
9 Questions You Should Ask a Pain Management Doctor During Consultation
Pain management is a specialized field of medicine focusing on reducing pain and improving quality of life through an integrated approach. If you're suffering from chronic pain, a pain management doctor can help devise a personalized treatment plan to alleviate your symptoms.
However, to ensure that you understand your condition and treatment options, there are several key questions you should consider asking your pain management doctor. Whether you're new to the world of pain management or have been navigating it for a while, these questions can guide your conversations with your doctor, ensuring you gain the maximum benefit from your consultation.
Let's delve into these questions and understand why they are important and how their answers can shape your pain management journey.
- What is the Likely Cause of My Pain?
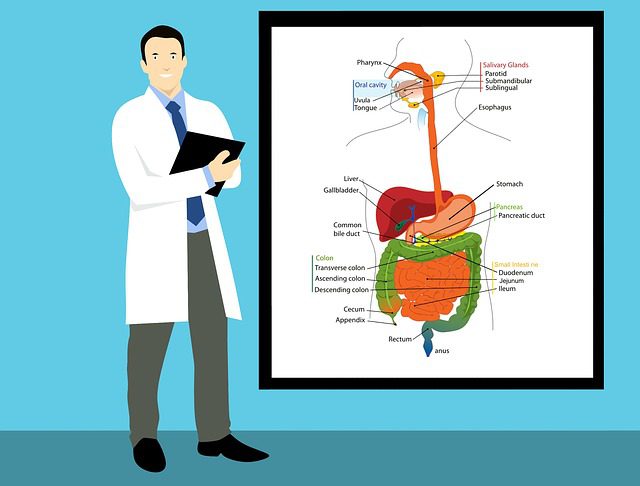
Understanding the source of your pain is crucial to treating it effectively. Pain can be caused by a variety of factors, such as injuries, illnesses, diseases, or conditions, and even mental health issues.
It's essential to ask your pain management doctor about what could be causing your pain, as it can help both of you devise an appropriate treatment plan.
Here's why this question is important:
- Correct Diagnosis: Pain is a symptom, not a disease. It usually indicates an underlying problem. Identifying the exact cause can lead to a more accurate diagnosis and thus, a more effective treatment plan.
- Effective Treatment: Different types of pain require different types of treatments. For instance, pain caused by a muscular injury might be treated with physical therapy and pain relievers, while pain caused by nerve damage might require different medications or interventions.
- Prevent Further Complications: In some cases, pain can be a sign of a serious condition that needs immediate attention. By identifying the cause of your pain early, you could prevent further complications.
- Personalized Care: Understanding your pain's cause helps your doctor tailor your treatment plan according to your specific needs, increasing the chances of successful pain management.
- Proactive Management: If your pain is caused by a chronic condition, knowing the cause can help you manage your symptoms proactively and prevent pain flare-ups.
When asking your pain management doctor about the likely cause of your pain, also inquire about any necessary tests or investigations that might be needed to confirm the diagnosis. These could include imaging tests like X-rays, MRIs, nerve conduction studies, or even blood tests. Remember, understanding your pain is the first step toward managing it effectively.
- What are My Treatment Options?
When it comes to managing chronic pain, numerous treatment options are available, and it's crucial to discuss these with your pain management doctor. Each treatment has its benefits, risks, and mode of action, and your doctor will recommend a plan based on your specific condition, lifestyle, and overall health.
Here's why this question is important:
- Personalized Treatment Plan: Understanding the available treatments can help you and your doctor create a personalized pain management plan. This could range from medications and physical therapy to more invasive procedures like surgery or nerve blocks.
- Informed Decision-Making: Knowing your treatment options helps you make informed decisions about your health. By understanding each treatment's potential benefits, risks, and side effects, you can choose the one that best aligns with your lifestyle, needs, and comfort level.
- Setting Realistic Expectations: Asking about treatment options can help set realistic expectations about the process and results. Some treatments may provide immediate relief, while others may require more time to show results.
- Exploring Alternatives: If the first-line treatment doesn't yield the desired results, knowing about alternative treatments can help guide the next steps.
Typical treatment options for chronic pain include:
- Medications: This could range from over-the-counter pain relievers and anti-inflammatory drugs to prescription medications such as opioids, antidepressants, or anticonvulsants.
- Physical Therapy: Techniques such as massage, heat, cold therapy, and exercises can help relieve pain and improve physical function.
- Behavioral Therapy: Cognitive-behavioral therapy and other psychological approaches can help you cope with pain and improve your quality of life.
- Interventional Procedures: These include nerve blocks, spinal cord stimulation, and injections, among others.
- Alternative Therapies: Techniques like acupuncture, chiropractic treatment, and biofeedback might also be beneficial.
The goal of pain management is not just to relieve pain but also to improve function and quality of life. So, it's essential to discuss all possible treatment options with your doctor and choose the one that suits you best.
- What are the Risks and Benefits of These Treatments?
Asking your pain management doctor about the risks and benefits of your potential treatments is critical in making informed decisions about your health care. Every treatment approach has potential advantages and disadvantages, and understanding these can help you choose the treatment that best aligns with your lifestyle, needs, and comfort level.
Here's why this question is important:
- Informed Decision Making: Knowing the risks and benefits allows you to make an informed decision about your treatment. This can also give you a better understanding of what to expect from the treatment process.
- Risk-Benefit Analysis: Understanding the benefits and risks of each treatment option helps you weigh the pros and cons. You can then opt for the treatment that provides the most benefit with the least risk.
- Preparation for Side Effects: Being aware of the possible risks or side effects of treatment will prepare you to recognize them if they occur and take appropriate action.
- Improved Compliance: When you understand why a particular treatment has been recommended and what it entails, you're more likely to follow the treatment plan.
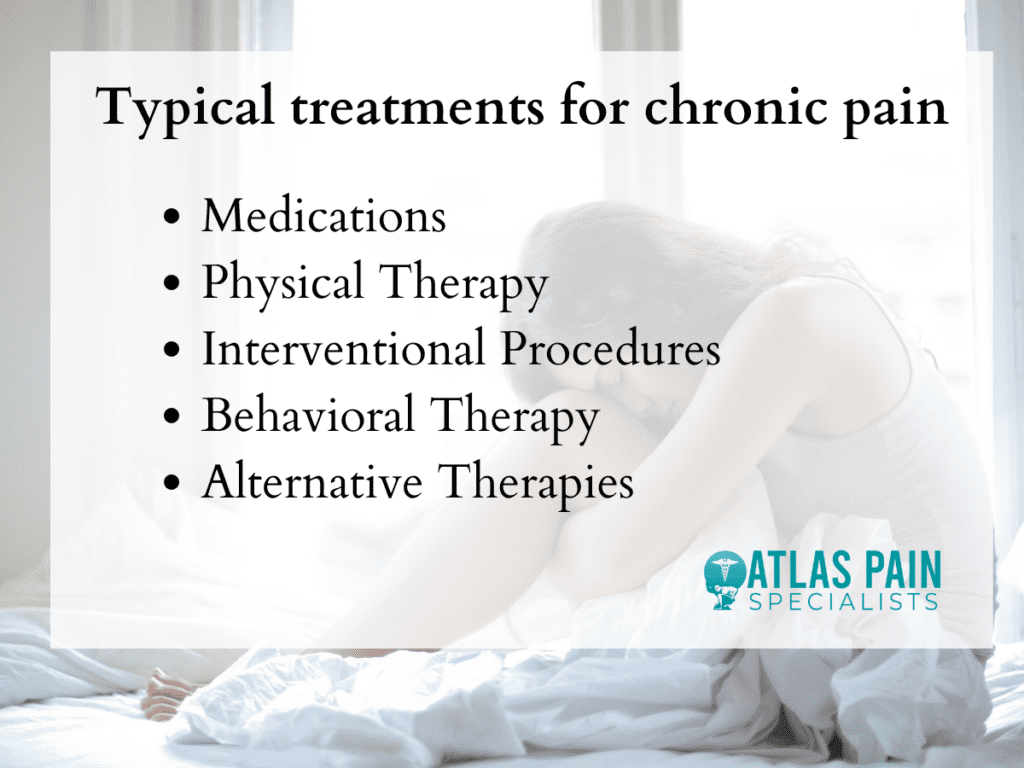
Typical treatments for chronic pain and their potential risks and benefits include:
- Medications: Medications can provide quick relief from pain, but they also carry risks such as side effects, allergic reactions, and the potential for dependency or addiction, especially with long-term use.
- Physical Therapy: Physical therapy can help improve mobility and function and reduce pain without the use of drugs. However, it requires commitment and may increase discomfort before improvements are made.
- Interventional Procedures: Procedures such as injections or nerve blocks can provide significant pain relief. However, they can also have risks such as infection, bleeding, or nerve damage.
- Behavioral Therapy: Behavioral therapies like cognitive-behavioral therapy can improve coping skills and reduce the perceived severity of pain, but they require active participation and may take time to show results.
- Alternative Therapies: Techniques like acupuncture or chiropractic care may help some patients, but their effectiveness varies from person to person. There's also a risk of complications if performed improperly.
The goal of treatment is to reduce pain and improve your overall quality of life. By understanding the risks and benefits of each treatment option, you can work with your doctor to devise a treatment plan that suits your specific needs and circumstances.
- What is the Goal of My Treatment Plan?
Asking your pain management doctor about the goal of your treatment plan is a crucial aspect of your healthcare journey. A clear understanding of what you and your doctor hope to achieve can help set realistic expectations, track your progress, and ensure that you're both working towards the same outcome.
Here's why this question is important:
- Setting Realistic Expectations: Knowing the goal of your treatment can help you understand what to expect from the treatment process. It can help you prepare mentally and emotionally for the journey ahead.
- Patient-Doctor Alignment: Ensuring that you and your doctor share the same treatment objectives is vital for the success of your treatment. It ensures both parties are working towards a common goal.
- Tracking Progress: A clear treatment goal can help you and your doctor measure progress and determine if the treatment is effective or if changes need to be made.
- Motivation and Compliance: When you understand the end goal of your treatment, you're likely to be more motivated to follow the treatment plan and more compliant with your doctor's instructions.
The goal of a pain management plan can vary greatly depending on your condition, severity of pain, overall health, and personal circumstances. Common goals for pain management can include:
- Pain Reduction: The primary goal of most treatment plans is to reduce the severity of pain. This can lead to a significant improvement in quality of life.
- Improved Function: For many, the goal is to increase functionality - to be able to perform daily activities with less pain and discomfort.
- Better Quality of Life: This could mean improved sleep, increased ability to work or participate in social activities, or greater well-being.
- Reduced Dependence on Medications: For some, especially those who've been on pain medications for a long time, an important goal might be reducing reliance on these drugs.
- Managing Flare-ups: Learning to manage episodes of severe pain, also known as flare-ups, can be a critical goal.
Overall, the best treatment goal is realistic, achievable, and aligned with your personal needs and lifestyle. Always discuss your treatment goals with your doctor to ensure that your pain management plan is tailored to suit your specific circumstances.
- What Lifestyle Changes Can Assist in Pain Management?
Lifestyle changes can often play a significant role in pain management. They can help improve your overall health, enhance the effectiveness of your treatments, and even reduce the severity of your pain.
Here's why this question is important:
- Improved Overall Health: Lifestyle changes often involve adopting healthier habits, which can enhance your overall health and well-being, making you more resilient and better able to cope with pain.
- Enhanced Treatment Effectiveness: Certain lifestyle changes can complement your medical treatments, making them more effective.
- Self-management Strategies: Lifestyle modifications can serve as self-management strategies that give you more control over your pain and life.
- Prevention of Further Issues: Healthy habits can also help prevent other health issues that could worsen your pain.
Some lifestyle changes that can assist in pain management include:
- Physical Activity
- Healthy Diet
- Stress Management
- Adequate Sleep
- Quitting Smoking
- Limit Alcohol
- Support Groups
It's important to discuss any potential lifestyle changes with your doctor, as not all changes may be suitable for everyone, and some may even have risks. Remember, lifestyle changes should complement your medical treatment, not replace it. Your doctor can guide you on incorporating these changes safely and effectively into your pain management plan.
- How Will We Measure Progress?
Measuring progress is a vital part of managing chronic pain. It can help you and your doctor understand if your treatment plan is working or if adjustments need to be made.
Here's why this question is important:
- Assessing Treatment Effectiveness: Regularly measuring progress can help determine if your current treatment is effective or if a different approach is needed.
- Motivation: Seeing measurable improvement can provide motivation and hope, both of which are crucial in managing chronic pain.
- Adjusting Treatment: Monitoring progress allows your doctor to make necessary adjustments to your treatment plan, ensuring it remains suited to your needs.
Different ways to measure progress in pain management include:
- Pain Scales: These are tools that help you rate your pain on a numerical or visual scale. They can provide a consistent method to express how you're feeling.
- Pain Diaries: Keeping a regular record of your pain, its triggers, and how it affects your daily activities can provide a clearer picture of your progress over time.
- Functional Assessment: This might involve assessing your ability to perform certain tasks or activities that were difficult for you due to pain.
- Sleep Quality: As chronic pain often affects sleep, improving sleep quality can be a sign of progress.
- Emotional Well-being: Chronic pain can also affect your mental health. An improvement in your mood or emotional well-being can indicate progress.
- Reduction in Medication Usage: If you can manage your pain with less medication, this can be a sign that your condition is improving.
- Patient-reported Outcomes: These are reports directly from you about how you feel and function. They can include pain, fatigue, physical function, mood, and quality of life.
Remember, progress might be slow, and there may be setbacks along the way. The goal is an overall improvement over time, not necessarily immediate results. Regularly discuss your progress with your doctor to ensure your treatment plan meets your needs.
- What Happens If the Treatment Doesn't Work?
Discussing a contingency plan with your pain management doctor is crucial. Understanding what steps will be taken if a treatment doesn't work can provide peace of mind and prepare you for different outcomes. Here's why this question is important:
- Plan B: Knowing that other options are available if a particular treatment doesn't work can alleviate anxiety about the future.
- Continuity of Care: This question ensures that your care continues seamlessly, even if a treatment fails to provide the desired results.
- Informed Decision-Making: Understanding the next steps can help you make informed decisions about your care and treatment.
If a treatment doesn't work as expected, your doctor may consider several options:
- Adjusting the Treatment Plan: Sometimes, making changes to the dosage, frequency, or method of administration can improve the effectiveness of treatment.
- Switching Treatments: If the current treatment isn't working, your doctor may suggest trying a different treatment. This could be a different medication, an alternative therapy, or a different type of intervention.
- Combining Treatments: Sometimes, combining treatments can provide better results than a single treatment. This is often referred to as a multimodal approach.
- Referral to a Specialist: If your pain is complex or difficult to manage, your doctor might refer you to a specialist with advanced training in managing your specific type of pain.
- Exploring Clinical Trials: If standard treatments aren't effective, you might be a candidate for clinical trials testing new pain management interventions or drugs.
Pain management often requires a trial-and-error approach. What works well for one person might not work as well for another. It's important to maintain open communication with your doctor, provide feedback on what's working and what's not, and stay informed about your treatment options. This will ensure that your treatment plan continues to evolve with your needs.
- How Can I Manage Pain Flare-ups?
Managing pain flare-ups, or periods when your pain suddenly becomes more intense, is an important part of chronic pain management. These episodes can be triggered by various factors such as stress, physical activity, weather changes, or even for no apparent reason.
Here's why this question is important:
- Improved Coping Skills: Knowing how to handle a pain flare-up can improve your ability to cope with these challenging episodes and reduce their impact on your life.
- Self-Management: Understanding flare-up management gives you more control over your pain and can help reduce anxiety and fear associated with these episodes.
- Prevention: Learning about triggers and early signs of a flare-up can help you take preventive measures to reduce their frequency or severity.
Some strategies to manage pain flare-ups include:
- Medication: Your doctor may prescribe certain medications to be taken at the onset of a flare-up.
- Relaxation Techniques: Deep breathing, progressive muscle relaxation, or guided imagery can help reduce tension and alleviate pain during a flare-up.
- Heat or Cold Therapy: Applying heat or cold to the affected area can help soothe the pain. Always remember to use a barrier like a cloth between your skin and the heat or cold source to avoid injury.
- Distraction: Doing an activity that distracts your mind from the pain, such as reading, listening to music, or watching a movie, can sometimes help during a flare-up.
- Rest: Resting during a flare-up can help your body recover. However, prolonged bed rest can have negative effects, so finding a balance is important.
- Pacing: Learning to pace your activities can prevent overexertion and potential flare-ups. Break tasks into manageable parts, take regular breaks, and listen to your body's signals.
Everyone is different, and what works for one person might not work for another. It's essential to discuss flare-up management with your doctor and create a personalized plan that suits your specific needs and circumstances. This can help you feel more prepared and in control when a flare-up occurs.
9. How Will My Pain Condition Affect My Overall Health?
Asking your pain management doctor about how your pain condition might affect your overall health is critical to understanding and managing your health. Chronic pain can impact your health and well-being, from physical fitness to emotional stability.
Here's why this question is important:
- Comprehensive Understanding: Knowing how your pain condition can impact your overall health can give you a more comprehensive understanding of your condition and its potential implications.
- Proactive Management: Understanding the potential impact can help you take proactive steps to minimize these effects and maintain your overall health.
- Holistic Approach: This question can encourage a more holistic approach to your healthcare, considering your pain and overall well-being.
Chronic pain can affect your overall health in several ways:
- Physical Health: Chronic pain can limit your physical activities and lead to a sedentary lifestyle, increasing the risk of conditions like obesity, heart disease, and diabetes. Pain can also disrupt your sleep, which can have numerous negative health effects.
- Mental Health: Chronic pain is linked to mental health conditions such as depression, anxiety, and stress disorders. Living with constant pain can be emotionally draining and affect your mood and outlook.
- Social Health: Pain can affect your ability to work, engage in social activities, or maintain relationships, which can lead to social isolation and impact your quality of life.
- Medication Side Effects: Some medications used for pain management can have side effects, such as constipation, drowsiness, or risk of dependency, which can affect your overall health.
- Co-existing Conditions: Chronic pain can exacerbate other health conditions you might have, and vice versa. For example, stress from pain can worsen conditions like hypertension or asthma.
Understanding the potential impact of your pain condition on your overall health can guide you and your doctor in devising a comprehensive pain management plan. This plan can include strategies to mitigate these effects. Remember, your pain management should encompass all aspects of your health for optimal results.
Conclusion
Managing chronic pain can be a complex and daunting task. It's a journey often marked by numerous consultations, different treatment options, and a series of trials and errors. Central to this journey is your relationship with your pain management doctor, a specialist trained to diagnose and treat pain.
During your consultation, asking the right questions is essential to fully understand your condition, treatment options, and what you can expect from your pain management plan. These questions can help you make informed decisions, set realistic expectations, and actively participate in your care. Remember, it's your right as a patient to understand your condition, treatment options, and the potential impact on your life.
About Dr. Sean Ormond