What Is a Discogram and When Is It Needed?
Back pain can be frustrating when every test seems to say “normal.” Sometimes, even advanced imaging like MRI or CT scans fail to reveal the exact source of pain. In these cases, a special diagnostic procedure called a discogram can help.
So, what Is a discogram and when is it needed? A discogram, or discography, is a test doctors use to determine whether a specific spinal disc is causing pain.
It goes beyond simple imaging by recreating the pain in a controlled way to confirm the true source. This article explores how discograms work, when they are used, what patients can expect, and what happens after the test.
Understanding How a Discogram Works
A discogram is not a typical imaging test. It combines imaging with a pain-provocation technique that targets spinal discs suspected of causing chronic back pain. During the procedure, a radiologist or spine specialist injects a contrast dye into one or more discs under X-ray guidance.
The injected dye highlights the disc on imaging and can also reproduce the patient’s usual pain.The most important thing to know is that a discogram helps identify which disc is truly causing pain rather than just showing structural abnormalities.
Many people have bulging or worn discs that do not cause any discomfort. The discogram distinguishes between “painful” and “non-painful” discs, allowing doctors to plan effective treatment.
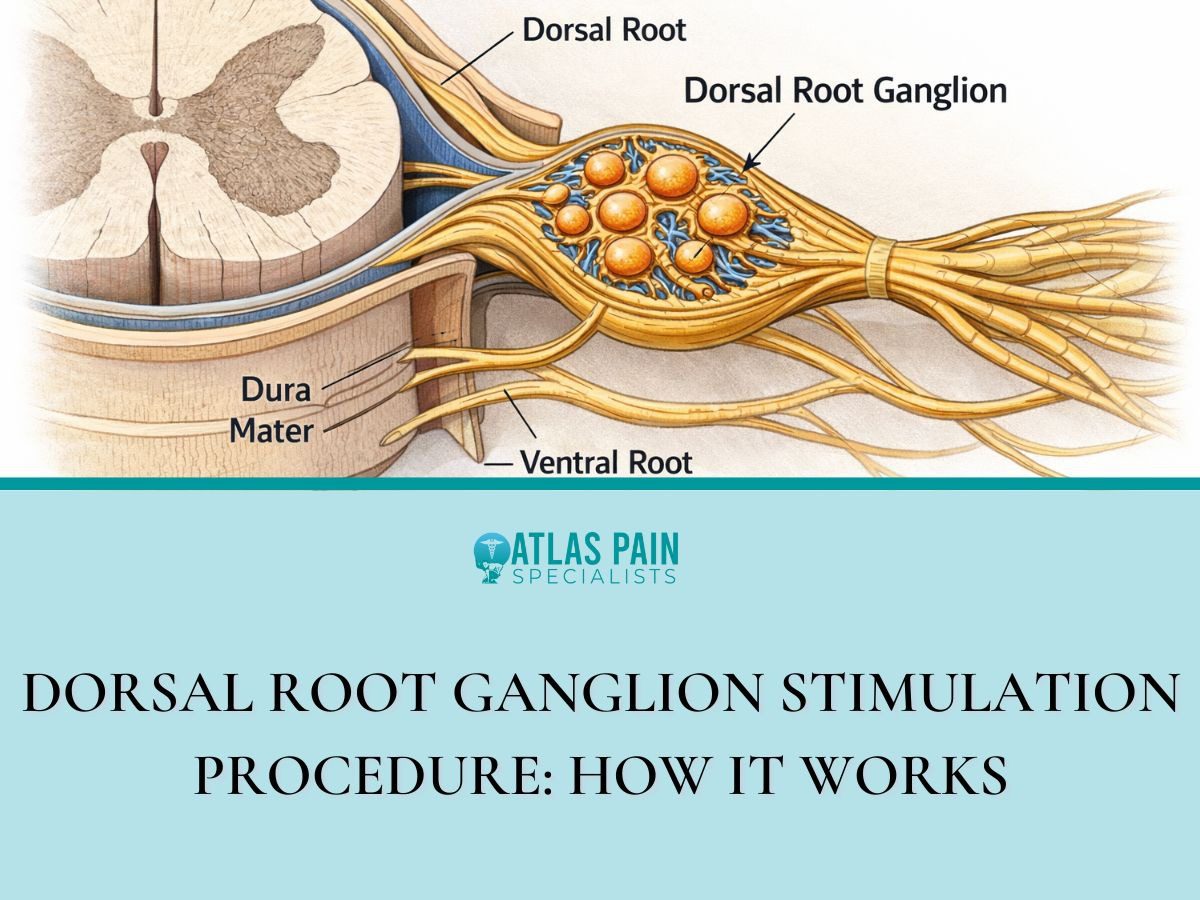
The Anatomy Behind the Test
Between each vertebra in the spine sits a cushion-like structure called an intervertebral disc. These discs act as shock absorbers and allow flexibility.
Each disc has a tough outer layer, the annulus fibrosus, and a soft inner core, the nucleus pulposus. Over time or after injury, discs can degenerate or tear, sometimes leading to chronic low back or neck pain.
A discogram targets these discs one by one. When contrast dye is injected, it increases pressure inside the disc. If that disc is healthy, the patient may feel only mild pressure.
But if the disc is damaged, the dye may leak through small tears, producing pain that matches the patient’s everyday symptoms. This match is what makes the test valuable.
The Procedure Step by Step
- Preparation: The patient lies on a table in a sterile procedure room, usually in a hospital or outpatient radiology center. An intravenous line delivers medication to relax the body but not put the patient fully to sleep.
- Numbing the Area: The doctor cleans and numbs the skin and tissues over the spine using local anesthesia.
- Needle Placement: Using fluoroscopy, a type of live X-ray, the physician guides thin needles into the target discs.
- Contrast Injection: A small amount of contrast dye is injected into each disc. The doctor asks the patient to describe sensations in real time, noting whether the injection reproduces their typical pain.
- Imaging: X-ray or CT images are taken immediately afterward to visualize the shape and integrity of the discs and the spread of contrast dye.
The entire procedure usually takes 30 to 60 minutes. Patients go home the same day after a short recovery period.
When Doctors Recommend a Discogram
Discograms are not for everyone with back pain. They are typically recommended only after conservative treatments and standard imaging fail to explain ongoing pain. Physicians consider several criteria before ordering one.
A discogram is often used when surgical decisions depend on pinpointing which disc is the real problem. For example, if an MRI shows multiple degenerated discs, a discogram can clarify which one is symptomatic so that surgery or targeted therapy focuses on the correct area.
Common Situations That Lead to a Discogram
- Persistent back or neck pain lasting more than three months despite physical therapy, medications, or injections
- Inconclusive MRI or CT scans that show changes but cannot explain the symptoms
- Planning for spinal fusion or artificial disc replacement where identifying the correct disc is crucial
- Evaluating post-surgical pain to determine if pain comes from a previously treated disc or another level
The goal is always to obtain precise information before performing irreversible treatments. The test can prevent unnecessary surgery by confirming that certain discs are not painful at all.
Who Should Avoid a Discogram
Certain conditions make the test inappropriate or risky. Doctors typically avoid discography in patients with active infections, severe allergies to contrast dye, bleeding disorders, or pregnancy.
People with primarily nerve-related pain, such as sciatica from a herniated disc pressing on a nerve, usually do not benefit from a discogram because the test targets disc pain, not nerve compression.
Benefits and Limitations of Discography
Like any medical test, a discogram has both strengths and weaknesses. Understanding them helps patients make informed decisions.
Key Benefits
Discograms can reveal pain sources that imaging alone cannot identify. MRIs show structure, but they cannot always tell whether a visible disc abnormality causes pain.
By comparing pain responses across multiple discs, doctors get functional information that guides treatment. Another advantage is surgical planning accuracy.
A 2020 study in The Spine Journal found that patients who had discograms before spinal fusion were more likely to have successful outcomes because surgeons could better target the pain-producing discs.
The test can also help rule out surgery if no painful disc is found, preventing unnecessary operations.Discograms offer psychological reassurance to patients.
Knowing exactly which disc is problematic and that the pain is real and identifiable can help reduce uncertainty and anxiety. It provides a tangible explanation for chronic pain that may have persisted for years without answers.
Limitations to Consider
However, discograms are not perfect. The procedure can temporarily increase back pain, and results depend on the patient’s pain descriptions, which introduces subjectivity. In rare cases, the injected dye can irritate or inflame a disc, causing discomfort for a few days.
Some experts also question whether discography always predicts surgical success. A 2019 American Journal of Neuroradiology review noted that pain reproduction is helpful but not infallible. Disc degeneration often exists in several levels, and distinguishing which one is most responsible for pain can be challenging.
| Aspect | Strengths | Limitations |
| Purpose | Identifies pain-producing discs | May not detect nerve-related pain |
| Accuracy | More specific than MRI alone | Dependent on patient pain feedback |
| Imaging | Combines fluoroscopy and CT for detail | Dye injection can cause short-term pain |
| Outcome Use | Guides targeted surgery or therapy | Cannot always predict long-term results |
| Recovery | Usually same-day discharge | Mild soreness possible for a few days |
Overall, when used for the right reasons, a discogram remains a valuable diagnostic option in complex spine cases.
What Patients Can Expect After the Procedure
After the discogram, patients rest in a recovery area for about 30 to 60 minutes. The doctor monitors vital signs and ensures pain levels are manageable. Mild soreness at the injection site or temporary worsening of back pain is common but usually fades within a few days.
Following the procedure, patients are advised to rest and avoid heavy lifting or strenuous activity for 24 hours. Ice packs and over-the-counter pain medicine often provide relief. Most people return to normal activities the next day, though doctors may recommend waiting longer if discomfort persists.
The Role of Post-Discogram CT Scans
Many clinics perform a CT scan immediately after the discogram while the dye is still visible. The CT shows detailed cross-sections of each disc, allowing doctors to see internal tears or leaks where contrast has escaped. This combined information the pain response and the imaging pattern offers a complete diagnostic picture.
Understanding Results
Doctors interpret the findings based on three main factors:
- Pain Response: If a particular disc reproduces the patient’s usual pain, it is considered “positive.”
- Imaging Findings: CT scans reveal whether dye spread indicates tears, fissures, or degeneration.
- Comparison with Other Discs: Healthy discs serve as controls. A positive response in one disc but not others strengthens the diagnosis.
Within a few days, the physician reviews the results with the patient. Together they discuss next steps, which might include continued non-surgical management or surgical consultation.
Long-Term Follow-Up
Some patients experience temporary relief after the injection, while others notice increased pain for a few days. This does not necessarily mean the discogram worsened their condition it simply reflects the disc’s sensitivity.
Most people return to their pre-test baseline within a week. Doctors may schedule follow-up appointments to assess pain patterns and discuss treatment options such as physical therapy, epidural injections, or surgery.
Risks, Safety, and Evolving Techniques
Although discograms are generally safe, they are invasive, and every procedure carries some risk. The overall complication rate is low, but awareness helps patients prepare realistically.
Potential Risks
- Infection: Very rare (less than 1% according to a 2022 Radiology report) but possible if bacteria enter the disc during needle insertion.
- Bleeding or nerve irritation: Uncommon, typically mild and temporary.
- Disc damage: Repeated injections or improper technique can, in theory, weaken a disc, though this is rare with modern sterile practices.
- Allergic reaction: Some people may react to the contrast dye, though pre-screening and test doses minimize this risk.
To minimize risk, doctors use strict sterile techniques, fluoroscopic guidance, and single-use needles. Most complications are minor and resolve quickly.
Advances in Discography Technology
Recent innovations have made the test more precise and comfortable. Digital pressure sensors now measure the exact amount of force applied during dye injection, allowing better correlation between pressure and pain.
Some centers use low-volume dye techniques to reduce irritation. In addition, high-resolution CT and MRI follow-ups provide clearer visualization of internal disc structure.
These advances are helping discography remain relevant in the era of high-tech imaging, ensuring it continues to offer unique insights into spine pain.
Alternatives to Discography
If a doctor decides a discogram is not appropriate, other diagnostic tools may be considered. These include:
- MRI with contrast, which highlights inflammation around nerves or discs.
- Facet joint injections, used to identify pain from joints rather than discs.
- Nerve blocks, which temporarily numb specific spinal nerves to see if pain decreases.
Each test serves a different purpose, and sometimes they are used together to form a complete diagnostic picture. Combining results allows physicians to customize care for each patient, ensuring that treatment addresses the true cause of pain.
What Is a Discogram: Understanding Its Role in Future Back Care
Discograms are a bridge between imaging and experience they connect what doctors see with what patients feel. By recreating pain under controlled conditions, the test clarifies which spinal discs are truly responsible for chronic discomfort. It is not the first step in diagnosis, but it becomes essential when pain remains unexplained after standard tests.
Discograms continue to be a key link between traditional radiology and modern surgical planning, providing precision that many other tests lack. As spine care continues to evolve, discography’s role may shift toward integration with advanced imaging and regenerative medicine.
For patients, this means more personalized care and fewer unnecessary surgeries. Discography results could help guide new treatments like stem cell injections or minimally invasive disc repair techniques. These emerging therapies depend on accurate mapping of the pain source something discograms are uniquely designed to provide.
About Dr. Sean Ormond