What Is the Next Step After a Medial Branch Block?
A medial branch block is a valuable diagnostic tool used to determine whether your chronic back or neck pain is originating from the facet joints. While the procedure itself provides only temporary relief, the real purpose is to guide the next steps in treatment.
By observing your body’s response, your healthcare provider can decide whether you're a good candidate for further interventions like radiofrequency ablation or if other sources of pain need to be investigated. Understanding what happens after the block is essential for creating an effective, personalized pain management plan.
Immediate Post-Procedure Evaluation (After a Medial Branch Block)
After receiving a medial branch block, the following hours are crucial in assessing its effectiveness. This procedure is primarily used to diagnose whether your back or neck pain originates from the facet joints. Here's how to evaluate your results effectively:
Track Your Pain Relief
Shortly after the procedure, usually within 15 to 30 minutes, you should begin to notice whether your pain improves. The local anesthetic used in medial branch blocks acts quickly, but its effects are temporary.
A significant drop in pain (typically 50% or more) is considered a positive response and may indicate that the facet joints are indeed the source of your pain.
Use a Pain Diary
Many clinics provide a pain diary for patients to use during the evaluation window. This tool allows you to log your pain levels, how long relief lasts, what kind of activities you attempt, and whether those activities trigger discomfort.
Accurate documentation helps your doctor better interpret the results and determine the most appropriate follow-up.
Test Normal Activities
After the block, you're encouraged to gently test movements that usually trigger pain, such as bending, walking, or twisting.
If you can perform these movements with noticeably less pain, it's a good sign that the block reached the intended nerves. This practical test helps validate whether the facet joints are the true source of pain.
Understand the Relief Window
It’s important to remember that medial branch blocks are not intended to provide long-term relief. If only a local anesthetic is used, pain relief may last a few hours.
Some injections include a corticosteroid, which might extend relief for a few days, but this is less common in strictly diagnostic procedures.
Communicate with Your Doctor
Your feedback is essential for planning next steps. Be open about the level of relief, the duration, and whether the pain returned fully or partially.
Based on this information, your physician may recommend proceeding to radiofrequency ablation for longer-lasting relief or suggest further diagnostic tests if the response was unclear or negative.
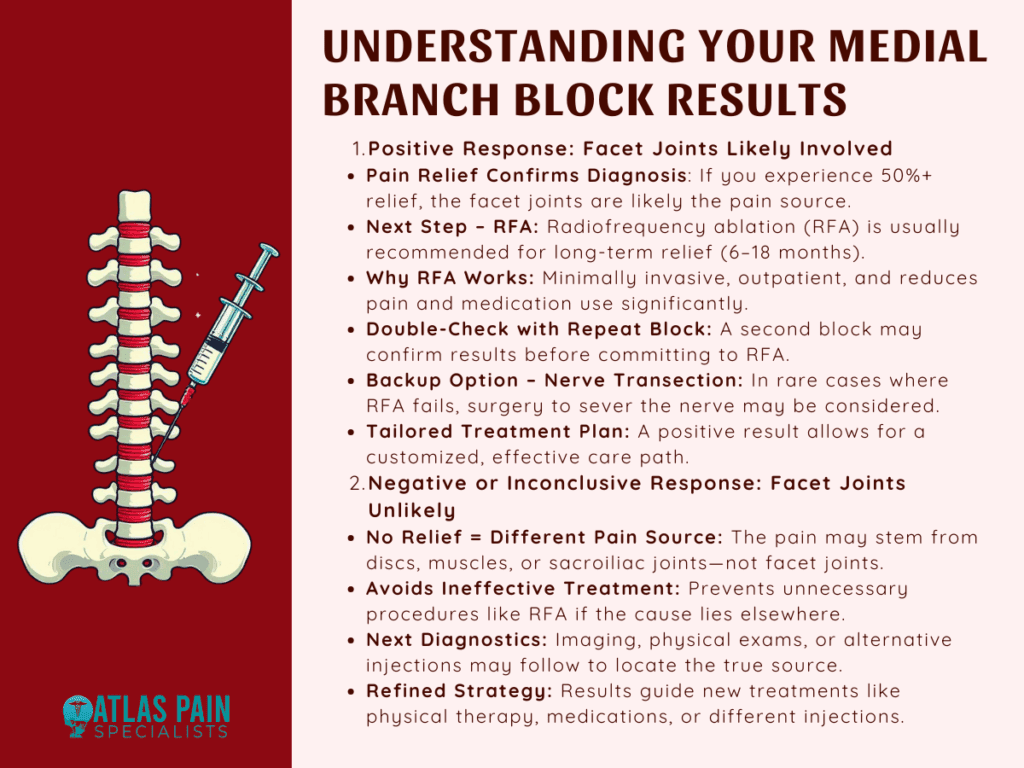
Positive Response to the Medial Branch Block
If you experience significant pain relief after a medial branch block, it’s considered a positive response, indicating that the facet joints are likely the source of your discomfort. This result provides valuable guidance for the next phase of treatment.
Confirmation of Facet Joint Involvement
A positive response typically means that the anesthetic successfully numbed the medial branch nerves, which supply the facet joints.
When pain relief is noticeable often 50% or more it confirms that these joints are contributing to your chronic back or neck pain. This diagnostic clarity helps narrow down treatment options and avoid unnecessary interventions.
Radiofrequency Ablation (RFA) as the Next Step
Radiofrequency ablation is commonly recommended following a successful medial branch block. This procedure targets the same medial branch nerves using controlled heat to disrupt their ability to transmit pain signals. Unlike the temporary relief offered by the block, RFA can provide longer-lasting results, often between 6 to 18 months.
Why RFA Is Often Preferred
RFA is minimally invasive, performed on an outpatient basis, and does not require general anesthesia.
It’s a logical next step when a medial branch block has provided temporary but significant relief. Many patients report a dramatic reduction in daily pain levels, improved mobility, and reduced reliance on pain medication after undergoing RFA.
Repeat Medial Branch Blocks for Confirmation
In some cases, a second medial branch block may be recommended before proceeding to RFA. This is done to confirm that the pain relief wasn't coincidental or influenced by external factors such as stress or placebo effect.
If pain relief is consistently achieved with both blocks, the likelihood of a successful RFA increases.
Alternative Option: Medial Branch Nerve Transection
Though less common, medial branch nerve transection surgery may be considered for patients who cannot undergo RFA or those for whom RFA fails to provide adequate relief.
This surgical option involves permanently severing the affected nerve, and it is typically reserved for severe cases where conservative measures have been exhausted.
Personalized Treatment Planning
A positive block result helps your physician tailor a treatment plan specific to your needs. Whether it's RFA, a combination of physical therapy and injections, or another minimally invasive procedure, the clarity gained from a successful block ensures you're not guessing about the source of your pain.
Negative or Inconclusive Response to the Medial Branch Block
If little to no pain relief is experienced following a medial branch block, this is considered a negative or inconclusive response. While this may feel discouraging at first, it actually provides important diagnostic information and helps redirect the treatment approach more accurately.
Facet Joints Likely Not the Pain Source
A lack of pain relief suggests that the facet joints are probably not responsible for the discomfort. Since medial branch blocks specifically target the nerves supplying these joints, an ineffective response means another structure such as spinal discs, sacroiliac joints, or muscles may be the true source of pain.
Importance of an Accurate Diagnosis
An inconclusive or negative result is not a failure; it prevents unnecessary treatments like radiofrequency ablation, which would not be effective if the facet joints are not involved. By ruling out facet-related pain, your healthcare provider can focus on exploring other potential causes more efficiently.
Next Steps in the Diagnostic Process
Following a negative response, your physician may recommend additional imaging studies such as MRI or CT scans, physical assessments, or alternative diagnostic injections. These tools help evaluate other spinal structures that may be contributing to your pain.
A multidisciplinary approach, involving pain specialists, physical therapists, or orthopedic experts, may be introduced to refine the diagnosis.
Guiding the Right Treatment Path
Even without a clear result from the block, your care team will use this outcome to shape a new treatment plan. This might include targeted physical therapy, different types of injections, medications, or exploring other minimally invasive procedures.
Medial Branch Block Procedure Overview
A medial branch block is a minimally invasive, outpatient procedure used to help diagnose and isolate the source of chronic spine-related pain. Specifically, it tests whether pain is coming from the facet joints, which are small joints located between each pair of vertebrae in the spine.
These joints allow movement and stability but can become inflamed or arthritic, leading to persistent neck or back pain. Understanding how the procedure works and what to expect can help patients feel more informed and prepared.
Purpose of the Procedure
Unlike other injections that are designed to treat pain, a medial branch block is diagnostic. It helps your doctor determine whether the medial branch nerves, which carry pain signals from the facet joints to the brain, are contributing to your symptoms.
If numbing these nerves significantly reduces your pain, it confirms that the facet joints are the likely source. This insight is crucial for deciding whether further treatment such as radiofrequency ablation is appropriate.
When It’s Used
Your doctor may recommend a medial branch block if you have chronic pain in the neck, mid-back, or lower back that hasn’t responded well to conservative treatments like physical therapy, medications, or massage. It is particularly useful in patients with pain that seems to originate from deeper joint structures rather than muscles or discs.
Procedure Setting and Timeframe
Medial branch blocks are typically performed in outpatient clinics, pain management centers, or ambulatory surgical facilities. They are relatively quick, often taking about 15 to 30 minutes to perform, with patients monitored for a short period afterward.
Since the procedure is non-surgical and does not require general anesthesia, you will be able to return home the same day.
Patient Preparation and Positioning
On arrival, you will be asked to change into a gown and lie face down on an X-ray table. The skin over the injection area will be cleaned with an antiseptic solution to prevent infection.
A local anesthetic is then used to numb the skin and underlying tissue, minimizing discomfort during needle insertion.
Imaging Guidance for Accuracy
The most critical part of the procedure is precise needle placement. To achieve this, your physician will use fluoroscopy (real-time X-ray) or ultrasound guidance to visualize the spine.
The imaging ensures that the needle is inserted near the small medial branch nerves that wrap around the facet joints. This step is essential for both safety and effectiveness.
Injection Process
Once the needle is in the correct position, the doctor injects a small amount of local anesthetic, and sometimes a steroid. The anesthetic temporarily blocks the nerve’s ability to transmit pain signals.
The steroid, when included, helps reduce any existing inflammation around the nerve or facet joint, although it is not always necessary for diagnostic purposes. Most patients begin to notice changes in pain within 10 to 15 minutes.
Monitoring and Activity Testing Post-Injection
After the injection, you will be observed for a short period, usually 15 to 30 minutes. During this time, your physician or nurse may ask you to perform movements or tasks that typically trigger your pain, such as walking, bending, or twisting.
The goal is to determine whether the injection has resulted in meaningful pain relief. This evaluation is essential in confirming whether the facet joints are involved.
Pain Diary and Follow-Up
You may be asked to keep a pain diary after leaving the facility. This diary should include details such as the timing, intensity, and duration of any pain relief you experience. The more specific your records, the easier it will be for your doctor to interpret the results and plan your next course of action.
Recovery and Side Effects
Because the procedure is minimally invasive and does not involve incisions or sutures, recovery is typically quick. Most patients return to their usual activities the same day or the next.
Some minor side effects can occur, such as temporary soreness or bruising at the injection site, mild dizziness, or numbness. These effects generally resolve within a few hours.
What Happens Next
If you experience significant, temporary pain relief, it suggests that your facet joints are the likely pain generators. Based on this result, your doctor may recommend radiofrequency ablation for longer-term relief. If there is no relief, further diagnostic evaluations will be considered to explore other sources of pain.
Everything You Need To Know About A Lumbar Medial Branch Block
If you’ve recently had a medial branch block or are considering one, understanding what comes next is just the beginning. Knowing whether the pain relief confirms facet joint involvement can shape your entire treatment plan. But what if the pain is located specifically in the lower back?
In our next blog, Everything You Need to Know About a Lumbar Medial Branch Block, we take a closer look at how this targeted procedure works in the lumbar spine, what to expect during recovery, and how it differs from other spinal injections. Continue reading to deepen your understanding and feel more prepared.
About Dr. Sean Ormond



