Managing Pain in Children: Approaches and Considerations
Managing pain in children is a complex and multifaceted task that requires a comprehensive approach. Recognizing the unique challenges associated with pediatric pain, a combination of pharmacological and non-pharmacological interventions tailored to individual needs is essential.
An interdisciplinary team—including physicians, nurses, therapists, and psychologists—plays a crucial role in providing holistic care. However, barriers such as underutilization of pediatric-specific tools, fear of adverse effects, and inadequate training hinder effective pain management. Addressing these challenges is vital for improving outcomes and ensuring children receive the best possible care.
Pain Assessment in Pediatrics
Timely and accurate pain assessment in pediatrics is crucial for effective diagnosis, management, and improving health outcomes. Pain, often considered the "fifth vital sign" significantly impacts a child's quality of life, physical and psychological well-being, and overall recovery from illness or injury.
However, assessing pain in children presents unique challenges due to age, cognitive development, and communication barriers. This necessitates a multifaceted approach utilizing both self-report tools and observational measures to accurately gauge pain levels.
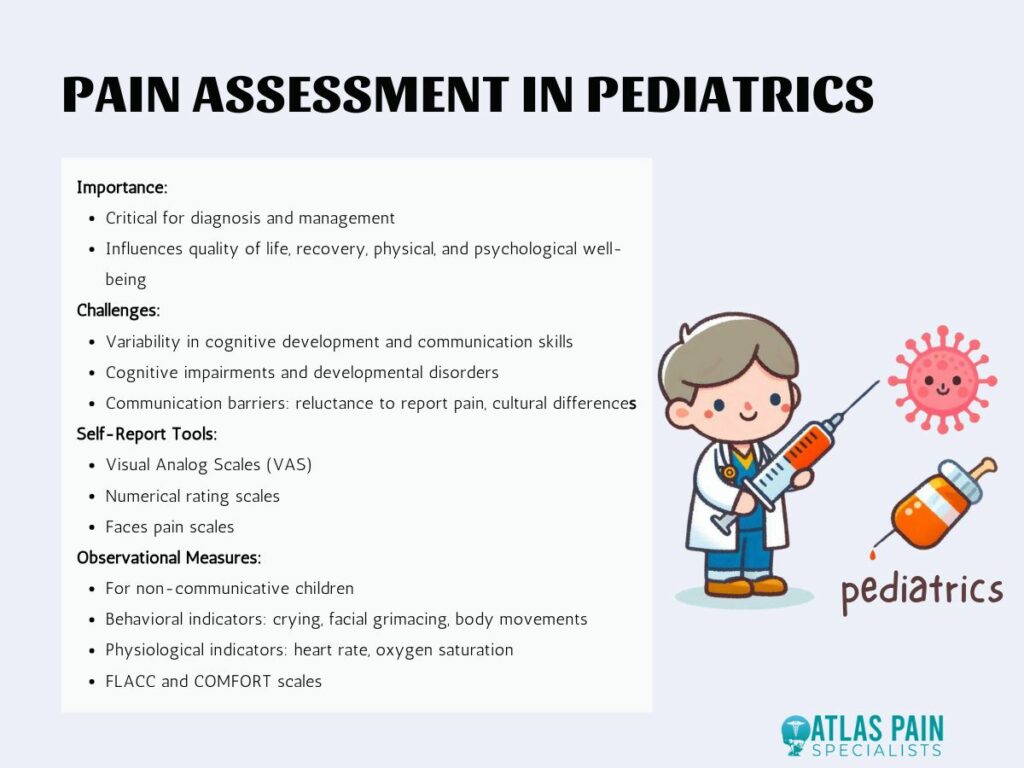
Challenges in Pediatric Pain Assessment
One of the primary challenges in pediatric pain assessment is the variability in cognitive development across different ages. Younger children, especially infants and toddlers, may lack the verbal skills to articulate their pain, while older children may not fully understand how to describe their pain intensity or quality.
Cognitive impairments and developmental disorders further complicate the assessment process, making it essential to tailor pain assessment tools to the child's developmental level and abilities.
Communication barriers are another significant hurdle. Children may be reluctant to report pain due to fear of medical procedures or a desire to please caregivers by appearing brave. Cultural differences can also influence pain expression and reporting, requiring healthcare providers to be culturally sensitive and aware of diverse pain communication styles.
Self-Report Tools
Self-report tools, such as visual analog scales (VAS), are effective in older children who can understand and reliably use these tools. The VAS involves a continuum of pain intensity levels, allowing children to mark their perceived pain on a scale, typically from "no pain" to "worst pain imaginable."
Other self-report tools include numerical rating scales and faces pain scales, which use facial expressions to represent varying levels of pain intensity, making them particularly useful for children who struggle with abstract concepts.
Observational Measures
For younger or non-communicative children, observational measures become indispensable. These measures assess pain based on behaviors such as crying, facial grimacing, and body movements, as well as physiological indicators like heart rate and oxygen saturation levels.
Tools like the FLACC (Face, Legs, Activity, Cry, Consolability) scale and the COMFORT scale are widely used to quantify pain in non-verbal children, providing a structured approach to interpreting behavioral and physiological pain signals.
Special Populations
Assessing pain in special populations, such as autistic children, requires unique considerations. Autistic children may have atypical pain responses and varied sensory processing, making traditional pain assessment tools less effective.
Healthcare providers must adapt their approach, often relying more heavily on caregiver reports and individualized observational strategies to ensure accurate pain assessment and management.
Pharmacological Pain Management
Pharmacological pain management in pediatrics is complex due to age-related differences in drug metabolism and clearance. These differences necessitate careful consideration of dosing and drug selection to avoid adverse effects while effectively managing pain.
A range of pharmacological options, including opioids, non-opioid analgesics, and adjuvant medications, are available for pediatric pain management, each with specific considerations for use in children.
Age-Related Differences in Drug Metabolism
Children's bodies process medications differently from adults, with variations in absorption, distribution, metabolism, and excretion that change with age. For instance, neonates and infants have immature liver enzymes and renal function, which can prolong the half-life of certain drugs, increasing the risk of toxicity.
As children grow, these metabolic pathways mature, altering the pharmacokinetics of medications and necessitating age-appropriate dosing adjustments.
Opioids and Non-Opioid Analgesics
Opioids, such as morphine and fentanyl, are potent analgesics used for moderate to severe pain in children. However, their use requires careful monitoring due to the risks of respiratory depression, sedation, and potential for abuse. Appropriate opioid stewardship involves using the lowest effective dose for the shortest duration necessary, combined with regular reassessment of pain and side effects.
Non-opioid analgesics, including acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, are often first-line treatments for mild to moderate pain. These medications are generally safer with fewer severe side effects than opioids but still require cautious use to avoid issues such as gastrointestinal irritation or liver toxicity, especially in chronic use.
Adjuvant Medications
Adjuvant medications, such as anticonvulsants and antidepressants, can enhance pain relief in certain conditions by targeting specific pain pathways. For example, gabapentin, an anticonvulsant, is effective in neuropathic pain management, while tricyclic antidepressants like amitriptyline can alleviate chronic pain syndromes. These medications are often used in conjunction with primary analgesics to optimize pain control.
Appropriate Opioid Stewardship
To address concerns of opioid abuse and adverse effects, healthcare providers must implement strict opioid stewardship practices. This includes thorough patient and caregiver education on the risks and benefits of opioid use, safe storage and disposal of medications, and regular follow-ups to monitor for signs of misuse or dependence.
By balancing effective pain relief with safety precautions, providers can mitigate the risks associated with opioid use in pediatric patients.
Non-Pharmacological Pain Management
Non-pharmacological pain management strategies play a vital role in pediatric care, providing complementary and sometimes primary pain relief methods that avoid the risks associated with pharmacological treatments.
These strategies encompass physical, behavioral, and cognitive measures, emphasizing a holistic approach to pain management that includes environmental and emotional support.
Physical Measures
Physical measures, such as heat and cold therapy, acupuncture, massage, exercise, and physical therapy, are effective in managing various types of pain. Heat and cold therapy can reduce inflammation and soothe sore muscles, while acupuncture and massage promote relaxation and pain relief through tactile stimulation and improved circulation.
Exercise and physical therapy help maintain mobility and reduce pain associated with musculoskeletal conditions, enhancing overall physical function and recovery.
Behavioral Measures
Behavioral measures like biofeedback, relaxation techniques, and art/play therapy help children manage pain by reducing stress and anxiety, which can exacerbate pain perception. Biofeedback involves using electronic devices to monitor physiological functions, teaching children to control processes such as heart rate and muscle tension to alleviate pain.
Relaxation techniques, including deep breathing and progressive muscle relaxation, calm the mind and body, providing relief from pain and discomfort. Art and play therapy offer creative outlets for expressing emotions and distract children from their pain, fostering a positive coping mechanism.
Cognitive Measures
Cognitive measures leverage the power of the mind to influence pain perception. Techniques such as video games, virtual reality (VR), and imagery provide engaging distractions that can significantly reduce pain levels.
Video games and VR immerse children in interactive environments, diverting their attention from pain and providing a sense of control and empowerment. Imagery, or guided visualization, helps children imagine pleasant scenarios, reducing stress and altering their pain experience.
Supportive Environment and Emotional Support
Creating a calm, supportive environment is crucial for effective pain management in children. This involves minimizing stressors, maintaining a comfortable and soothing atmosphere, and providing emotional support from family and caregivers. Encouraging family involvement in pain management helps children feel secure and supported, enhancing their ability to cope with pain.
Emotional support, including empathetic communication and reassurance, builds trust and reduces fear, contributing to a more positive pain management experience.
Multimodal and Interdisciplinary Approach to Pediatric Pain Management
Pain in children is a complex and multifactorial experience that necessitates a comprehensive and nuanced management strategy. Recognizing the multifaceted nature of pain, an effective approach combines pharmacological and non-pharmacological interventions tailored to the individual needs of each child.
This holistic method involves the coordinated efforts of an interdisciplinary team, including physicians, nurses, therapists, and psychologists, to address the various dimensions of pain and enhance overall treatment outcomes.
Comprehensive Management Strategy
A multimodal approach to pain management integrates multiple therapies to address the different aspects of pain, from its physical sensations to its emotional and psychological impacts. Pharmacological interventions, such as the use of opioids, non-opioid analgesics, and adjuvant medications, provide the necessary chemical relief to mitigate pain.
These medications are selected and dosed carefully, considering the child’s age, weight, and specific health conditions to ensure safety and effectiveness. Complementing pharmacological treatments, non-pharmacological interventions play a crucial role in pain management.
Techniques such as physical therapy, acupuncture, and massage address the physical aspects of pain, while behavioral therapies like biofeedback, relaxation techniques, and art therapy help children manage their emotional and psychological responses to pain. Cognitive measures, including the use of video games, virtual reality, and guided imagery, provide engaging distractions that can significantly reduce pain perception.
Interdisciplinary Team Involvement
Effective pediatric pain management requires the collaborative efforts of an interdisciplinary team. Physicians lead the medical aspect of pain management, prescribing appropriate medications and monitoring the child’s overall health. Nurses provide essential bedside care, administering medications, and observing the child’s response to treatment.
Therapists, including physical, occupational, and recreational therapists, implement non-pharmacological interventions, helping children regain physical function and providing therapeutic activities to distract and comfort. Psychologists address the emotional and psychological dimensions of pain, offering counseling and behavioral therapies to help children cope with their pain and reduce anxiety and stress.
By working together, this interdisciplinary team ensures a holistic and coordinated approach to pain management, addressing all facets of the child's pain experience and promoting better health outcomes.
Barriers and Challenges in Pediatric Pain Management
Despite the availability of various pain management tools and techniques, several barriers and challenges hinder their effective use in pediatric care. These include the underutilization of pediatric-specific pain assessment tools, a lack of awareness and fear of adverse effects among healthcare providers, the significant role of anxiety and emotional factors in exacerbating pain, and the need for improved education and training in pediatric pain management.
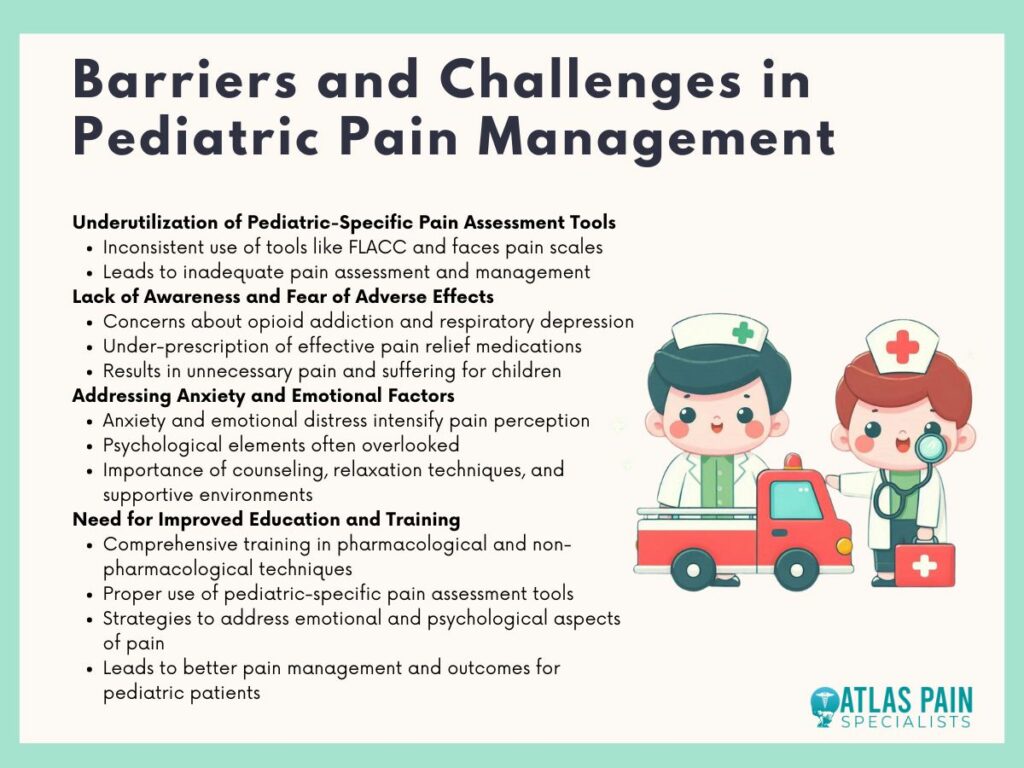
Underutilization of Pediatric-Specific Pain Assessment Tools
One of the major challenges in pediatric pain management is the underutilization of pain assessment tools designed specifically for children. These tools, such as the FLACC scale and faces pain scales, are crucial for accurately assessing pain in children who may not be able to articulate their pain levels. However, healthcare providers may not consistently use these tools, leading to inadequate pain assessment and management.
Lack of Awareness and Fear of Adverse Effects
Healthcare providers often exhibit a lack of awareness or express fear regarding the adverse effects of pain medications in children. Concerns about opioid addiction, respiratory depression, and other side effects can lead to the under-prescription of effective pain relief medications. This fear and lack of knowledge can result in children experiencing unnecessary pain and suffering.
Addressing Anxiety and Emotional Factors
Anxiety and emotional distress significantly impact a child's perception of pain, often intensifying their pain experience. Healthcare providers sometimes overlook these emotional factors, focusing solely on the physical aspects of pain. Addressing these psychological elements through counseling, relaxation techniques, and supportive environments is essential for comprehensive pain management.
Need for Improved Education and Training
There is a pressing need for improved education and training of healthcare providers in pediatric pain management. Comprehensive training programs that cover both pharmacological and non-pharmacological pain management techniques, the use of pediatric-specific pain assessment tools, and strategies to address emotional and psychological aspects of pain are vital. Enhancing providers' knowledge and skills will lead to more effective pain management and better outcomes for pediatric patients.
Conclusion
Effective pain management in children demands a multimodal and interdisciplinary approach that addresses both physical and emotional aspects of pain. By utilizing pediatric-specific assessment tools, overcoming fears related to medication side effects, and enhancing provider education, healthcare teams can significantly improve pain management strategies.
Integrating pharmacological treatments with non-pharmacological techniques and ensuring comprehensive training for healthcare providers are key steps toward optimal care. By addressing these challenges, we can enhance the quality of life for pediatric patients, ensuring they receive the compassionate and effective pain relief they deserve.
About Dr. Sean Ormond