What Causes Knee Pain in Females?
Knee pain is a common complaint among women of all ages and activity levels. While anyone can experience knee problems, women are more likely to develop certain conditions due to differences in anatomy, hormones, and biomechanics.
From chronic issues like arthritis to sports-related injuries and muscle imbalances, understanding what causes knee pain in females can help with early diagnosis, prevention, and effective treatment. Two key areas to examine include how a woman’s anatomy affects knee function and the specific medical conditions that frequently lead to knee pain.
Anatomical and Biomechanical Differences in Female Knees
Several unique anatomical and biomechanical characteristics in women contribute to a higher risk of knee pain compared to men. Differences in bone structure, muscle strength, and joint stability all affect how the knee functions during movement.
These factors change how forces are distributed across the knee joint and influence its overall stability, making women more susceptible to pain and injury. Understanding these differences is key to addressing knee problems and developing effective prevention and treatment strategies.
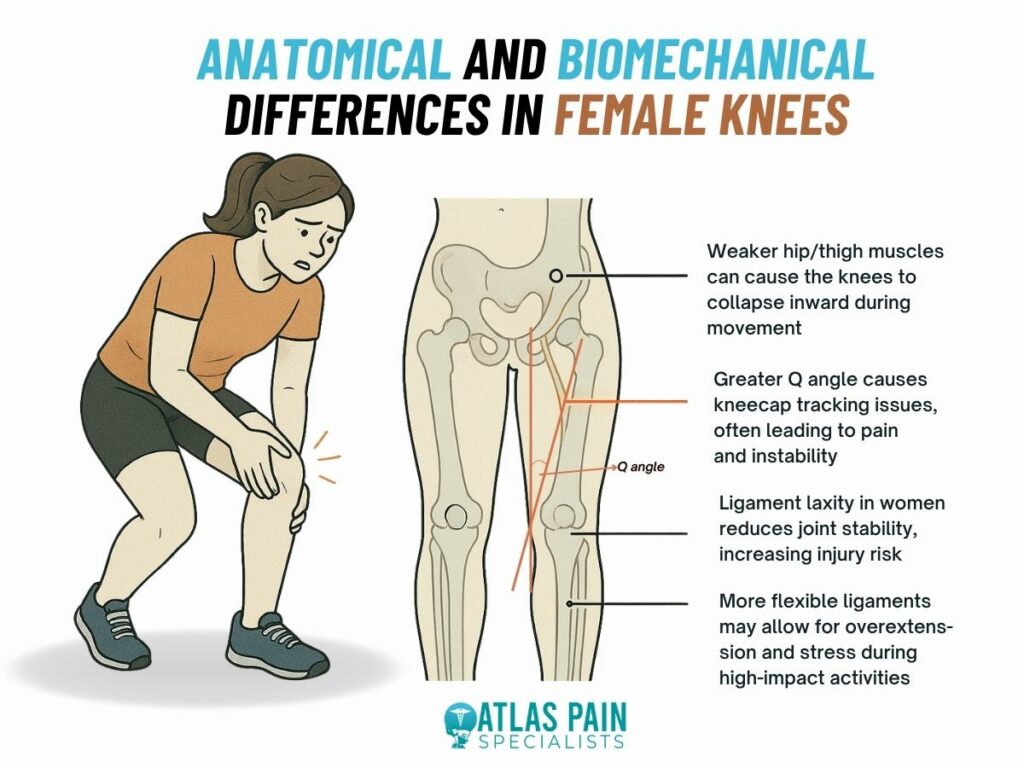
Wider Pelvic Structure and Increased Q Angle
Women naturally have a wider pelvic structure, which leads to a larger Q angle, the angle between the hip and knee. This changes how forces are distributed across the knee joint, increasing stress and often causing the kneecap to move improperly during activities such as walking or running.
Impact on Kneecap Movement
Abnormal kneecap tracking can irritate the cartilage beneath the patella. This irritation often results in patellofemoral pain syndrome, commonly called “runner’s knee,” which is a frequent cause of pain at the front of the knee.
Muscle Imbalances and Knee Alignment
Weakness in thigh and hip muscles, especially those that stabilize the knee, can lead to poor alignment during movement. For example, weak hip muscles may cause the knee to drift inward, increasing strain on the joint and raising the risk of pain and injury.
Ligament Laxity and Joint Stability
Women generally have more ligament laxity, meaning their ligaments are more flexible. While this flexibility allows a greater range of motion, it can make the knee joint less stable. This instability makes women more susceptible to ligament injuries, particularly anterior cruciate ligament (ACL) tears, which are more common in females than males.
Common Medical Conditions Causing Knee Pain in Women
Knee pain in women can be linked to a variety of medical conditions, many of which are influenced by anatomy, hormones, and repetitive movement patterns. While some discomfort may come from temporary strain, persistent or worsening pain often points to a deeper issue. Below are some of the most common medical conditions that cause knee pain in women.
Osteoarthritis
Osteoarthritis is one of the leading causes of chronic knee pain. This condition involves the gradual breakdown of cartilage, which cushions the bones in the joint. When cartilage wears away, bones begin to rub against each other, leading to stiffness, swelling, and discomfort.
This condition is more common and often more severe in women. Hormonal changes, especially after menopause, may increase inflammation and cartilage loss. In addition, women’s wider hips and differences in joint alignment place extra mechanical stress on the knees, accelerating wear over time.
Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disorder where the immune system attacks the lining of the joints. This leads to swelling, pain, stiffness, and over time, joint damage or deformity.
Women are more likely to develop this condition, especially in midlife. In the knees, rheumatoid arthritis can cause chronic inflammation that makes movement difficult and uncomfortable. Unlike osteoarthritis, it affects the entire body and can impact both knees at once.
Patellofemoral Pain Syndrome
Also known as runner’s knee, this condition causes pain around or behind the kneecap. It often results from poor patellar tracking, usually caused by muscle imbalances or misalignment in the lower body.
Patellofemoral pain is especially common in active women. Weaker hip stabilizers and increased joint mobility can cause the kneecap to shift out of place during movement. This may lead to aching or discomfort during squatting, stair climbing, or even sitting for long periods.
Ligament Injuries
Ligament injuries, particularly anterior cruciate ligament (ACL) tears, are more frequent in women. These injuries often happen during sports or activities that involve sudden stops, pivots, or jumps.
Female athletes tend to move differently than males during these activities. For example, landing with straighter knees or inward knee motion can place extra strain on the ACL. Hormonal fluctuations may also affect joint stability, contributing to the higher injury rate.
Meniscus Tears
The meniscus is a pad of cartilage that cushions the space between the thigh bone and shin bone. A tear can occur from a sudden twisting movement or gradual wear with age.
In women, hormonal effects on connective tissue may increase the risk of meniscal injury. These tears can cause swelling, joint stiffness, and locking. Some may heal with rest and therapy, while others require surgical repair.
Tendonitis
Tendonitis is inflammation of the tendons that connect muscles to the knee. It often affects the patellar tendon or quadriceps tendon and is typically caused by overuse.
Women who engage in repetitive activities like running, cycling, or jumping are at risk, especially if there are imbalances in surrounding muscle groups. Pain often feels sharp during activity and may linger afterward. Early management helps prevent chronic symptoms.
Iliotibial Band Syndrome
Iliotibial band syndrome causes pain on the outer side of the knee. It happens when the iliotibial band, a thick band of tissue running from the hip to the shin, rubs repeatedly against the femur.
This condition is particularly common in female runners due to wider hips and increased tension on the band. Weak hip muscles and poor running form can make the problem worse. Treatment focuses on stretching, strengthening, and correcting movement patterns.
Hormonal Influences on Knee Health
Hormones play a critical but often overlooked role in knee pain among women. Fluctuations in estrogen, progesterone, and relaxin levels can affect joint stability, pain sensitivity, and the health of ligaments and cartilage. These hormonal shifts occur naturally throughout different stages of life, including the menstrual cycle, pregnancy, and menopause, and can significantly influence knee function and injury risk.
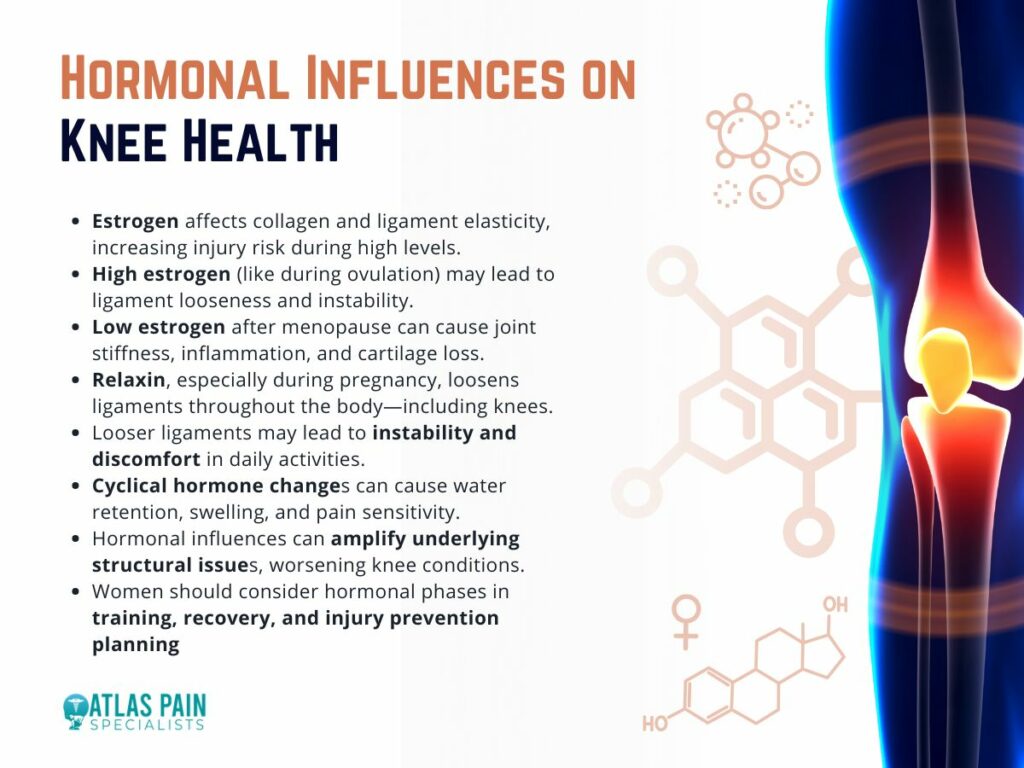
Estrogen
Estrogen, in particular, impacts the elasticity of ligaments and the production of collagen, a key structural protein in connective tissue. High estrogen levels, such as during ovulation, can make ligaments more flexible, which may increase the risk of knee injuries like ACL tears.
Conversely, declining estrogen levels during menopause may contribute to joint stiffness, cartilage breakdown, and increased inflammation, which are hallmark symptoms of osteoarthritis.
Relaxin
Relaxin, another hormone that rises during pregnancy, is known for loosening the pelvic joints to prepare for childbirth. However, its effects are not limited to the pelvis.
Relaxin also affects other ligaments in the body, including those that support the knee. This can lead to increased laxity and instability in the knee joint, which may result in discomfort or pain during routine activities like walking or climbing stairs.
Cyclical Knee Pain
Many women also report cyclical knee pain that worsens during certain phases of their menstrual cycle. Hormonal changes can cause water retention, joint swelling, or increased pain sensitivity, even in the absence of an injury or condition.
Lifestyle and Footwear Choices
Everyday habits, particularly related to footwear and activity levels, have a major impact on knee health in women. Seemingly small choices, like what shoes to wear or how long one remains seated, can add up over time and contribute to chronic knee pain or sudden injuries.
- High heels are a common example. When women wear heels, their center of gravity shifts forward, increasing pressure on the front of the knee and altering the body’s natural alignment. This posture places continuous strain on the quadriceps and patellar tendon, increasing the likelihood of developing patellofemoral pain syndrome or tendonitis. Wearing heels regularly can also shorten calf muscles, limit ankle mobility, and further affect knee joint mechanics.
- Improper athletic footwear is another concern. Shoes without proper arch support, shock absorption, or heel stability can lead to uneven weight distribution and inefficient movement patterns. Over time, this can cause imbalances in the hips, knees, and ankles, leading to pain or injury. Women who run, cycle, or engage in high-impact workouts should wear activity-appropriate footwear and replace it regularly.
- Sedentary habits can also contribute to knee pain. Extended periods of sitting, especially with knees bent, can cause tightness in the hip flexors and hamstrings. These muscle imbalances place stress on the knees and reduce joint support. Conversely, overuse from repetitive activities like stair climbing, jogging, or squatting, especially without proper technique, can inflame tendons and irritate cartilage.
- Carrying heavy handbags on one side of the body, poor posture, and even standing for long periods in one position can also lead to subtle shifts in alignment that gradually wear down the knees.
Knee Pain Location Chart Explained
Knee pain in women often comes from a mix of structural differences, hormonal changes, and daily habits. Factors like wider hips, looser ligaments, poor footwear, and repetitive movements all play a role in how knee problems develop over time. Knowing these causes can help you take simple and effective steps to prevent injury and manage discomfort. Building muscle strength, improving posture, choosing supportive shoes, and adjusting activity based on your body's needs can go a long way in protecting your knees.
Even with this understanding, one important question remains. Where exactly does it hurt? The location of your knee pain can reveal a lot about what might be going on inside. In the next part of this blog, we will walk you through a detailed knee pain location chart to help you better understand your symptoms and what they could mean.
About Dr. Sean Ormond