
The Connection Between Hormones and Pain Perception in Women
The connection between hormones and pain perception in women constitutes a dynamic and intricate relationship that significantly influences healthcare practices and patient experiences. Across various life stages, from menstruation to pregnancy and menopause, hormonal fluctuations exert profound effects on pain sensitivity and perception. Understanding this interplay is paramount for healthcare providers in developing tailored pain management strategies that address the unique needs of female patients.
This article explores the multifaceted dynamics of hormones and pain perception in women, delving into the implications for treatment and empowerment. Through an in-depth examination of menstrual cycle influences, pregnancy-related pain experiences, menopausal transitions, and the impact on chronic pain conditions, this article elucidates the complex nexus between hormones and pain perception.
Hormonal Fluctuations and Pain Sensitivity in Women
The ebb and flow of hormones significantly impact how women experience pain, influencing a complex interplay of biological, psychological, and social factors. From menstrual cycles to pregnancy, childbirth, and menopause, changes in estrogen, progesterone, and other hormones intricately shape how pain is perceived and managed.
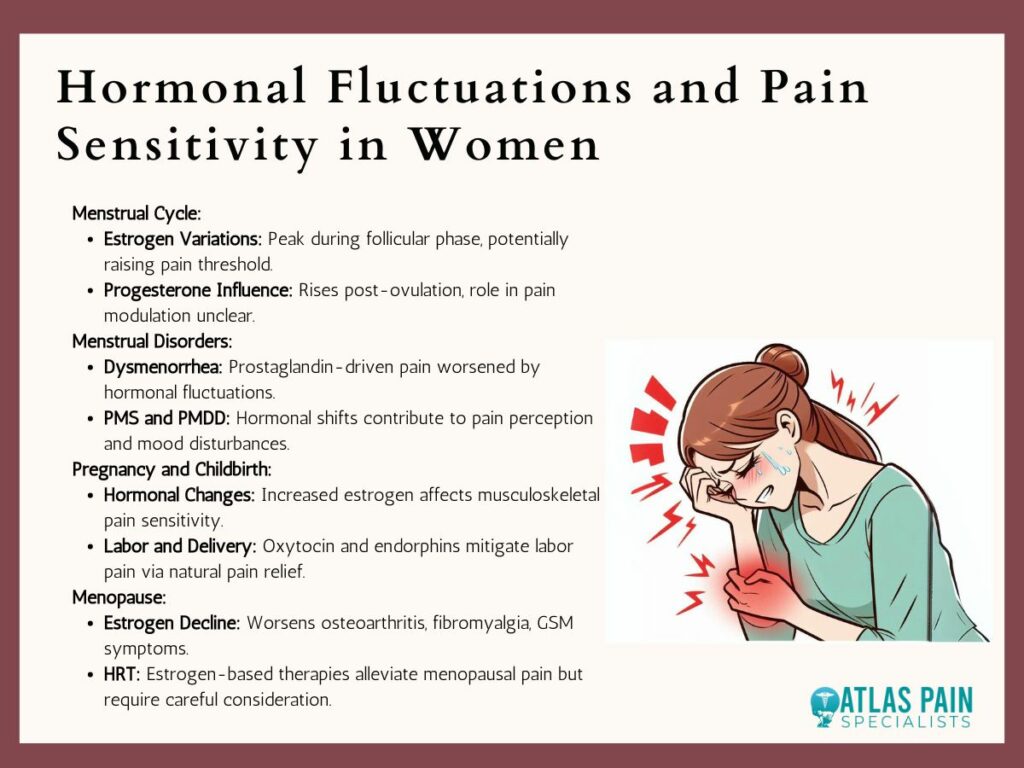
Menstrual Cycle
- Estrogen Variations: Estrogen levels fluctuate throughout the menstrual cycle, peaking during the follicular phase. Elevated estrogen levels may alleviate pain by affecting neurotransmitter activity and reducing inflammation, leading to a higher pain threshold and decreased sensitivity, particularly to musculoskeletal pain and headaches.
- Progesterone Influence: Conversely, progesterone levels rise during the luteal phase post-ovulation. While progesterone's role in pain modulation isn't fully understood, evidence suggests it may heighten pain sensitivity through interactions with neuroendocrine pathways, potentially increasing susceptibility to pain stimuli during this phase.
Menstrual Disorders
- Dysmenorrhea: Severe menstrual pain, or dysmenorrhea, is closely tied to hormonal imbalances and increased prostaglandin production. Prostaglandins induce uterine contractions and inflammation, worsening cramping and abdominal discomfort during menstruation. Fluctuations in estrogen and progesterone exacerbate these symptoms, contributing to the cyclic nature of dysmenorrhea.
- Premenstrual Syndrome (PMS) and Premenstrual Dysphoric Disorder (PMDD): Hormonal shifts throughout the menstrual cycle influence the development of PMS and PMDD, characterized by physical and psychological symptoms before menstruation. Changes in pain perception, mood disturbances, and stress sensitivity are common, highlighting the complex interplay between hormones and pain pathways.
Pregnancy and Childbirth
- Hormonal Changes: Pregnancy brings significant hormonal shifts, with rising estrogen levels and other hormones influencing pain sensitivity. Increased estrogen contributes to joint mobility and ligament laxity, predisposing women to musculoskeletal pain, especially in the lower back and pelvis. Hormonal changes during pregnancy also affect neuropathic pain perception and alter pain thresholds.
- Labor and Delivery: During childbirth, the release of oxytocin, known as the "love hormone," and endorphins act as natural pain relievers, easing labor pain and promoting well-being. This hormonal cascade underscores the intricate relationship between hormones and pain perception during reproductive experiences.
Menopause
- Estrogen Decline: Menopause involves declining estrogen levels, exacerbating conditions like osteoarthritis, fibromyalgia, and genitourinary syndrome of menopause (GSM). Estrogen withdrawal may worsen chronic pain symptoms, emphasizing the role of hormonal fluctuations in pain during menopause.
- Hormone Replacement Therapy (HRT): HRT is sometimes used to alleviate menopausal symptoms and associated pain. Estrogen-based HRT can relieve vasomotor symptoms, musculoskeletal pain, and genitourinary discomfort in menopausal women. However, the risks and benefits of HRT should be carefully considered based on individual health profiles and preferences.
Hormonal fluctuations significantly influence pain sensitivity and response mechanisms in women across various life stages. Understanding the interplay between hormones and pain perception is crucial for tailoring pain management approaches and addressing the unique needs of women coping with pain.
Understanding Pain Perception
Pain perception is a multifaceted process involving the detection, interpretation, and response to noxious stimuli. It includes sensory, cognitive, emotional, and behavioral elements, making it highly subjective and influenced by various factors.
Nociceptors, specialized nerve fibers, detect potential harm and transmit signals to the brain, where sensory information is processed and integrated. However, pain perception isn't solely determined by stimulus intensity; biological, psychological, and social factors also play crucial roles.
Genetics, past experiences, culture, and emotional state contribute to an individual's pain experience. The brain modulates pain perception through "top-down" regulation, where cognitive factors like attention and coping strategies influence pain intensity. Emotions such as stress and anxiety can sensitize pain pathways, while social support can alleviate pain.
Understanding these complexities helps healthcare professionals develop effective pain management strategies, ultimately improving individuals' quality of life.
The Key Players in Pain Perception for Women
In the intricate landscape of pain perception in women, several key players orchestrate the experience and modulation of pain. These include:
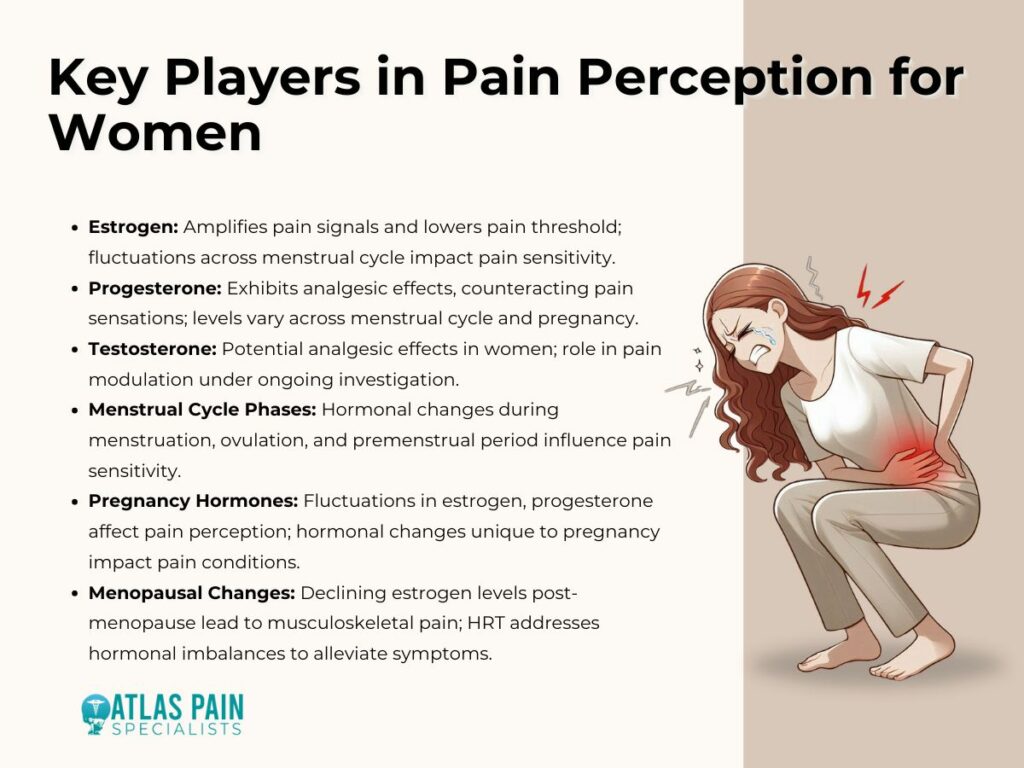
Estrogen
Often considered a primary regulator in women's health, estrogen exerts multifaceted effects on pain perception. It can enhance pain sensitivity by amplifying pain signals and lowering the pain threshold. Fluctuations in estrogen levels across the menstrual cycle contribute to variations in pain perception, with some women experiencing heightened sensitivity during specific phases, such as menstruation or menopause transition.
Progesterone
Working in tandem with estrogen, progesterone plays a crucial role in modulating pain perception. Unlike estrogen, progesterone exerts analgesic effects, mitigating pain sensations. The balance between estrogen and progesterone levels influences women's pain experiences, with fluctuations during the menstrual cycle and pregnancy impacting pain thresholds.
Testosterone
While often overshadowed in discussions of pain perception in women, testosterone also contributes to the modulation of pain. Research suggests that testosterone may have analgesic effects, potentially reducing pain sensitivity. However, its precise role in women's pain perception remains an area of ongoing investigation.
Menstrual Cycle Phases
The menstrual cycle itself serves as a significant influencer of pain perception in women. Hormonal fluctuations during different phases of the menstrual cycle, such as menstruation, ovulation, and the premenstrual period, can profoundly impact pain sensitivity. Estrogen withdrawal during menstruation and hormonal surges during ovulation are associated with changes in pain perception.
Pregnancy Hormones
Pregnancy introduces a unique hormonal milieu characterized by fluctuations in estrogen, progesterone, and other hormones. These hormonal changes can influence pain perception, with some women experiencing alleviation of certain pain conditions while others develop new or exacerbated symptoms. Hormones like progesterone contribute to uterine relaxation, potentially alleviating pelvic pain, while physiological adaptations during pregnancy can predispose women to musculoskeletal pain.
Menopausal Changes
The hormonal transition of menopause, marked by declining estrogen levels, significantly impacts pain perception in women. Postmenopausal women commonly report musculoskeletal pain attributed to estrogen deficiency and its effects on bone density and musculoskeletal health. Hormone replacement therapy (HRT) aims to address these hormonal imbalances and alleviate menopause-related symptoms, including pain.
These key players interact within a complex network of physiological, psychological, and sociocultural factors to shape women's experiences of pain throughout their lives. Understanding these dynamics is essential for developing tailored approaches to pain management and promoting women's health and well-being.
Implications for Pain Management
Understanding the intricate relationship between hormones and pain perception is essential for devising tailored and effective pain management strategies for women. By acknowledging how hormonal fluctuations influence pain experiences, healthcare providers can customize treatment plans to address the unique needs of female patients across different stages of life.
Tailored Treatment
Recognizing the impact of hormonal fluctuations on pain sensitivity enables healthcare providers to tailor treatment approaches accordingly. For example, during specific phases of the menstrual cycle, such as the premenstrual period when estrogen levels drop, women may experience heightened pain sensitivity. By adjusting pain medication dosages or recommending specific therapies based on menstrual cycle tracking, healthcare providers can better manage pain symptoms and improve treatment outcomes.
Hormone Replacement Therapy (HRT)
For women experiencing chronic pain during perimenopause or menopause, hormonal fluctuations can exacerbate symptoms and contribute to discomfort. Hormone replacement therapy (HRT) offers a potential solution by replenishing declining estrogen and progesterone levels. By stabilizing hormonal balance, HRT may help alleviate pain and improve overall quality of life for menopausal women experiencing pain-related symptoms.
Pain Education
Educating women about the connection between hormones and pain empowers them to recognize patterns and advocate for themselves during medical consultations. Understanding how hormonal fluctuations can influence pain perception allows women to better communicate their symptoms and preferences to healthcare providers. This knowledge fosters a collaborative approach to pain management, where women actively participate in decision-making and treatment planning based on their individual experiences and needs.
Integrating knowledge of hormonal influences on pain perception into clinical practice enables healthcare providers to develop personalized and effective pain management strategies for women. By tailoring treatments, considering hormone replacement therapy options, and promoting pain education, healthcare providers can improve outcomes and enhance the well-being of women experiencing pain across various life stages.
Conclusion
Understanding the intricate relationship between hormones and pain perception in women reveals the diverse nature of pain experiences across life stages. From menstruation to pregnancy and menopause, hormonal fluctuations profoundly shape pain sensitivity. This awareness is vital for tailoring effective pain management strategies.
Throughout this article, we've explored how hormonal dynamics influence pain experiences, from menstrual cycles to menopausal transitions. By recognizing these influences, healthcare providers can offer personalized care and empower women to advocate for themselves during consultations.
Integrating knowledge of hormonal influences into clinical practice is essential for enhancing pain management outcomes.
By adopting holistic approaches that consider hormonal fluctuations, healthcare providers can better support women in navigating pain across various life stages. This fosters patient-centered care that prioritizes individual needs and ensures comprehensive support for women's well-being.
About Dr. Sean Ormond