Can Bowels Cause Back Pain? The Gut-Spine Connection Explained
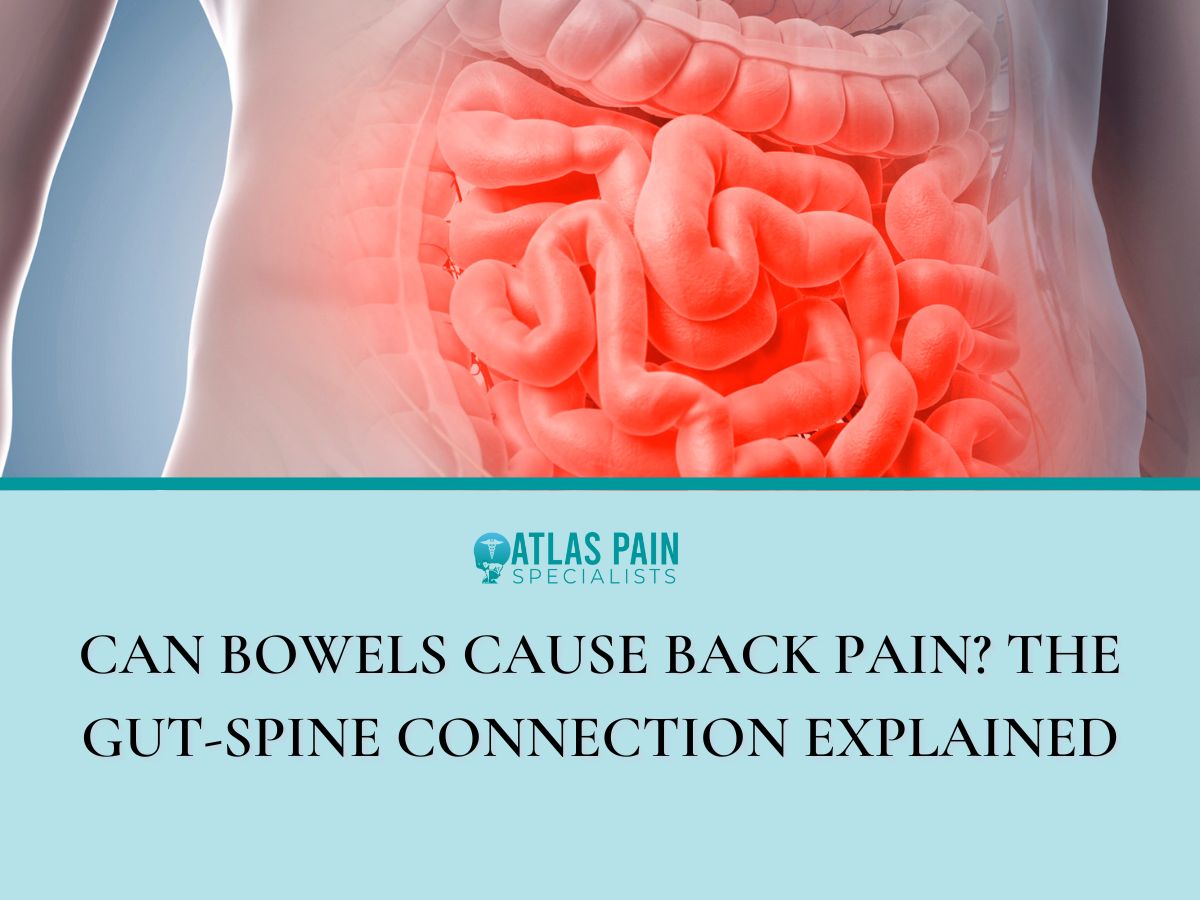
Did you know that the stubborn back pain that just won’t go away, no matter how much you stretch, adjust your chair, or crack your spine might not be due to muscles or posture? It might sound odd at first, but your digestive system and your spine are more connected than most people realize.
Think about how your body feels when you're bloated or constipated. There's that pressure, that heaviness in your abdomen, and sometimes a strange ache that seems to reach around to your lower back.
It's not imagination because your gut has a way of pulling your body out of balance. Can bowels cause back pain? Let's find out.
When Your Gut Talks to Your Back
It’s easy to focus only on the spot that hurts. Your back flares up, so you stretch, lie down, or reach for something to numb the pain.
But when the same pain keeps coming back, especially in your lower back, it’s worth looking somewhere else. Sometimes, the answer doesn't lie in your muscles or spine but starts in your gut.
The Gut-Spine Connection
Your body works as a system, and that includes your digestive system and spine. The two share a deep connection through nerves and pathways you can’t see but often feel.
When something irritates your gut, your nervous system can send pain signals to your back. These signals might feel like tension, soreness, or even sharp aches that won’t ease up.
This can start due to something as simple as trapped gas or slowed digestion. Pain signals can travel fast, and your brain doesn’t always pinpoint where they began.
Why Gut Inflammation Can Show Up as Back Pain
During gut inflammation, your immune system reacts, your muscles tighten, and the discomfort can spread. That inflammation can affect your posture, your core strength, and even your body’s ability to handle everyday movement without triggering back pain.
Your lower back sits right behind much of your digestive system. When things swell or slow down in your gut, pressure builds up and pushes out, and your spine feels it.
It doesn’t take much for this pressure to throw off your alignment or irritate the nerves around your spine. The pain can feel dull, or it can be sharp, but in either case, it feels like it’s coming from your back.
Common Digestive Problems That Might Be Behind Your Back Pain
You probably don’t expect your gut to be responsible for that tight, aching feeling in your lower back. It often feels like two completely different systems since your stomach handles food, and your back supports movement.
Common Digestive Issues and the Back Pain They May Trigger
| Digestive Issue | What It Does to Your Body | How It May Lead to Back Pain |
| Constipation | Slows bowel movement, causes abdominal pressure | Extra pressure strains the lower back and pelvic muscles |
| Bloating | Traps gas and causes distension | Can change posture and stress spinal alignment |
| IBS (Irritable Bowel Syndrome) | Causes chronic cramping, irregular digestion | Can lead to tension in lower back and hips |
| Gut Inflammation | Triggers immune response and systemic inflammation | Increases pain sensitivity in joints and muscles |
| Food Intolerances | Leads to gas, cramps, or slow digestion | Discomfort may cause tightness and back strain |
But when one struggles, the other can react. Your digestive issues might be sending out warning signs that show up far from your stomach.
- Constipation
When your bowel movements slow down, your gut holds on to more than it should. This leads to bloating and pressure that builds up inside your abdomen.
Your lower back sits right behind that area, so the extra weight and tension can press directly against your spine. Constipation can also strain the muscles around your pelvis and back.
As your body tries to compensate, you might feel stiffness or soreness that doesn’t go away with rest. For some people, this becomes a cycle involving back pain that makes movement harder and slows digestion even more.

- Bloating
You might associate bloating with discomfort in your stomach or sides, but it often affects the way you sit, stand, and move. When your belly feels swollen and full, you tend to adjust your posture to relieve that tightness, even without realizing it.
Those subtle shifts can throw off your spine’s alignment. Your lower back may arch more than usual, or your muscles may tense up to brace your body.
Over time, that can lead to soreness, fatigue, and sharp aches that feel like they’re rooted in your back.

- Gut Inflammation
When your gut becomes irritated, due to infection, chronic conditions, or even stress, your nervous system becomes more sensitive. That can heighten how your body reacts to other small discomforts, including tension in your back.
Pain that spreads like this often feels unpredictable. One day it might be centered in your lower back, and the next it could move into your hips or sides.
The original source, though, still lies in your gut, where inflammation disrupts the balance your body needs to feel steady and pain-free.

- Irritable Bowel Syndrome
Irritable Bowel Syndrome is known for causing cramps, bloating, and changes in digestion. But it also affects the nervous system and muscles.
When your gut goes through a flare-up, your back can tense up in response, especially in the lower region. This condition often creates a loop where your gut flares up, your back hurts, the discomfort increases your stress, and that stress circles back to make digestion worse.
Breaking this cycle often means paying closer attention to your digestive habits and stress triggers.

Back Pain and Your Diet
You might focus on your posture, your mattress, or your workouts during back pain. But what you eat can affect how your body feels every day, especially your back.
The connection between your diet and your spine isn’t obvious at first, but once you feel it, it’s hard to ignore. Your gut depends on the food you give it, so poor digestion, bloating, and inflammation often trace back to what’s on your plate.
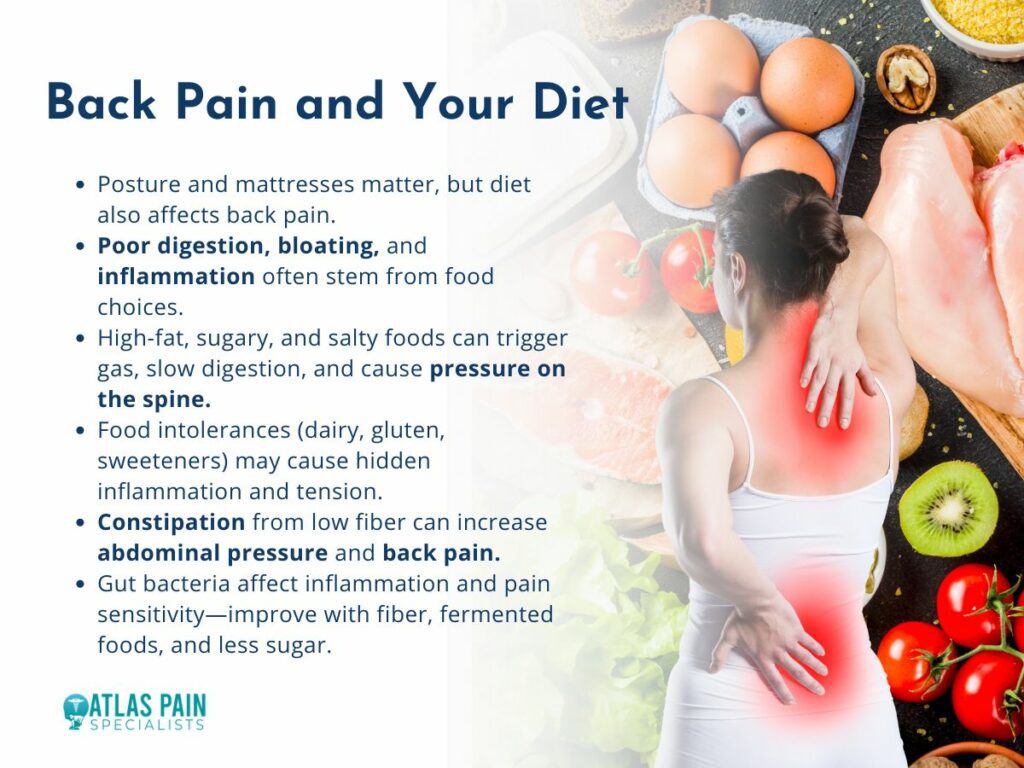
- Food Choices
Some foods trigger gas, inflammation, or digestive slowdown. High-fat meals, processed snacks, and sugary drinks often cause bloating or irregular digestion, which leads to pressure around your lower spine.
Foods high in salt or low in fiber can also make constipation more likely. When your system slows down, your abdomen swells and tightens.
That pressure builds and can press directly against your back muscles, causing discomfort or soreness that sticks around longer than you’d expect from a simple food reaction.
- Food Intolerances
You may be eating something every day that your body struggles with. Common triggers like dairy, gluten, or artificial sweeteners don’t always cause immediate stomach cramps.
Instead, they can lead to low-level inflammation or slow digestion, both of which increase tension in your gut and your back. This kind of discomfort tends to start gradually like a little tightness in your lower back.
By the time the pain becomes clear, the pattern has already set in. Tracking your meals can help you spot these hidden connections before they turn into daily pain.
- Gut Bacteria
The balance of bacteria in your gut helps your digestion and plays a role in how your body handles inflammation, stress, and even pain sensitivity. When this balance gets disrupted, by processed foods, antibiotics, or a lack of variety in your diet, your digestive system may struggle.
An unbalanced gut can lead to more inflammation throughout the body. This increases sensitivity in places like your lower back and hips.
Restoring that balance often involves simple changes like adding more fiber, fermented foods, or cutting back on sugar.
When To See a Doctor
Some aches feel easy to explain, maybe you ate too fast, sat too long, or forgot to stretch. But when your back pain sticks around or keeps coming back after digestive flare-ups it may be pointing to something else.
| Feature | Muscle-Based Back Pain | Gut-Linked Back Pain |
| Pain Trigger | Lifting, twisting, poor posture | Bloating, meals, digestive flare-ups |
| Pain Relief | Improves with stretching or massage | Relieved after bowel movement or digestion eases |
| Pain Location | Centered around muscles or spine | Can spread from abdomen or sides to back |
| Duration | Short-term or related to activity | Lasts longer, often linked to digestion pattern |
| Other Symptoms | Stiffness, soreness | Gas, cramping, irregular stools |
Your body has a way of flagging problems through pain, and the message can get louder over time.
Signs You Should Watch Out For
Back pain that comes with digestive problems can sometimes be linked to conditions that need medical care. When you notice blood in your stool, unexplained weight loss, intense cramping, or fatigue that doesn’t improve with rest, it’s time to take it seriously.
These symptoms may signal something deeper than just poor digestion or a food reaction. Pain that worsens after eating or follows a consistent pattern can also be a red flag.
If your discomfort always appears after meals or seems to flare up after certain types of food, your gut might be reacting in ways that go beyond normal sensitivity.
Chronic Gut Conditions
Conditions like Crohn’s disease, ulcerative colitis, and even small intestinal bacterial overgrowth (SIBO) can cause back pain. These aren't limited to the digestive tract.
Inflammation spreads, your muscles tighten, and the pain often settles in your lower back or pelvic area. These chronic issues can also affect how you absorb nutrients, which plays a role in muscle and bone health.
With time, your body can become weaker and more sensitive to pain.
The Connection Between Gut Health and Chronic Pain: Dietary Considerations
When your back hurts, it’s natural to look for solutions in your posture, your mattress, or how much you lift during the day. The way your body processes food, handles inflammation, and responds to stress all connect.
What you eat influences your gut health, and in turn, your gut shapes how your body feels and functions. Chronic pain often has more than one source, and your digestive system can be one of them.
That’s why knowing The Connection Between Gut Health and Chronic Pain offers useful insight into how inflammation, nutrient absorption, and food sensitivity play into lasting pain. Small changes in how you eat, move, and support your body can reduce both gut discomfort and back tension over time.
About Dr. Sean Ormond