The Connection Between Gut Health and Chronic Pain: Dietary Considerations
The intricate relationship between gut health and chronic pain is a growing area of interest in medical research. The gut microbiome, a complex ecosystem of trillions of microorganisms, plays a crucial role in maintaining overall health and regulating pain.
Emerging evidence suggests that dietary interventions can significantly impact gut health and, consequently, chronic pain management. By incorporating dietary fiber, omega-3 fatty acids, polyphenols, and probiotics while avoiding processed foods, individuals can support a healthy gut microbiome and potentially alleviate chronic pain.
This article explores these dietary considerations and their benefits for gut health and pain management.
Gut Microbiome and Pain
In recent years, the intricate relationship between gut health and chronic pain has garnered increasing attention from researchers and healthcare professionals. The gut microbiome, which consists of trillions of microorganisms residing in the intestines, plays a pivotal role in maintaining overall health.
Emerging evidence suggests that an imbalance in gut microbiota, known as dysbiosis, may contribute to the development and persistence of chronic pain. Understanding this connection and implementing dietary strategies to support a healthy gut can offer promising avenues for managing chronic pain.
The Gut-Brain Axis and Pain Regulation
The gut-brain axis is a bidirectional communication network linking the gut and the central nervous system. This complex system involves neural, hormonal, and immunological pathways.
One of the key mechanisms through which the gut microbiome influences pain is the production of neurotransmitters and signaling molecules. For instance, certain gut bacteria produce short-chain fatty acids (SCFAs) such as butyrate, propionate, and acetate, which have anti-inflammatory properties and can modulate pain perception.
The gut microbiome can influence the production of serotonin, a neurotransmitter that plays a crucial role in mood regulation and pain modulation. Approximately 95% of the body's serotonin is produced in the gut. Dysbiosis can disrupt serotonin production, potentially leading to increased pain sensitivity and chronic pain conditions.
Chronic Pain and Gut Dysbiosis
Chronic pain conditions, such as fibromyalgia, irritable bowel syndrome (IBS), and chronic pelvic pain, have been associated with alterations in gut microbiota. Research has shown that individuals with these conditions often exhibit reduced diversity in their gut microbiome and an imbalance between beneficial and harmful bacteria. This dysbiosis can exacerbate inflammation, disrupt immune function, and amplify pain signals.
For example, patients with IBS often experience abdominal pain and discomfort, which is believed to be linked to gut dysbiosis and increased intestinal permeability, also known as "leaky gut." This condition allows harmful substances to enter the bloodstream, triggering systemic inflammation and pain.
Dietary Considerations
The connection between gut health and chronic pain has become a focal point of research, highlighting the significant role the gut microbiome plays in overall health. The gut microbiome, comprised of trillions of microorganisms, influences various bodily functions, including the modulation of pain.
Dietary interventions can support a healthy gut microbiome, potentially reducing chronic pain. Here are key dietary considerations to optimize gut health and manage chronic pain:
Dietary Fiber
Increasing dietary fiber intake is crucial for promoting a healthy gut microbiome. Fiber serves as a prebiotic, providing nourishment for beneficial gut bacteria. This, in turn, fosters a diverse and balanced microbiome, which is essential for overall health and pain management.

Sources of Dietary Fiber:
- Fruits: Apples, bananas, berries, pears, and oranges.
- Vegetables: Broccoli, carrots, leafy greens, and Brussels sprouts.
- Whole Grains: Oats, brown rice, quinoa, and whole wheat products.
- Legumes: Beans, lentils, chickpeas, and peas.
- Nuts and Seeds: Almonds, chia seeds, flaxseeds, and walnuts.
Dietary fiber helps regulate bowel movements, prevent constipation, and promote the production of short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory properties. By supporting gut health, fiber can indirectly contribute to the reduction of chronic pain.
Omega-3 Fatty Acids
Omega-3 fatty acids are renowned for their anti-inflammatory properties and their ability to support gut health. These essential fats play a vital role in reducing systemic inflammation, which is often a key factor in chronic pain conditions.

Sources of Omega-3 Fatty Acids:
- Fatty Fish: Salmon, mackerel, sardines, and trout.
- Flaxseed: Ground flaxseed or flaxseed oil.
- Walnuts: A convenient snack or addition to meals.
- Chia Seeds: Can be added to smoothies, yogurt, or salads.
Incorporating omega-3 fatty acids into the diet can help modulate inflammatory processes and improve the integrity of the gut barrier, thereby contributing to the management of chronic pain.
Polyphenols
Polyphenols are micronutrients with antioxidant properties found in various plant-based foods. These compounds help reduce oxidative stress and inflammation, promoting overall gut health and potentially alleviating chronic pain.
Sources of Polyphenols:
- Fruits: Berries (blueberries, strawberries, raspberries), apples, and grapes.
- Vegetables: Spinach, kale, onions, and broccoli.
- Beverages: Green tea, black tea, and coffee.
- Nuts and Seeds: Almonds, hazelnuts, and flaxseeds.
- Dark Chocolate: Choose products with high cocoa content for maximum benefits.
Polyphenols support the growth of beneficial gut bacteria and inhibit the growth of harmful bacteria. By reducing inflammation and oxidative stress, these compounds can play a significant role in pain management.
Probiotics
Probiotics are live beneficial bacteria that can be introduced into the gut through fermented foods or supplements. These microorganisms help maintain a balanced gut microbiome, which is essential for reducing inflammation and managing chronic pain.

Sources of Probiotics:
- Fermented Foods: Yogurt, kefir, sauerkraut, kimchi, miso, and kombucha.
- Supplements: Various probiotic supplements are available, containing strains like Lactobacillus and Bifidobacterium.
Regular consumption of probiotics can enhance gut health, improve digestion, and support immune function, all of which can contribute to the reduction of chronic pain.
Avoid Processed Foods
Processed foods often contain additives, preservatives, and high levels of sugar and unhealthy fats, which can disrupt the gut microbiome and contribute to inflammation and chronic pain. Limiting or avoiding processed foods is crucial for maintaining a healthy gut.

Examples of Processed Foods to Avoid:
- Sugary Snacks and Beverages: Sodas, candies, and pastries.
- Fast Food: Burgers, fries, and fried chicken.
- Packaged Snacks: Chips, crackers, and processed cheese.
- Processed Meats: Sausages, hot dogs, and deli meats.
Processed foods can promote the growth of harmful bacteria and reduce microbial diversity, leading to dysbiosis. By minimizing the intake of these foods, individuals can support a healthier gut environment and potentially alleviate chronic pain.
Practical Dietary Tips
Implementing these dietary considerations can significantly impact gut health and chronic pain management. Here are some practical tips to incorporate these changes into daily life:
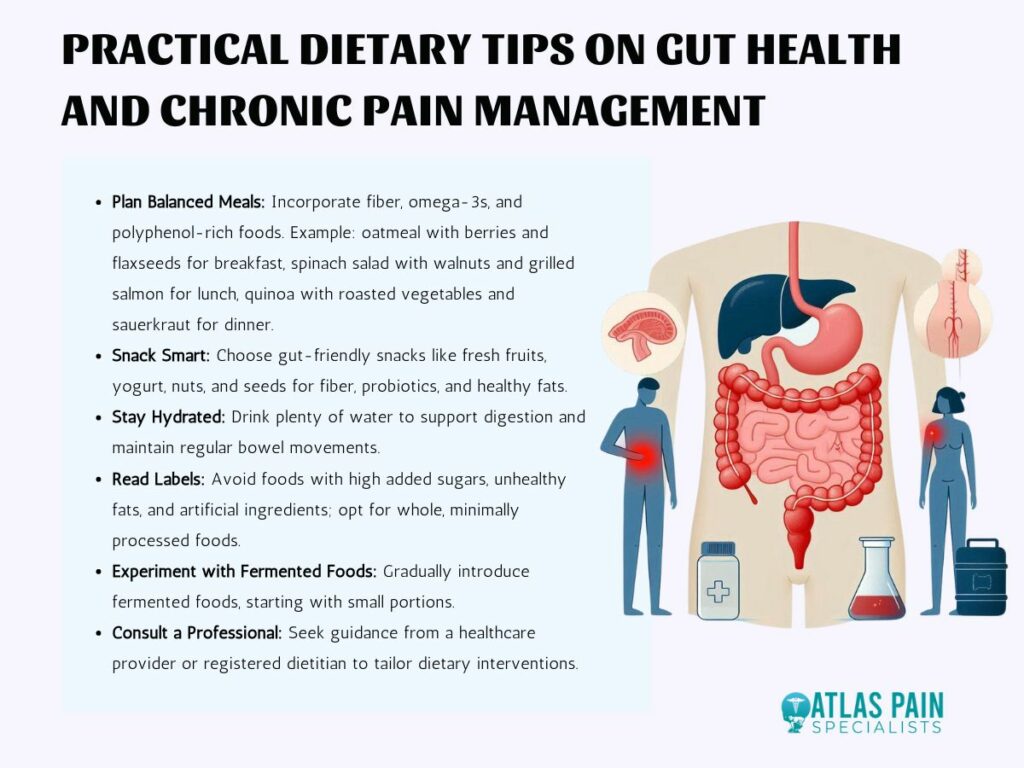
- Plan Balanced Meals: Ensure each meal includes a source of fiber, omega-3 fatty acids, and polyphenol-rich foods. For example, a breakfast of oatmeal topped with berries and flaxseeds, a lunch of a spinach salad with walnuts and grilled salmon, and a dinner of quinoa with roasted vegetables and a side of sauerkraut can provide a balanced intake of these nutrients.
- Snack Smart: Choose gut-friendly snacks such as fresh fruits, yogurt, nuts, and seeds. These options provide fiber, probiotics, and healthy fats, supporting gut health throughout the day.
- Stay Hydrated: Drink plenty of water to support digestion and overall gut health. Proper hydration is essential for maintaining regular bowel movements and preventing constipation.
- Read Labels: Be mindful of food labels and avoid products with high levels of added sugars, unhealthy fats, and artificial ingredients. Opt for whole, minimally processed foods whenever possible.
- Experiment with Fermented Foods: Introduce fermented foods gradually into the diet to see how they affect gut health and pain levels. Start with small portions and increase intake as tolerated.
- Consult a Professional: Working with a healthcare provider or a registered dietitian can help tailor dietary interventions to individual needs and conditions, ensuring the most effective approach to managing chronic pain through diet.
Conclusion
Optimizing gut health through mindful dietary choices offers a promising strategy for managing chronic pain. By increasing dietary fiber, incorporating omega-3 fatty acids and polyphenol-rich foods, consuming probiotics, and avoiding processed foods, individuals can foster a balanced and diverse gut microbiome.
These dietary interventions can help reduce inflammation, support gut integrity, and modulate pain. Embracing these nutritional strategies not only enhances gut health but also contributes to overall well-being and improved quality of life. For tailored advice, consulting with healthcare professionals or registered dietitians can further enhance the effectiveness of these dietary approaches.
About Dr. Sean Ormond



