Shin Splints and Stress Fractures: Identifying and Managing Leg Injuries in Athletics
Shin splints and stress fractures stand as prevalent lower limb injuries among athletes, posing significant challenges to their performance and well-being. These conditions often arise from overuse, biomechanical factors, and training errors, impacting individuals engaged in high-impact sports and activities.
Understanding the distinct characteristics, prevention strategies, and treatment approaches for shin splints and stress fractures is paramount for athletes, coaches, and healthcare professionals alike.
In this comprehensive guide, we explore the causes, symptoms, prevention, and treatment of shin splints and stress fractures, aiming to equip individuals with the knowledge and tools necessary to mitigate the risk of these injuries and optimize recovery outcomes.
Identifying the Causes of Shin Splints
Shin splints, medically known as medial tibial stress syndrome (MTSS), refer to pain along the shinbone (tibia), the large bone in the front of the lower leg.
Common causes of shin splints include overuse, biomechanical issues, and inadequate footwear. These factors lead to repetitive stress on the shinbone during activities like running or jumping. Overuse, biomechanical problems, and poor footwear contribute to muscle fatigue and increased strain on the shins. Understanding these causes is vital for preventing and managing shin splints in athletes.
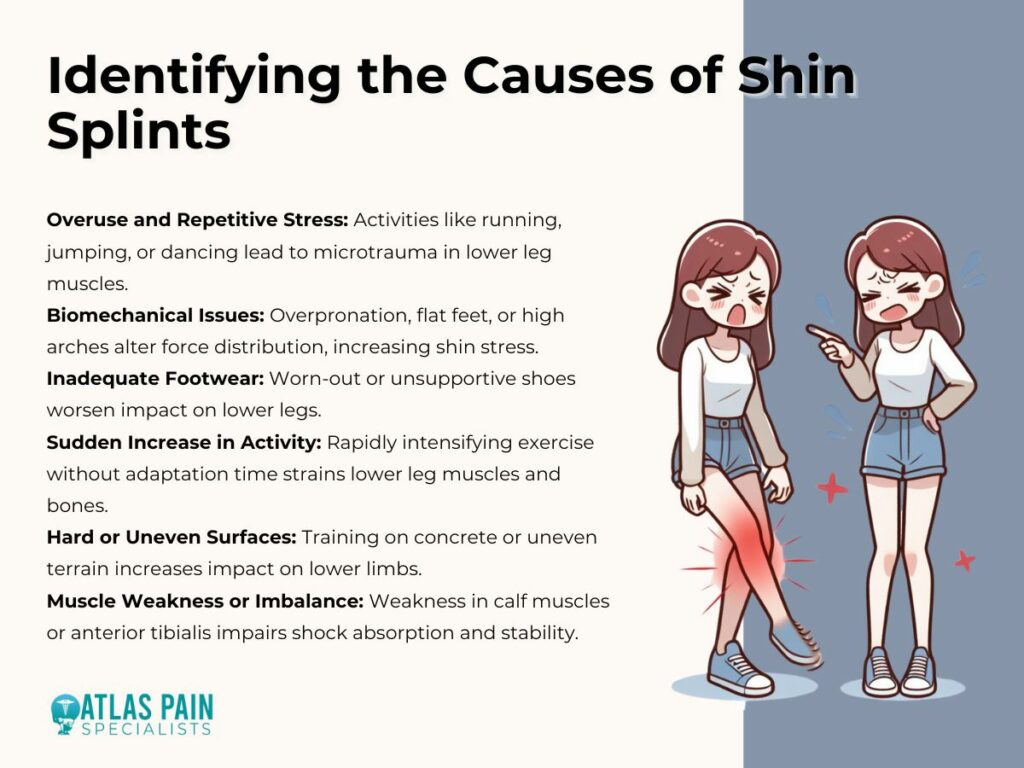
1. Overuse and Repetitive Stress
Shin splints often occur due to repetitive stress on the shinbone and surrounding muscles. Activities such as running, jumping, dancing, or high-impact sports can lead to microtrauma in the muscles and bones of the lower leg.
2. Biomechanical Issues
Faulty biomechanics, such as overpronation (excessive inward rolling of the foot), flat feet, or high arches, can contribute to the development of shin splints. These biomechanical abnormalities can alter the distribution of forces along the lower extremities, increasing stress on the shins.
3. Inadequate Footwear
Wearing improper or worn-out footwear lacking adequate support and cushioning can exacerbate the impact on the lower legs, predisposing individuals to shin splints. Shoes that do not provide sufficient shock absorption can increase the strain on the shinbone and surrounding tissues.
4. Sudden Increase in Intensity or Duration of Activity
Abruptly ramping up the intensity, duration, or frequency of exercise without allowing adequate time for the body to adapt can overload the muscles and bones of the lower leg, leading to shin splints.
5. Hard or Uneven Surfaces
Training on hard or uneven surfaces, such as concrete or uneven terrain, can increase the impact on the lower limbs, contributing to the development of shin splints.
6. Muscle Weakness or Imbalance
Weakness or imbalance in the muscles of the lower leg, particularly the calf muscles and anterior tibialis, can impair shock absorption and stability, predisposing individuals to shin splints.
By understanding these underlying causes, athletes can implement preventive measures and effectively manage shin splints for sustained performance and well-being.
Identifying the Causes of Stress Fractures
Stress fractures, frequently seen in athletes, stem from multiple factors. Overuse, sudden training intensity changes, and biomechanical issues like flat feet contribute to their occurrence. Poor bone density and nutritional deficiencies also heighten the risk. Recognizing these causes is crucial for prevention and management in athletes.
1. Overuse and Repetitive Stress
Like shin splints, stress fractures often result from repetitive stress and overuse of the bones in the lower extremities. Activities involving repetitive pounding or impact, such as running, jumping, or gymnastics, can lead to microfractures in the bones over time.
2. Sudden Increase in Training Intensity
A rapid escalation in training intensity, duration, or frequency without adequate rest or recovery periods can overwhelm the body's ability to repair and remodel bone tissue, increasing the risk of stress fractures.
3. Poor Bone Density
Individuals with low bone density, such as those with osteoporosis or osteopenia, are more susceptible to stress fractures as their bones are less resilient to repetitive stress.
4. Biomechanical Factor
Structural abnormalities or biomechanical issues, such as flat feet, high arches, leg length discrepancies, or improper gait mechanics, can alter the distribution of forces along the lower limbs, predisposing certain bones to stress fractures.
5. Inadequate Nutrition
Nutritional deficiencies, particularly in calcium and vitamin D, can weaken bones, making them more susceptible to stress fractures. Proper nutrition is essential for maintaining bone health and integrity.
6. Female Athlete Triad
In female athletes, the triad of disordered eating, amenorrhea (absence of menstruation), and osteoporosis can significantly increase the risk of stress fractures due to hormonal imbalances and decreased bone density.
Understanding these underlying causes is crucial for implementing preventive strategies and designing effective treatment and rehabilitation plans for individuals with shin splints and stress fractures.
By addressing contributing factors and modifying training regimens accordingly, athletes can reduce their risk of these debilitating injuries and optimize their overall performance and well-being.
Common Symptoms of Shin Splints
Shin splints and stress fractures present distinct sets of symptoms, both commonly affecting athletes engaged in high-impact activities. Shin splints typically manifest as pain along the shinbone during or after exercise, accompanied by tenderness and swelling.

1. Pain Along the Shinbone
The primary symptom of shin splints is pain along the inner edge of the shinbone (tibia).
2. Pain During or After Activity
Pain typically develops during or after physical activity, particularly running, jumping, or other high-impact exercises.
3. Tenderness and Swelling
Tenderness and swelling may be present along the shinbone, often accompanied by mild to moderate swelling.
4. Dull or Aching Pain
The pain associated with shin splints is often described as dull, aching, or throbbing in nature.
5. Pain Alleviated by Rest
Symptoms may improve with rest but can worsen upon resuming activity.
Recognizing these symptoms is crucial for early intervention and effective management of shin splints. If experiencing persistent or worsening pain, it is essential to seek medical evaluation for proper diagnosis and treatment.
Common Symptoms of Stress Fractures
In contrast, stress fractures exhibit localized pain in specific areas of the lower leg or foot, worsening with activity and often accompanied by swelling and tenderness. Understanding these characteristic symptoms is crucial for accurate diagnosis and appropriate management of these common lower limb injuries in athletes.
1. Localized Pain
Stress fractures cause localized pain in a specific area of the affected bone, typically the lower leg or foot.
2. Pain Worsens with Activity
Pain tends to worsen during weight-bearing activities, such as walking, running, or jumping, and may subside with rest.
3. Swelling and Tenderness
Swelling, tenderness, and bruising may be present over the site of the stress fracture.
4. Pain at Night
Pain may persist even at rest, and individuals may experience increased discomfort, particularly at night.
5. Sudden Onset of Severe Pain
In some cases, stress fractures may present with a sudden onset of severe pain, particularly with a direct impact or sudden increase in activity.
Recognizing these symptoms is crucial for early diagnosis and timely intervention to prevent further complications and facilitate optimal recovery in individuals with shin splints and stress fractures.
Preventing Shin Splints and Stress Fractures in Athletes
Shin splints and stress fractures are often preventable with proper attention to training techniques, equipment, and lifestyle factors. Effective prevention strategies can significantly reduce the risk of these injuries in athletes. Below are guidelines for preventing shin splints and stress fractures:
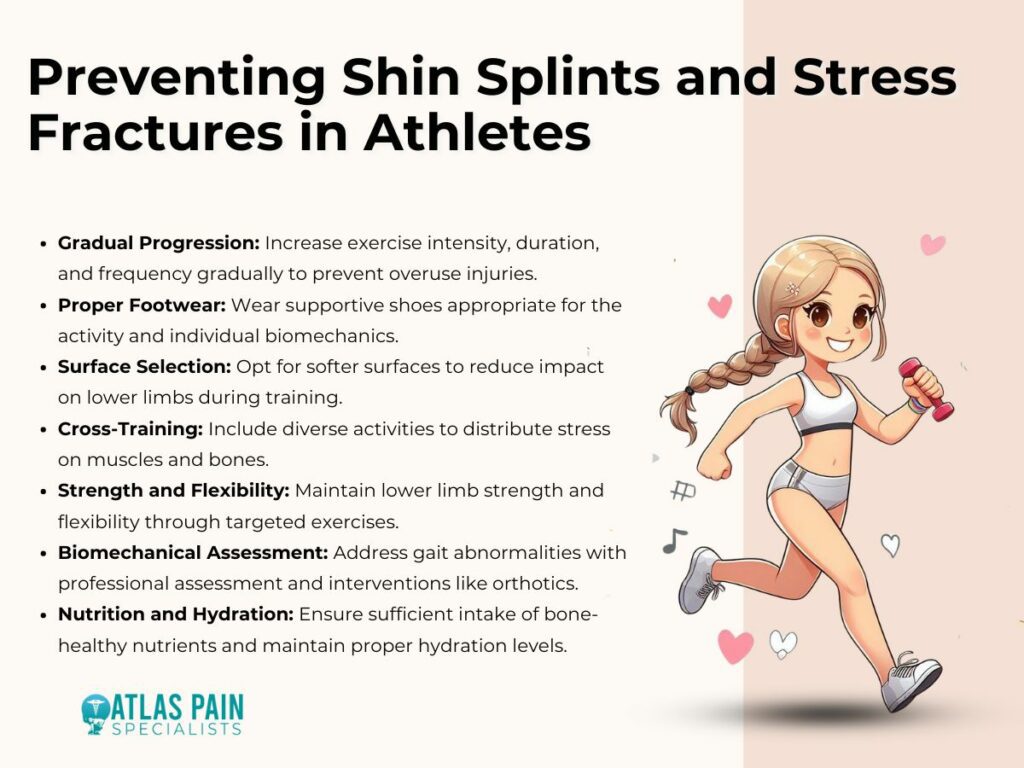
1. Gradual Progression
Gradually increase the intensity, duration, and frequency of exercise to allow the body to adapt and minimize the risk of overuse injuries.
2. Proper Footwear
Wear appropriate footwear with adequate support and cushioning, suitable for the specific activity and individual biomechanics.
3. Surface Selection
Choose softer, even surfaces for training whenever possible to reduce the impact on the lower limbs.
4. Cross-Training
Incorporate cross-training activities to diversify the stress on muscles and bones, reducing the risk of overuse injuries.
5. Strength and Flexibility
Maintain good lower limb strength and flexibility through targeted exercises, focusing on the calf muscles, anterior tibialis, and surrounding musculature.
6. Biomechanical Assessment
Identify and address biomechanical abnormalities or gait issues through professional assessment and appropriate interventions, such as orthotics or gait retraining.
7. Nutrition and Hydration
Ensure adequate intake of nutrients essential for bone health, including calcium, vitamin D, and magnesium, and maintain proper hydration levels.
Treatment Strategies for Shin Splints and Stress Fractures
Effective treatment strategies for shin splints and stress fractures are crucial for athletes aiming to recover swiftly and return to their sport. Treatment typically involves a combination of rest, pain management, rehabilitation exercises, and addressing underlying factors contributing to the injuries. Timely intervention and adherence to treatment protocols are essential to ensure optimal recovery outcomes and prevent long-term complications.
1. Rest
Rest the affected limb to allow for healing and alleviate symptoms. Avoid activities that exacerbate pain until symptoms resolve.
2. Ice and Compression
Apply ice packs and use compression wraps to reduce pain and inflammation, particularly during the acute phase of injury.
3. Pain Management
Over-the-counter pain relievers such as ibuprofen or acetaminophen may help alleviate discomfort associated with shin splints and stress fractures.
4. Stretching and Strengthening
Perform gentle stretching exercises for the calf muscles, Achilles tendon, and anterior tibialis to improve flexibility and prevent muscle imbalances. Gradually incorporate strengthening exercises to enhance muscle stability and support.
5. Physical Therapy
Seek guidance from a physical therapist for personalized rehabilitation programs focusing on restoring function, addressing biomechanical issues, and preventing recurrence.
6. Orthotics and Supportive Devices
Consider using orthotic inserts or supportive devices, such as braces or splints, to provide additional stability and cushioning during activity.
7. Gradual Return to Activity
Once symptoms improve, gradually reintroduce activity, starting with low-impact exercises and gradually progressing to higher-intensity activities.
8. Medical Evaluation
Consult with a healthcare professional if symptoms persist or worsen despite conservative measures, as further evaluation may be necessary to rule out underlying conditions or complications.
By implementing these preventive measures and appropriate treatment strategies, athletes can effectively manage shin splints and stress fractures, minimize downtime, and safely return to their sport or activity with reduced risk of recurrence.
However, it's essential to listen to your body, seek professional guidance when needed, and prioritize long-term musculoskeletal health and injury prevention.
Summary
In summary, understanding the nuances between shin splints and stress fractures is vital for athletes and sports enthusiasts alike. Both injuries, though distinct in nature, share commonalities in terms of causes, symptoms, prevention, and treatment.
By recognizing the signs early, implementing preventive measures, and seeking timely intervention, individuals can mitigate the risk of these debilitating conditions and facilitate optimal recovery. To sustain participation in sports and activities while safeguarding overall well-being, it is imperative to prioritize long-term musculoskeletal health through proper training techniques, adequate rest, and injury prevention strategies.
With a proactive approach to injury management and a focus on comprehensive rehabilitation, athletes can continue pursuing their passions with confidence and resilience, maximizing their potential and enjoyment in sports and physical endeavors.
About Dr. Sean Ormond