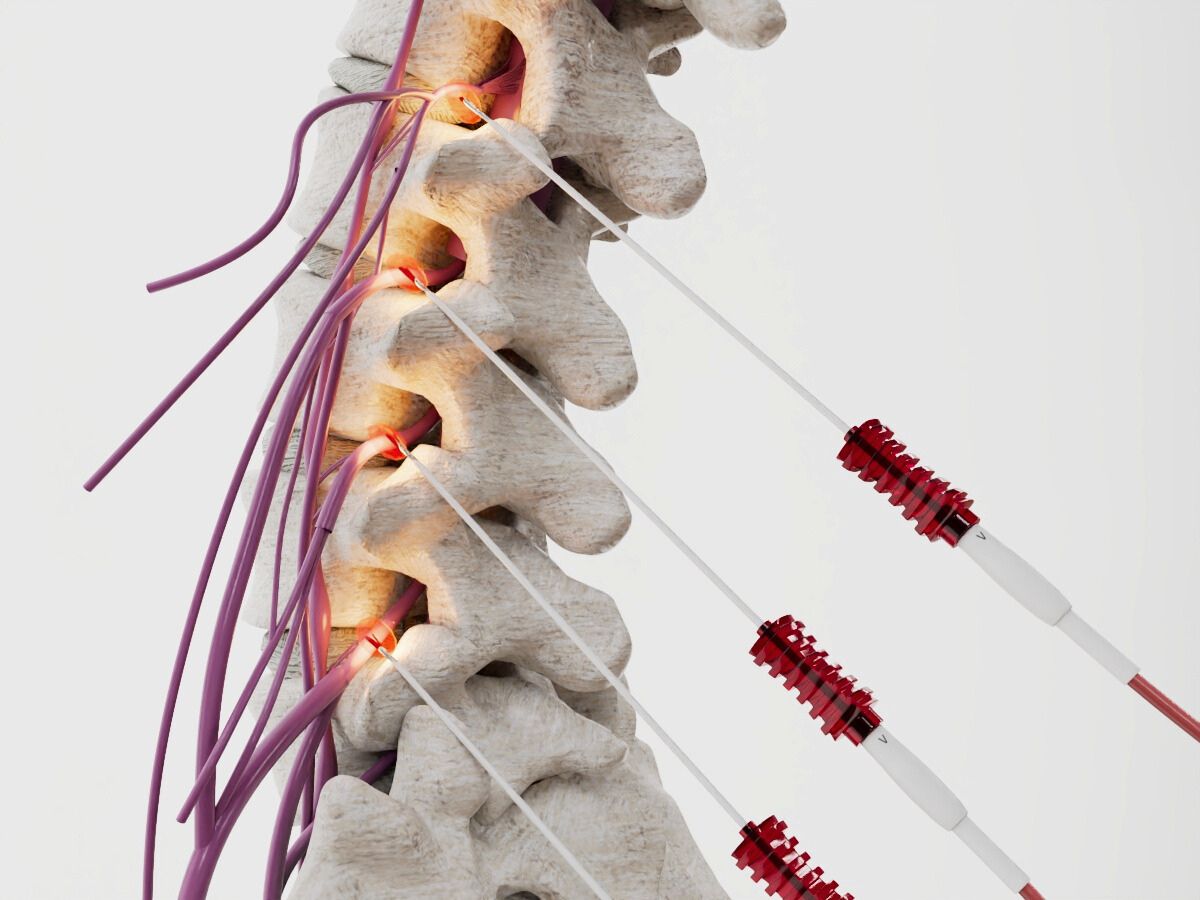
- Needle Placement with Fluoroscopic Guidance – Using X-ray imaging, a small, hollow needle is inserted near the target nerve.
- Testing & Confirmation – A mild electrical current is used to confirm that the correct nerve is being targeted before ablation begins.
- Radiofrequency Energy Application – A controlled heat pulse is applied to the nerve, disrupting its ability to send pain signals.
- Closure & Recovery – The needle is removed, and a small bandage is applied. Patients are monitored briefly before going home the same day.
Recovery is typically quick, with most patients resuming light activities within 24 to 48 hours.
Types of Radiofrequency Ablation
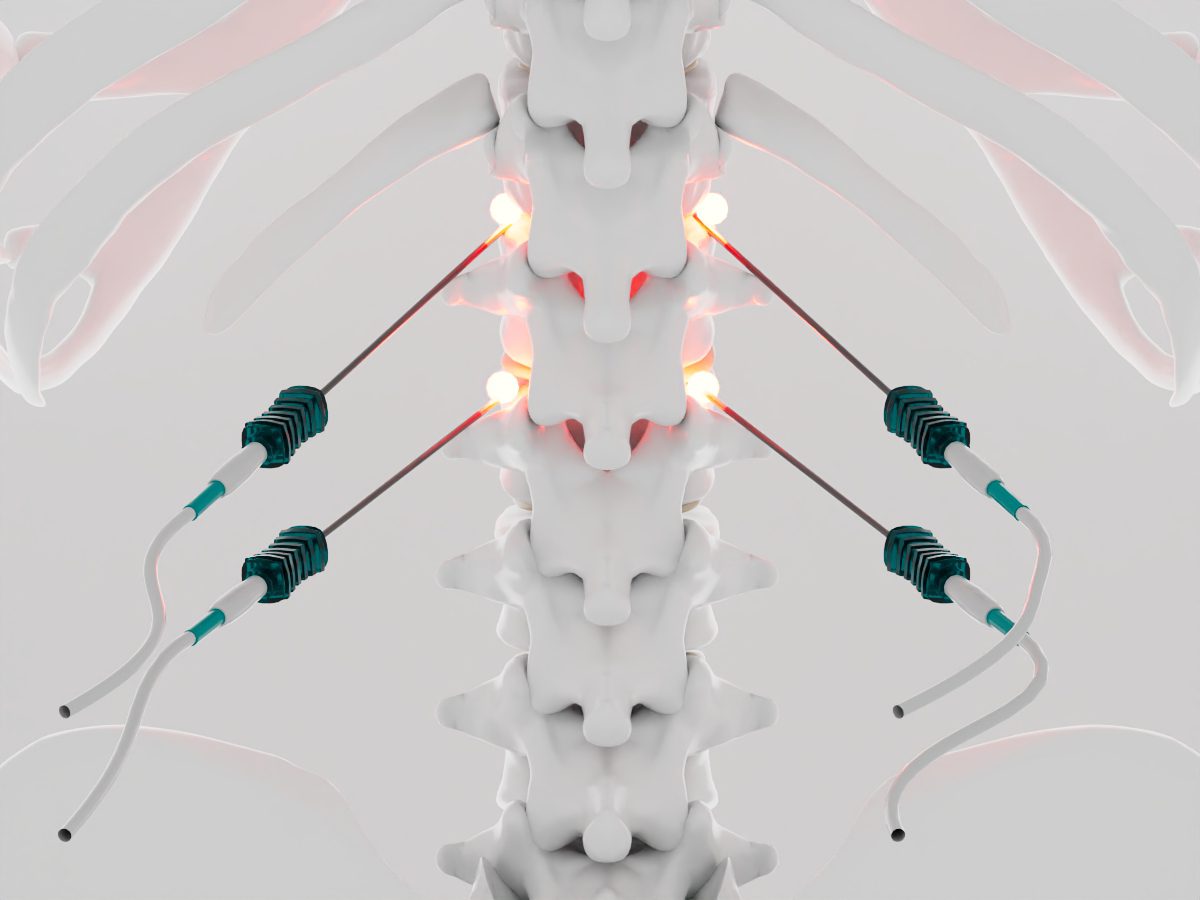
There are different types of RFA, depending on the specific pain condition and treatment approach:
- Conventional (Thermal) RFA – Uses continuous heat energy to create a lesion on the nerve, stopping pain transmission.
- Pulsed RFA – Delivers intermittent pulses of radiofrequency energy at lower temperatures, making it suitable for sensitive nerve areas like those involved in headaches or neuralgia.
- Cooled RFA – Uses a cooled electrode to create a larger lesion, often used for sacroiliac joint pain and other deep nerve structures.
- Water-Cooled RFA – Uses circulating water to prevent excessive heating, reducing tissue damage while still effectively blocking pain signals.
Each technique is customized based on the patient’s pain condition, ensuring optimal results and long-term relief.
Types of Vertebral Compression Fractures Treated with Kyphoplasty
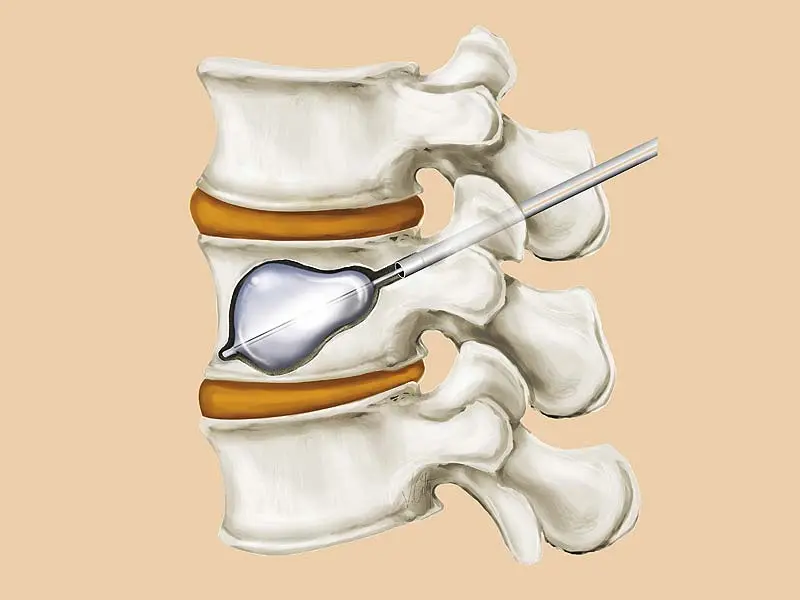
Kyphoplasty is most effective for acute or subacute compression fractures, meaning fractures that are relatively recent and still causing pain. Some of the common types include:
- Wedge fractures: The front of the vertebra collapses, creating a wedge-like shape and leading to kyphosis (hunchback posture).
- Biconcave fractures: The middle of the vertebra collapses, causing the bone to become concave in appearance.
- Crush fractures: The entire vertebra collapses uniformly, which can lead to severe instability.
The type and severity of the fracture determine whether kyphoplasty or another treatment approach is best.
Ask us anything, or
schedule a same day
appointment.
