Pain Management for Chronic Kidney Disease: Considerations and Support
Chronic Kidney Disease (CKD) affects millions worldwide, with pain being a significant and often overlooked aspect of the condition. Managing pain in CKD patients presents unique challenges due to various factors, including the prevalence and impact of pain, types of pain experienced, and physiological changes that affect pain management.
In this article, we look pain management for CKD patients and explore strategies to address their needs effectively. Let's look at pain management for chronic kidney disease.
Understanding Pain in CKD Patients
Pain is a prevalent and distressing symptom in CKD patients, significantly impacting their quality of life and overall well-being. Chronic pain can stem from various sources, including neuropathic, nociceptive, and musculoskeletal origins.
Below are types of pain experienced by CKD Patients:
- Neuropathic Pain: CKD patients commonly experience neuropathic pain due to nerve damage resulting from the disease process. This type of pain is often described as burning, tingling, or shooting sensations and can be challenging to manage.
- Nociceptive Pain: Nociceptive pain in CKD patients can arise from tissue damage or inflammation, such as kidney stones or renal cysts. It is typically localized and described as dull, aching, or cramping.
- Musculoskeletal Pain: CKD patients may also experience musculoskeletal pain due to abnormalities in bone metabolism, osteoarthritis, or muscle cramps associated with electrolyte imbalances.
Below are factors contributing to pain in CKD Patients
- Comorbidities: CKD patients often have comorbid conditions such as diabetes, hypertension, and cardiovascular disease, which can exacerbate pain symptoms.
- Medications: Certain medications used to manage CKD-related complications, such as erythropoiesis-stimulating agents (ESAs) or phosphate binders, may contribute to pain or discomfort as side effects.
- Fluid and Electrolyte Imbalances: Fluctuations in fluid and electrolyte levels characteristic of CKD can lead to muscle cramps, nerve irritation, and other sources of pain.
Challenges in Pain Management for CKD Patients
Managing pain in CKD patients poses several challenges due to the physiological changes and complications associated with the disease.
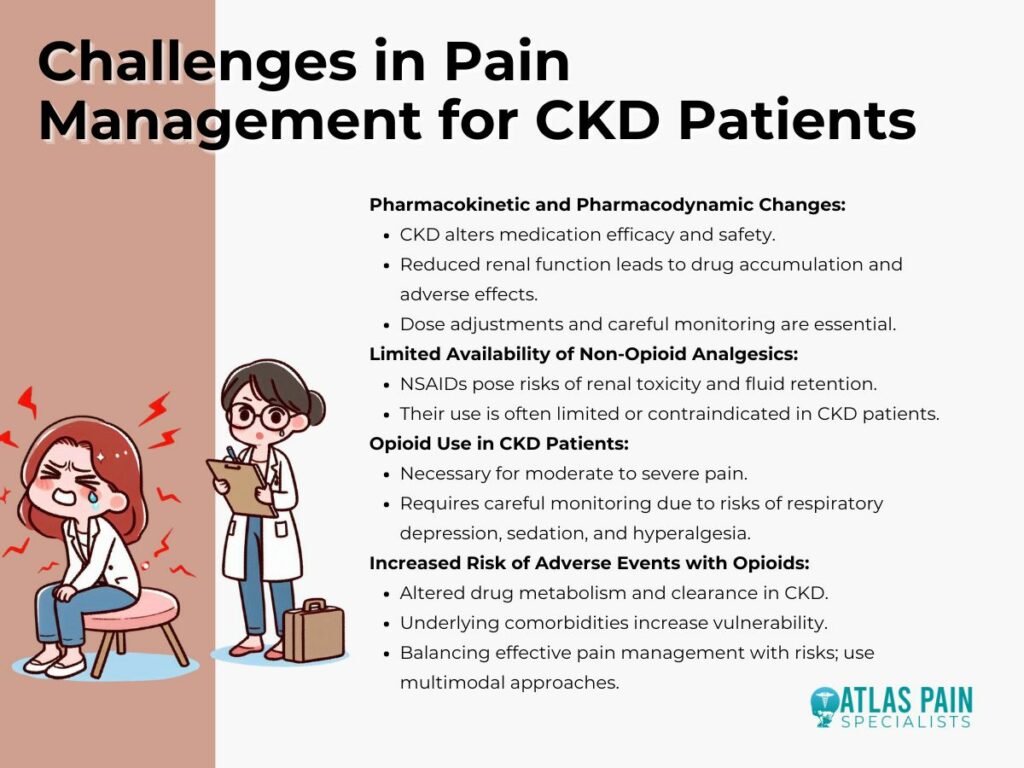
- Pharmacokinetic and Pharmacodynamic Changes in CKD Patients: CKD alters the pharmacokinetics and pharmacodynamics of many medications, affecting their efficacy and safety profiles. Reduced renal function can lead to drug accumulation and increased susceptibility to adverse effects, necessitating dose adjustments and careful monitoring.
- Limited Availability of Non-Opioid Analgesics and Opioid Use in CKD Patients: Non-opioid analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to manage pain but pose risks of renal toxicity and fluid retention, particularly in CKD patients. As a result, their use is often limited or contraindicated, leaving fewer options for pain relief.
- Opioid therapy may be necessary for managing moderate to severe pain in CKD patients, but it requires careful consideration and monitoring due to the increased risk of adverse events, including respiratory depression, sedation, and opioid-induced hyperalgesia.
- Increased Risk of Adverse Events with Opioids in CKD Patients:CKD patients are particularly vulnerable to the adverse effects of opioids due to altered drug metabolism and clearance, as well as underlying comorbidities. Concerns regarding opioid misuse and addiction further complicate their use in this population. Healthcare providers must balance the need for effective pain management with the risks associated with opioid therapy, opting for judicious prescribing and multimodal approaches whenever possible.
Non-Pharmacological and Non-Opioid Analgesic Options
Managing pain in Chronic Kidney Disease (CKD) patients necessitates a multifaceted approach that extends beyond pharmacological interventions. Non-pharmacological therapies and non-opioid analgesics play crucial roles in alleviating pain and improving quality of life for individuals with CKD.
Physical Activity and Other Non-Pharmacological Therapies for Pain Management
Physical activity, including aerobic exercises, stretching, and strength training, can effectively reduce pain and improve physical function in CKD patients. Regular exercise promotes muscle strength, joint flexibility, and cardiovascular health, which can mitigate musculoskeletal pain and enhance overall well-being.
In addition to physical activity, various non-pharmacological therapies offer complementary benefits for pain management in CKD patients:
- Heat and Cold Therapy: Applying heat packs or cold compresses to painful areas can provide temporary relief by reducing inflammation, soothing muscle spasms, and numbing nerve endings.
- Transcutaneous Electrical Nerve Stimulation (TENS): TENS therapy involves the use of low-voltage electrical currents to disrupt pain signals, offering non-invasive pain relief for CKD patients.
- Massage Therapy: Massage techniques, such as gentle kneading or targeted pressure, can promote relaxation, improve circulation, and alleviate muscle tension and discomfort.
Non-Opioid Analgesics and Their Use in CKD Patients
Non-opioid analgesics play a crucial role in managing mild to moderate pain in CKD patients while minimizing the risk of renal toxicity and adverse effects associated with NSAIDs. Common non-opioid analgesics used in CKD patients include:
- Acetaminophen (Paracetamol): Acetaminophen is a first-line analgesic for CKD patients due to its minimal impact on renal function. However, careful dosing is essential to avoid hepatotoxicity, particularly in patients with liver impairment or co-existing conditions.
- Topical Analgesics: Topical agents such as lidocaine patches or capsaicin creams can provide localized pain relief without systemic absorption, making them suitable options for CKD patients with renal impairment.
Gabapentinoids, Serotonin-Norepinephrine Reuptake Inhibitors, and Tricyclic Antidepressants for Pain Management
Gabapentinoids, including gabapentin and pregabalin, are commonly prescribed for neuropathic pain in CKD patients. These agents modulate calcium channels in the central nervous system, reducing excitatory neurotransmitter release and dampening neuropathic pain signals. However, dose adjustments are necessary in CKD patients to prevent drug accumulation and potential toxicity.
Serotonin-norepinephrine reuptake inhibitors (SNRIs) such as duloxetine and tricyclic antidepressants (TCAs) like amitriptyline exhibit analgesic properties and are effective in managing neuropathic pain. These medications may also address associated symptoms of depression or anxiety, contributing to overall pain relief and improved quality of life for CKD patients.
Opioid Use in CKD Patients
Despite the risks associated with opioid therapy, judicious use of opioids may be necessary for managing moderate to severe pain in CKD patients, particularly when other treatment modalities have proven ineffective. However, selecting appropriate opioids and closely monitoring their use are essential considerations in this population.
Opioid Use in CKD Patients: Risks and Benefits
Opioids provide potent analgesia by binding to opioid receptors in the central nervous system, effectively modulating pain perception. However, CKD patients are at increased risk of adverse effects and complications associated with opioid therapy, including respiratory depression, sedation, constipation, and cognitive impairment.
Healthcare providers must weigh the potential benefits of opioid analgesia against these risks, considering individual patient factors and pain severity.
Opioids That Are Safer to Use in CKD Patients
Certain opioids exhibit favorable pharmacokinetic profiles and reduced reliance on renal clearance, making them safer options for CKD patients:
- Oxycodone: Oxycodone undergoes hepatic metabolism and is primarily excreted in the urine as metabolites, minimizing the risk of drug accumulation in CKD patients.
- Hydromorphone: Hydromorphone is primarily eliminated via hepatic metabolism, with minimal renal excretion, making it suitable for CKD patients with reduced renal function.
Buprenorphine as a Promising Option for Pain Management in CKD Patients
Buprenorphine, a partial mu-opioid receptor agonist, offers unique advantages for pain management in CKD patients. Its high binding affinity and slow dissociation from opioid receptors contribute to prolonged analgesic effects and reduced risk of respiratory depression compared to traditional opioids.
Buprenorphine's partial agonist activity also limits the potential for abuse and dependence, making it a promising option for long-term pain management in CKD patients requiring opioid therapy. However, dose adjustments and careful monitoring are necessary to optimize efficacy and safety in this population.
Best Practices for Pain Management in CKD Patients
Managing pain in Chronic Kidney Disease (CKD) patients requires a comprehensive and multidisciplinary approach that encompasses various strategies to optimize pain relief while minimizing risks and enhancing overall quality of life. Here, we outline best practices for pain management in CKD patients, focusing on a multidisciplinary approach, assessment and monitoring of pain, and patient education and expectation management.

Multidisciplinary Approach to Pain Management
A multidisciplinary team consisting of nephrologists, pain specialists, nurses, pharmacists, physical therapists, and other healthcare professionals plays a pivotal role in addressing the complex needs of CKD patients with chronic pain.
Collaborative care allows for a holistic assessment of pain, consideration of comorbidities and individual preferences, and implementation of multimodal treatment approaches tailored to each patient's unique circumstances. By drawing on the expertise of diverse healthcare professionals, the multidisciplinary team can provide comprehensive pain management that addresses physical, psychological, and social aspects of pain in CKD patients.
Assessment and Monitoring of Pain in CKD Patients
Regular assessment and monitoring of pain are essential components of effective pain management in CKD patients. Validated pain assessment tools, such as the Brief Pain Inventory (BPI) or the Numeric Rating Scale (NRS), can help quantify pain intensity, location, and impact on daily activities, facilitating ongoing evaluation of treatment effectiveness and adjustment of management strategies as needed.
Healthcare providers should be attentive to changes in pain patterns, comorbid conditions, and medication-related adverse effects, conducting thorough assessments to optimize pain relief while minimizing risks.
Patient Education and Expectation Management
Empowering CKD patients with knowledge about their condition, treatment options, and self-management strategies is critical for optimizing pain management outcomes. Patient education initiatives should emphasize the importance of adhering to prescribed medications, lifestyle modifications, and non-pharmacological interventions, while also addressing common misconceptions and concerns about pain management.
Healthcare providers should engage in open and honest discussions with patients about realistic expectations regarding pain relief, potential side effects of treatment modalities, and the importance of active participation in their care. By fostering a collaborative and transparent relationship with patients, healthcare providers can enhance treatment adherence, satisfaction, and overall well-being in CKD patients with chronic pain.
Conclusion
Effective pain management in Chronic Kidney Disease demands a tailored and comprehensive approach that integrates multidisciplinary care, rigorous assessment, and patient-centered education. By embracing evidence-based practices and fostering collaborative partnerships between healthcare providers and patients, we can navigate the complexities of pain in CKD, alleviate suffering, and promote holistic well-being for individuals living with this chronic condition
About Dr. Sean Ormond



