
Treatment for disc extrusion
The spine is one of the most significant elements of the human skeleton due to its critical involvement in health and wellbeing. It maintains the mobility of the human body and also contains the central spinal nerves, which branch out at different exit locations in the spinal canal to form the peripheral nervous system.
Thus, the spine and its constituent parts must be preserved in excellent health. One of the sections is the intervertebral discs positioned between the spinal vertebrae bones.
A medical problem that might negatively impact these discs is disc extrusion. A disc extrusion is one of the most prevalent kinds of spinal cord damage.
This disease could result in back or neck pain, discomfort, and even more complicated symptoms, including sciatica, pinched nerves, radiculopathy, or myelopathy. Therefore, treatment for disc extrusion is important as soon as it is diagnosed for positive results.
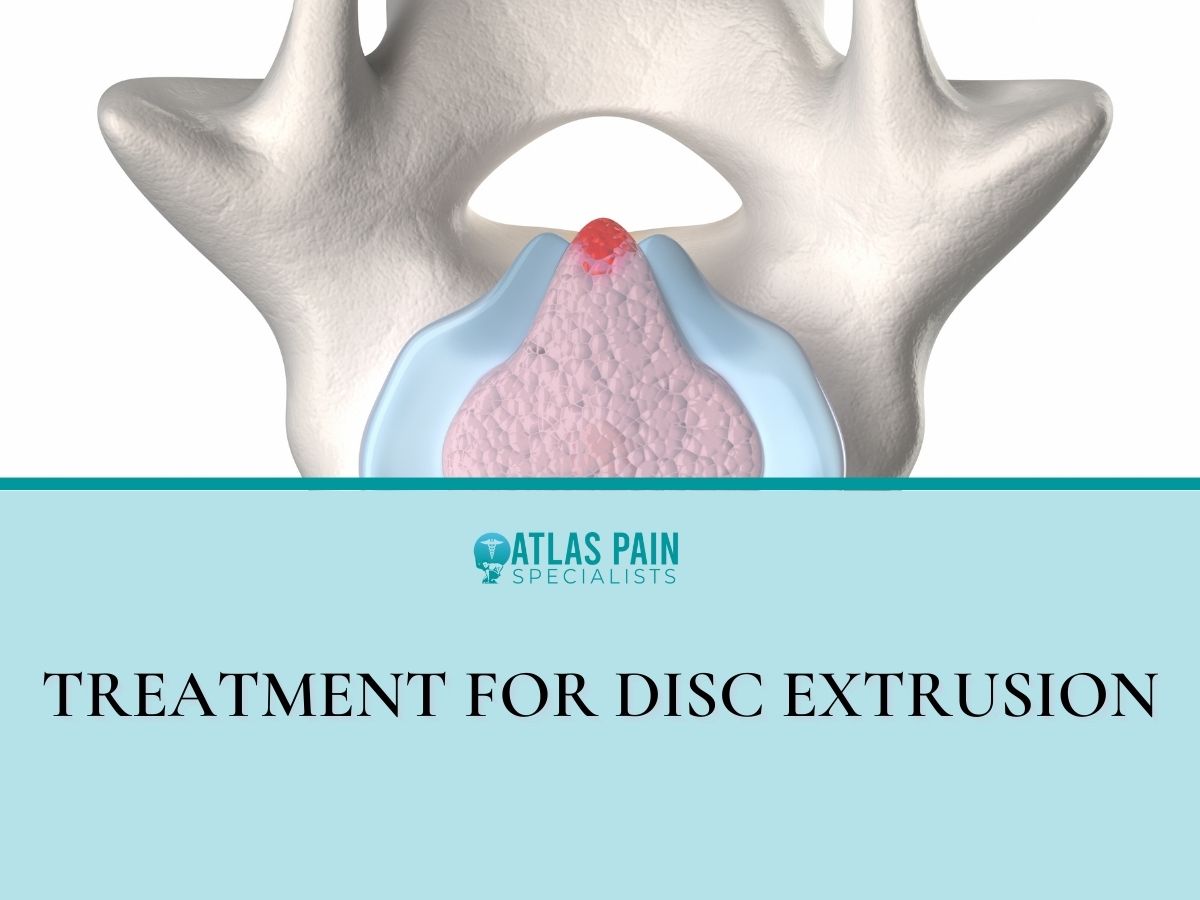
What Is a Disc Extrusion?
A significant disc herniation is a protrusion of the disc. It occurs when the nucleus of an intervertebral disc, or disc nucleus, escapes from the disc's core.
Extruded discs can develop in the neck, mid back, or lower back, resulting in excruciating back pain. Serious arm or leg pain might also ensue if the protruding disc is pushing on a neighboring nerve root.
Pinched nerve and spine pain can be caused by a disc that is out of place in the spine.
Where disc extrusion can occur in the spine
A typical disc extrusion is visible in the spinal segments with the most range of motion and can support the most weight. Disc herniations can induce nerve root impingement in several places in the back.
Extruded cervical and lumbar spine discs press on nerve roots that emerge at a certain level, such as the C6 nerve root at the C5-C6 cervical segment and the L5 nerve root at the L4-L5 segment.
The thoracic spine has the lowest risk of disc extrusion of all the spinal segments. As a result, the discs in the cervical and lumbar spines are more resistant to damage than those in the upper back.
Cervical disc extrusion

- C4-C5 disc extrusion
Stability in the neck is provided by the C4-C5 cervical disc, which protects the C4 and C5 vertebrae from damage. Naturally occurring wear and tear can therefore occur over time. Over time, the cartilaginous ligaments that link the disc to the vertebrae may lose their elasticity, allowing the disc to rupture at any moment.
Degeneration, disc herniation, trauma, and neurological impairment can all result from damage to the C2-C5 motion segment, which includes the C4-C5 disc.
- C5-C6 disc extrusion
As a critical intervertebral component that supports the two "stress" vertebrae that bear the head's weight, the C5-C6 disc is susceptible to various injuries and diseases.
In the C5-C6 region of the spine, poor posture, such as "forward head position," can lead to a wide range of health issues, including neck pain and headaches.
Over time, the natural curvature of the lower neck straightens, putting strain on intervertebral discs and nerves. This can lead to pain and discomfort. A forward head position condition commonly causes a herniated disc in the C5-C6 region.
- C6-C7 disc extrusion
The C6-C7 disc is formed at the intersection of the C6 and C7 cervical vertebrae. An injury often causes a C6-C7 disc extrusion to the cervical spine. The C6-C7 motion segment provides support for the upper neck.
The most movable zone region links the cervical and thoracic spines. Herniation of the C6-C7 segment, which causes nerve impingement and inflammation, is the second most common kind of disc extrusion.
Lumbar disc extrusion
As the spine transitions from lumbar to sacral, the L5-S1 spinal segment, or lumbosacral joint, is a critical area of the lower back.
In this motion segment, the natural curvature of the spine shifts from a forward bend to a backward bend. Weight is transferred from the spine to the legs via this joint. Nerves L5 and S1 are frequently pinched in the lower back.
Symptoms of disc extrusion
As the disc extrusion progresses, its symptoms will change. Cervical and lumbar herniated discs create distinct symptoms.
Shoulders, legs, necks, and backs are frequently affected by inflammation of the nerve roots that control mobility.
The sensory and motor regions associated with the nerve root are generally affected when a herniated disc pinches them. Because of this, patients with a herniated disc may have difficulty doing routine tasks.
Most of the time, these people lose sensation in parts of their body, like their arms, hands, or fingers. These signs and symptoms might be annoying and interfere with everyday life.
Diagnosis of disc extrusion
From the extrusion, patients often experience sensations such as tingling, numbness, loss of mobility, or discomfort. Herniated discs can irritate or compress the nerves in the arms and legs, resulting in these symptoms.
In order to determine the spine's structure and integrity, an MRI will be necessary. A physical examination must determine where and how severe the pain is. A discogram is essential to determine the exact location of the faulty disc in instances when surgery is required to fix it.
Your doctor will examine your back for discomfort during a physical checkup. To pinpoint the source of your discomfort, your doctor may have you lay down and move your legs in various directions.
A physical examination and a review of your medical history are usually sufficient to make the diagnosis of a herniated disk. Your doctor may order the following tests if he or she suspects another ailment or wants to see which nerves are impacted.
Imaging tests

- X-rays. An infection, tumor, misalignment of the spine, or shattered bone can all cause back discomfort, but X-rays can rule out herniated disks.
- CT scan. A CT scanner creates cross-sectional pictures of the spinal column and the structures around it by combining a series of X-rays taken from various angles.
- MRI. The body's interior architecture may be seen using radio waves and a powerful magnetic field. If a herniated disk is found, this test will show you which nerves have been damaged and where the herniation is located.
- Myelogram. Prior to a CT scan, a patient's spinal fluid is injected with a dye. Multiple herniated disks or other problems may cause pressure on the spinal cord or nerves, to be shown by this test.
Nerve tests
Nerve conduction investigations and electromyograms are used to determine how efficiently electrical impulses travel through nerve tissue. Nerve injury can be pinpointed using this method.
- Nerve conduction study. Electrodes inserted on the skin measure this test's electrical nerve impulses and muscle and nerve function. When a tiny current is applied to a neuron, the electrical impulses in the nerve signals are measured.
- Electromyography (EMG). An EMG involves the insertion of a needle electrode into several muscles by a physician. During a muscular contraction, the electrical activity of the muscle is measured.
Treatment for disc extrusion
Most people's symptoms can be alleviated within a few days or weeks with conservative therapy, which consists mostly of altering activities to prevent movement that causes pain and taking pain medication.
Medications

- Nonprescription pain medications. There are several over-the-counter medications that can ease your discomfort, such as acetaminophen (Tylenol) or naproxen sodium (Advil) (Aleve).
- Neuropathic drugs. These medications work by altering the transmission of nerve impulses. Gabapentin, pregabalin (Lyrica), duloxetine (Cymbalta, Drizalma Sprinkle), and gabapentin (Gralise, Horizant, Neurontin) are only a few examples (Effexor XR).
- Muscle relaxers. If you suffer from muscular spasms, you may be prescribed these. A typical adverse effect is a drowsiness and dizziness.
- Opioids. Many clinicians are wary of prescribing opioids for disk herniation because of the risk of addiction and the negative effects. Your doctor may prescribe codeine or an oxycodone-acetaminophen combination if other drugs fail to alleviate your discomfort (Percocet, Oxycet). These medicines may cause adverse effects of sedation, nausea, disorientation, and constipation.
- Cortisone injections. Corticosteroids, which may be injected into the spinal nerves, may be recommended by your doctor if oral treatments fail to alleviate your pain. An MRI study of the spine can assist in needle placement.
Therapy
In order to alleviate your discomfort, your doctor may recommend physical therapy. Herniated disk discomfort can be alleviated with the help of physical therapists, who can demonstrate various postures and exercises.
Surgery

Discectomy:
Surgery is seldom necessary for persons who have herniated disks. If conservative therapy fails to alleviate your symptoms after six weeks, your doctor may recommend surgery, especially if:
- Difficulty standing or walking due to numbness or weakness
- Poorly managed pain
- Inability to regulate one's bowels or bladder
Surgeons are able to remove the projecting piece of the disk in virtually all cases. A handful of times, the entire disk must be replaced. A bone transplant may be necessary for certain situations.
Metal hardware is inserted into the spine to stabilize it throughout the months-long bone fusion procedure. Your surgeon, on rare occasions may recommend an artificial disk.
Process:
Endoscopic spine surgery is conducted with the patient sedated at our state-of-the-art surgery center. Endoscopically, a 7mm incision is all that is required for this surgery.
The procedure is essentially bloodless and takes around 30 minutes for each disc to be fixed. Yes, you read it correctly; a permanent repair will be made to your own natural disc so that you no longer experience discomfort.
In order to view the damaged disc, an endoscope and a high-definition camera are inserted through a 14-inch incision. While the majority of the patient's disc is left in place to maintain spinal mobility and function, just the damaged disc tissue is removed with this procedure. When a patient has had their natural disc fixed, there is no need for fusions or artificial discs to be used.
It employs a precise laser to melt the herniated tissue and provides the most successful laser spine surgery. Unlike conventional microdiscectomy, artificial discs, and spinal fusions, the bone and surrounding tissues are not injured or removed during this treatment.
Instead of drilling through bone like in a microdiscectomy, the doctor utilizes FDA-approved equipment to reach the disc through a naturally occurring gap in the spine. Drilling into bone weakens the spine, leading to more problems requiring spinal fusion surgery in the future.
The body can begin to mend itself spontaneously when the herniation and annular tear have been gently evaporated. Inflammation around the spine diminishes, and nerve root pressure symptoms diminish. It takes time for the disc to return to its pre-injury state.
Patients wake up to immediate relief and a surgical scar so thin that the surgeon may cover it with a Band-aid following surgery. Hospitalization is unnecessary when only a few drops of blood are lost. Outpatient Laser Disc Repair operations have been performed on 1,300 patients so far.
Invasive, risky surgery that only succeeds half the time is absurd. Laser Disc Repair is a no-brainer when compared to other surgical options, including microdiscectomy, laminectomy, spinal fusion, and complete disc replacement. Your health is in jeopardy by undergoing traditional spine surgery, which is needless and risky.
The advice and information in this article are intended solely for educational purposes and should not be seen as a substitute for professional medical advice or judgment. After speaking with your doctor, follow any medical advice you get from this site or any other source. If you have any questions or concerns, feel free to make an appointment with one of our doctors at Atlas.
Frequently Asked Questions
What causes disc extrusion?
Disc herniation can be caused by a variety of diseases, each of which might have an impact on one or more joints. Spinal wear and strain are the most typical explanations for this.
As we age, the cartilage connecting the spinal discs to the vertebrae might become less elastic. When an accident or fall occurs, the immediate impact and trauma can cause herniated discs.
About Dr. Sean Ormond



