
The Connection Between Chronic Pain and Sleep Disorders: Breaking the Cycle
Chronic pain and sleep disorders are closely linked, forming a cycle that affects quality of life. Understanding this relationship is crucial for effective treatment.
This article explores how chronic pain impacts sleep and vice versa. Effective management involves strategies like pain management techniques, Cognitive Behavioral Therapy for Insomnia (CBT-I), and addressing sleep disorders.
By adopting integrated interventions and lifestyle changes, we can break the cycle and improve the overall well-being of those affected.
Understanding Chronic Pain
Chronic pain is defined as pain that persists for more than three months and can arise from various conditions, including arthritis, fibromyalgia, neuropathy, and migraines. Unlike acute pain, which serves as a warning signal of injury or illness, chronic pain often persists beyond the initial injury or disease resolution. This prolonged pain can lead to significant physical, emotional, and psychological distress.
The Role of Sleep in Health
Sleep is a fundamental biological process crucial for physical and mental health. It is during sleep that the body undergoes repair and rejuvenation, and the brain processes and consolidates memories. A lack of adequate sleep can impair cognitive function, weaken the immune system, and increase susceptibility to various health conditions, including cardiovascular diseases, diabetes, and mental health disorders.
The Impact of Chronic Pain on Sleep
Chronic pain can have a significant impact on sleep quality and quantity, creating a vicious cycle where poor sleep exacerbates pain, and increased pain disrupts sleep further. Here's how chronic pain affects sleep:
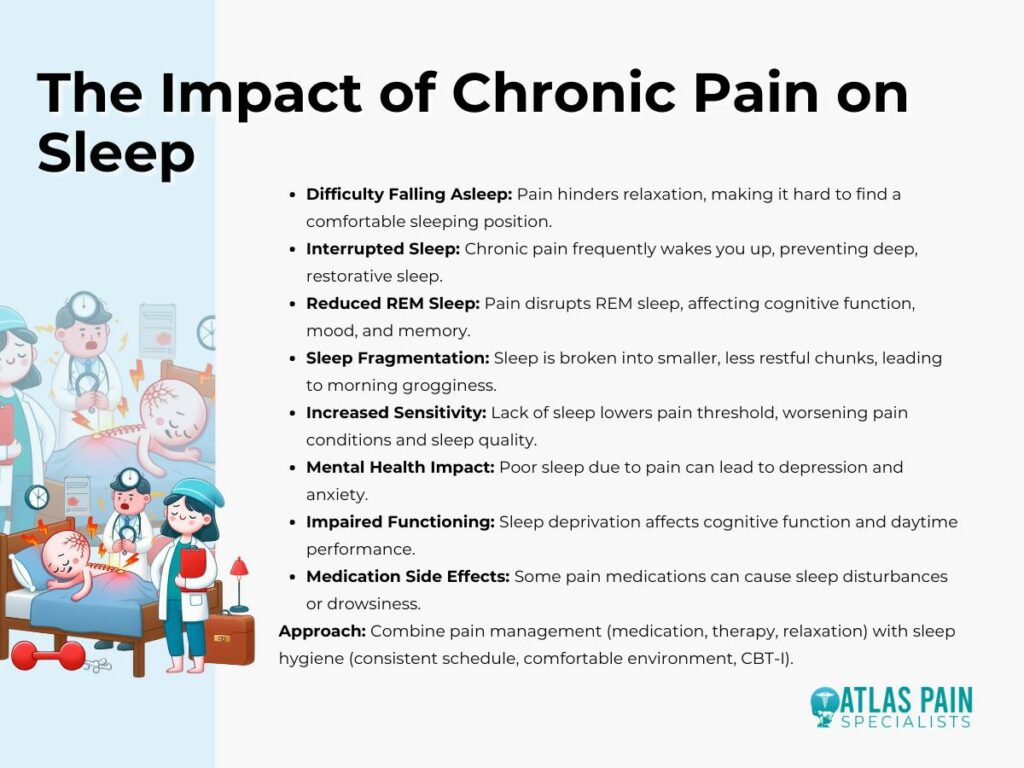
- Difficulty Falling Asleep
Pain can make it difficult to relax and fall asleep. When you're in pain, it's hard to find a comfortable position, which can prolong the time it takes to fall asleep.
- Interrupted Sleep
Even if you manage to fall asleep, chronic pain can frequently wake you up throughout the night. This interruption prevents you from getting deep, restorative sleep.
- Reduced REM Sleep
REM (rapid eye movement) sleep is crucial for cognitive function, memory consolidation, and mood regulation. Chronic pain can disrupt REM sleep, leading to cognitive impairment, mood disturbances, and memory problems.
- Sleep Fragmentation
Chronic pain can cause sleep fragmentation, where sleep is broken into smaller, less restful chunks. This fragmented sleep pattern can leave you feeling groggy and unrefreshed in the morning.
- Increased Sensitivity
Lack of sleep can lower your pain threshold, making you more sensitive to pain. This increased sensitivity can worsen existing pain conditions, leading to a further decline in sleep quality.
- Mental Health Impact
Poor sleep due to chronic pain can contribute to mental health issues such as depression and anxiety. The combination of physical discomfort and sleep disturbances can take a toll on your emotional well-being.
- Impaired Functioning
Sleep deprivation resulting from chronic pain can impair cognitive function, concentration, and overall daytime functioning. This can affect your performance at work or school and increase the risk of accidents.
- Medication Side Effects
Some medications used to manage chronic pain can also affect sleep. For example, opioid painkillers may cause drowsiness or sleep disturbances.
Addressing chronic pain and sleep disturbances often requires a multi-faceted approach. This may include pain management strategies such as medication, physical therapy, or relaxation techniques, as well as sleep hygiene practices like maintaining a consistent sleep schedule, creating a comfortable sleep environment, and practicing relaxation techniques before bed. Cognitive-behavioral therapy for insomnia (CBT-I) can also be effective in improving sleep quality in individuals with chronic pain.
How Sleep Disorders Affect Chronic Pain
Sleep disorders can exacerbate chronic pain in various ways, creating a complex interplay between sleep disturbances and pain perception. Here's how sleep disorders can affect chronic pain:

- Increased Pain Sensitivity
Sleep disorders such as insomnia or sleep apnea can lead to increased sensitivity to pain. When you don't get enough restorative sleep, your body's pain modulation systems may become dysregulated, making you more sensitive to pain stimuli.
- Reduced Pain Tolerance
Sleep deprivation can lower your pain threshold, making chronic pain feel more intense. This can exacerbate existing pain conditions and make it more challenging to manage pain effectively.
- Altered Pain Processing
Sleep disturbances can disrupt the brain's processing of pain signals, leading to alterations in pain perception. This can result in a heightened perception of pain even in the absence of new stimuli.
- Inflammation
Sleep disorders can contribute to systemic inflammation, which is associated with various chronic pain conditions such as arthritis and fibromyalgia. Increased inflammation can worsen pain symptoms and make them more difficult to manage.
- Impaired Healing
Adequate sleep is essential for tissue repair and recovery. Sleep disorders can impair the body's ability to heal from injuries or inflammation, prolonging the duration of pain and delaying recovery.
- Mood Disturbances
Sleep disorders are often accompanied by mood disturbances such as depression and anxiety. These mood disorders can amplify the perception of pain and make it more challenging to cope with chronic pain effectively.
- Medication Interactions
Some medications used to treat sleep disorders may interact with pain medications or exacerbate pain symptoms. For example, certain sleep aids can cause muscle relaxation or sedation, which may worsen pain in individuals with musculoskeletal conditions.
Addressing sleep disorders in individuals with chronic pain is crucial for improving pain management outcomes and overall quality of life. Treatment may involve addressing underlying sleep disorders through behavioral interventions, medication, or therapies such as cognitive-behavioral therapy for insomnia (CBT-I). Additionally, implementing good sleep hygiene practices and creating a conducive sleep environment can help improve sleep quality and reduce pain intensity.
Mechanisms Linking Chronic Pain and Sleep Disorders
The relationship between chronic pain and sleep disorders is bidirectional, with each condition influencing the other through various interconnected mechanisms. Here are some key mechanisms linking chronic pain and sleep disorders:

1. Inflammation
Both chronic pain and poor sleep can increase levels of pro-inflammatory cytokines, which can further exacerbate pain and disrupt sleep.
2. Neurotransmitter Imbalance
Pain and sleep are regulated by neurotransmitters such as serotonin and dopamine. Imbalances in these chemicals can affect both conditions.
3. Hormonal Changes
Hormones like cortisol and melatonin, which regulate stress and sleep-wake cycles, can be disrupted by chronic pain and poor sleep.
4. Psychological Factors
Anxiety, depression, and stress are common in individuals with chronic pain and can also lead to sleep disturbances, creating a feedback loop.
Addressing these mechanisms requires a comprehensive approach targeting both conditions simultaneously. This may involve pharmacological interventions, cognitive-behavioral therapies, lifestyle adjustments, and interdisciplinary pain management strategies tailored to individual needs. By addressing chronic pain and sleep disturbances together, individuals can experience significant improvements in overall well-being and quality of life.
Breaking the Cycle: Addressing Sleep Disorders to Manage Chronic Pain
Breaking the cycle of chronic pain and sleep disorders involves addressing sleep disturbances as a crucial component of pain management. Here's how to approach it:
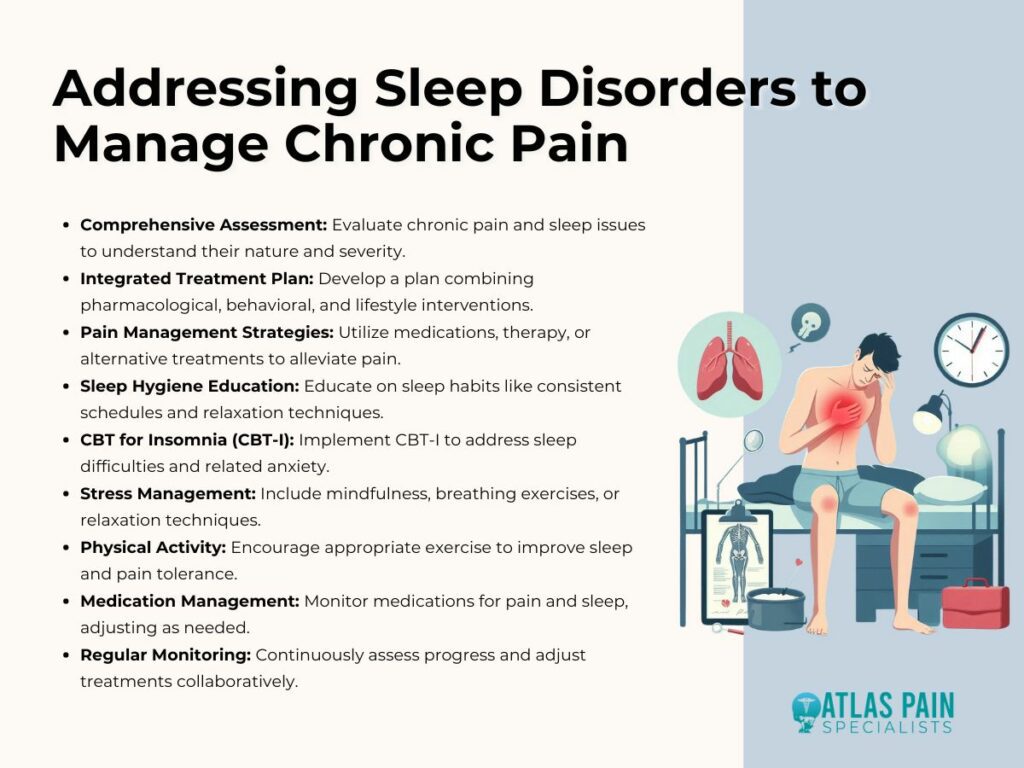
- Comprehensive Assessment
Start by conducting a thorough evaluation of both the chronic pain condition and the sleep disturbances. Understand the nature and severity of the pain, as well as the specific sleep problems experienced, such as difficulty falling asleep, staying asleep, or non-restorative sleep.
- Integrated Treatment Plan
Develop an integrated treatment plan that addresses both the chronic pain and the sleep disorder simultaneously. This plan should involve a combination of pharmacological, behavioral, and lifestyle interventions tailored to the individual's needs.
- Pain Management Strategies
Implement pain management strategies to help alleviate pain symptoms. This may include medications, physical therapy, acupuncture, or other interventions aimed at reducing pain intensity and improving function.
- Sleep Hygiene Education
Provide education on sleep hygiene principles to promote healthy sleep habits. Encourage consistent sleep schedules, a comfortable sleep environment, and relaxation techniques before bedtime. Discourage behaviors that may disrupt sleep, such as excessive caffeine intake or screen time close to bedtime.
- Cognitive-Behavioral Therapy for Insomnia (CBT-I)
Consider CBT-I, which is a highly effective treatment for insomnia. CBT-I focuses on changing thoughts and behaviors that contribute to sleep difficulties and teaches relaxation techniques and strategies for managing sleep-related anxiety.
- Stress Management
Incorporate stress management techniques into the treatment plan to help reduce stress levels, which can exacerbate both pain and sleep disturbances. This may include mindfulness meditation, deep breathing exercises, or progressive muscle relaxation.
- Physical Activity
Encourage regular physical activity, as it can improve sleep quality and reduce pain severity. However, it's essential to choose activities that are appropriate for the individual's pain condition and to avoid overexertion, which can worsen pain symptoms.
- Medication Management
Evaluate the use of medications for both pain management and sleep disorders, taking into account potential interactions and side effects. Work closely with healthcare providers to optimize medication regimens and monitor for any adverse effects.
- Regular Monitoring and Adjustment
Regularly monitor progress and adjust the treatment plan as needed based on feedback from the individual. Encourage open communication and collaboration between the healthcare team and the individual to ensure that their needs are being met effectively.
By addressing sleep disorders as part of a comprehensive pain management approach, individuals with chronic pain can experience improvements in both sleep quality and pain severity, leading to enhanced overall well-being and quality of life.
Conclusion
The complex relationship between chronic pain and sleep disorders poses a significant challenge to individuals' well-being. Understanding the underlying mechanisms is crucial for crafting effective treatment approaches. By implementing a comprehensive strategy that includes pain management techniques and targets specific sleep disorders, we can take the first steps toward breaking this cycle.
Continued research and holistic interventions offer promise for individuals seeking relief from the burden of chronic pain and sleep disturbances. Through these efforts, individuals can reclaim control over their lives and strive for better overall health. By empowering individuals with tailored interventions and promoting holistic well-being, we can foster a future where chronic pain and sleep disorders no longer dictate quality of life.
About Dr. Sean Ormond



