
How to Stop Anxiety Nerve Pain
Living with anxiety is difficult enough, but when nerve pain joins the picture, the discomfort can feel overwhelming. The sharp, burning, or tingling sensations that travel along nerves are often intensified by stress. Anxiety does not always cause nerve pain directly, but it can heighten sensitivity in the nervous system, making existing discomfort worse and sometimes even triggering new sensations. Learning how to stop anxiety nerve pain involves a mix of calming the mind, protecting the body, and developing habits that support both mental and physical health.
Below we break down the relationship between anxiety and nerve pain, practical strategies for relief, and long-term approaches that bring control back into your hands.
Understanding Anxiety-Related Nerve Pain
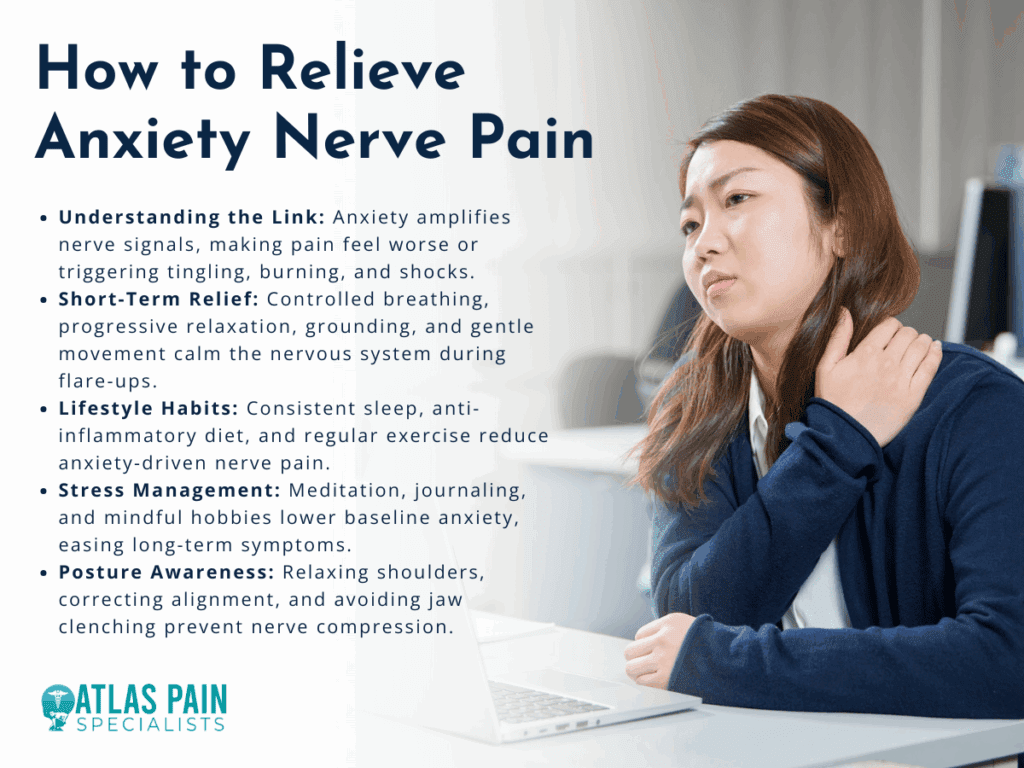
When people first experience nerve pain during an anxious period, it can be confusing. Anxiety can cause muscle tightness, disrupted blood flow, and overactive nerve signaling. These physical reactions sometimes create sensations similar to neuropathy, such as pins and needles, burning, or electric-like shocks.
The key idea is that anxiety amplifies the nervous system’s signals, making pain feel more intense than it would under calm conditions. For example, if you are already dealing with a pinched nerve, stress hormones like cortisol may heighten your sensitivity to the discomfort. Even in the absence of an existing injury, anxiety can cause body sensations that mimic nerve pain because of constant muscle tension and misfired nerve communication.
Understanding this connection is important. It shifts the perspective from worrying about mysterious symptoms to realizing that the brain and body are linked. Once you recognize the role anxiety plays, you can begin addressing both the physical discomfort and the mental stress that feeds into it.
Short-Term Relief Techniques
Calming nerve pain in the moment often means giving your body and mind a chance to reset. These are methods that can be used during flare-ups to ease symptoms and prevent spirals of anxiety.
The most effective short-term relief combines relaxation with gentle body awareness. When you slow down your stress response, the nervous system becomes less reactive.
Controlled Breathing
Breathing exercises may seem simple, but they directly influence how the nervous system functions. Slow, deep breaths reduce the “fight or flight” response that fuels nerve pain sensitivity. One method is box breathing: inhale for four counts, hold for four, exhale for four, hold again for four, and repeat several times.
Progressive Muscle Relaxation
Tight muscles put pressure on nerves, which can worsen pain. With progressive muscle relaxation, you tense one muscle group at a time for a few seconds, then release. This helps the body recognize the difference between tension and relaxation, often leading to reduced nerve irritation.
Grounding Exercises
Sometimes nerve pain worsens when attention is focused too intensely on it. Grounding techniques, like naming five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste, bring the brain back to the present moment instead of cycling through anxious sensations.
Gentle Movement
If the pain allows, slow stretches or light walking improve circulation and reduce stiffness. Even a few minutes of shoulder rolls or neck stretches can ease nerve compression and help the body relax.
Lifestyle Adjustments for Long-Term Comfort
Managing anxiety-related nerve pain is not just about handling flare-ups. The way you eat, sleep, move, and handle daily stress determines how often and how severe the pain becomes.
Long-term relief from anxiety nerve pain requires steady lifestyle habits that calm the nervous system and strengthen the body. This does not mean a total life overhaul in a single week. Small, consistent changes build resilience over time.

Sleep and Rest
Poor sleep increases both pain sensitivity and anxiety. Aiming for consistent bedtimes, limiting screen exposure before sleep, and keeping the bedroom cool and quiet can help restore restorative rest. When the brain is rested, the body interprets pain signals less harshly.
Balanced Diet
Inflammation makes nerve pain worse, and stress hormones are also affected by diet. Including foods rich in omega-3 fatty acids, leafy greens, whole grains, and lean proteins helps stabilize mood and reduce inflammation. Avoiding excessive caffeine and sugar prevents spikes in anxiety that can aggravate pain.
Exercise
Physical activity strengthens muscles, improves posture, and reduces chronic tension. Low-impact exercises like swimming, yoga, and cycling are particularly helpful for nerve health. Beyond physical benefits, exercise triggers endorphins, which naturally counter both anxiety and pain.
Stress Management
Incorporating regular stress-reducing practices makes a difference over time. Meditation, journaling, or mindful hobbies like painting or gardening create mental breaks from constant stress. Over weeks and months, this lowers baseline anxiety, which in turn reduces nerve pain sensitivity.
Posture Awareness
Many anxiety sufferers unconsciously hunch their shoulders or clench their jaw. These habits create nerve compression, especially in the neck and back. Paying attention to body alignment during daily tasks can ease strain and prevent pain.
Common Triggers That Worsen Anxiety Nerve Pain
Even when practicing good self-care, certain daily habits or situations can flare up nerve pain. Recognizing these triggers makes it easier to avoid unnecessary discomfort.
Anxiety nerve pain often worsens because of small lifestyle factors that overstimulate the nervous system or strain the body. Becoming aware of them provides another layer of control.

Caffeine and Stimulants
Caffeine may increase alertness, but it also heightens the body’s stress response. Too much coffee, energy drinks, or even strong tea can trigger jitters, muscle tension, and nerve sensitivity.
Prolonged Sitting
Sitting for long periods, especially at desks or with poor posture, compresses nerves in the spine and legs. Breaks to stand, stretch, or walk every hour can reduce flare-ups.
Device Overuse
Constant phone scrolling or laptop use without breaks strains the neck, shoulders, and wrists. This creates nerve compression while also feeding anxiety with overstimulation.
Dehydration
When the body lacks hydration, nerve conduction is less efficient, and muscles become tighter, which may worsen nerve irritation. Drinking water regularly throughout the day supports smoother nerve function.
Emotional Triggers
Stressful conversations, news consumption, or environments that feel unsafe can all spike anxiety, which in turn heightens pain signals. Creating healthy boundaries with media and people helps reduce this effect.
Comparison: Short-Term vs. Long-Term Strategies
| Approach | Short-Term Relief | Long-Term Comfort |
| Breathing & Relaxation | Calms immediate stress response and reduces sensitivity to pain | Builds a resilient nervous system when practiced daily |
| Gentle Movement | Provides instant circulation and reduces stiffness | Strengthens muscles, prevents chronic tension, improves nerve health |
| Grounding & Distraction | Breaks focus on pain during flare-ups | Creates healthier thought patterns and reduces anxiety over time |
| Diet & Hydration | Stabilizes blood sugar and reduces inflammation temporarily | Supports steady energy, balanced mood, and long-term nerve protection |
| Sleep & Rest | A single nap can reduce pain intensity temporarily | Consistent sleep restores the nervous system and prevents recurrent pain flare-ups |
| Professional Support | Offers immediate guidance or treatment when needed | Provides lasting solutions through therapy, medical care, and physical rehabilitation |
Short-term strategies interrupt the cycle in the moment, while long-term practices gradually reduce how often anxiety nerve pain occurs. Both are valuable, and using them together brings the best results.
When to Seek Professional Help
Self-care goes a long way, but sometimes nerve pain and anxiety persist despite best efforts. At that point, it is important to involve medical and mental health professionals.
Persistent nerve pain alongside anxiety should be evaluated to rule out underlying conditions and to provide targeted treatment. Even if the main cause is anxiety, professional support brings relief faster and prevents complications.
Medical Evaluation
Doctors may check for underlying neuropathy, vitamin deficiencies, or musculoskeletal issues. If these are found, addressing them directly often improves both pain and anxiety. Sometimes, simple corrections such as vitamin B12 supplementation or ergonomic adjustments at work can ease discomfort.
Therapy
Cognitive Behavioral Therapy (CBT) is one of the most effective treatments for anxiety, and it also helps people reinterpret and manage physical sensations like nerve pain. By reframing anxious thoughts and practicing coping strategies, therapy reduces the severity of symptoms.
Medication Options
In some cases, medication may be prescribed to calm nerve signaling or to manage anxiety. These range from antidepressants that stabilize mood and nerve sensitivity to medications that specifically target nerve pain. Decisions about medication should always be made in consultation with a healthcare provider.
Physical Therapy
Targeted exercises, nerve gliding techniques, and manual therapy from a trained physical therapist can reduce compression and improve nerve function. This also restores confidence in the body, reducing fear that worsens anxiety.
Building a Daily Self-Care Routine
The best results often come from combining several small practices into a structured routine. Creating consistency reassures the brain and body that they are safe, reducing both anxiety and nerve flare-ups.
A daily self-care routine that balances mind and body is the strongest defense against anxiety nerve pain.
Morning
- Begin the day with gentle stretches such as neck tilts, shoulder rolls, or cat-cow stretches to ease overnight tension.
- Practice five minutes of deep breathing or meditation before checking devices.
- Eat a protein-rich breakfast with eggs, oatmeal, or yogurt to stabilize blood sugar.
Midday
- Take short breaks from work every 60 minutes. Stand, walk, or stretch arms overhead.
- Choose a balanced lunch with lean protein, vegetables, and whole grains to prevent energy crashes.
- Use grounding techniques during stressful moments, especially after meetings or heavy workloads.
Evening
- Engage in 20–30 minutes of light exercise like walking, cycling, or swimming to release built-up tension.
- Limit screen exposure an hour before bedtime, and instead read or listen to calming music.
- Create a consistent wind-down routine with dimmed lights, a warm shower, or herbal tea to signal the body it is time for rest.
By layering these practices, the nervous system adapts to a calmer state, making flare-ups less frequent and easier to manage.
Conclusion
Learning how to stop anxiety nerve pain is about more than chasing away symptoms. It is about understanding the two-way connection between body and mind, then using that knowledge to build healthier patterns. Quick relief techniques help break the cycle during flare-ups, while lifestyle adjustments and professional support provide long-term stability. Over time, the combination of calm breathing, balanced routines, and mindful care gives back control. While nerve pain can feel alarming in the moment, it becomes far less powerful when met with consistent strategies that strengthen both mental and physical resilience.
About Dr. Sean Ormond