Silent Migraine Symptoms: How to Recognize This Hidden Condition
Silent migraines, also known as acephalgic migraines, are a lesser-known type of migraine that occurs without the typical headache pain. Instead, they present with other disruptive symptoms such as visual disturbances, dizziness, nausea, and sensory sensitivities. Because they lack the hallmark head pain, silent migraines are often misdiagnosed or overlooked, making it crucial to recognize their unique signs.
This article covers what silent migraines are, their symptoms, phases, triggers, and causes. It also explores diagnosis, treatment options, and when to seek medical attention, helping those affected manage their condition effectively.
What is a Silent Migraine?
A silent migraine is a type of migraine that presents with typical migraine symptoms, such as aura and sensory disturbances, but without the accompanying headache. These migraines can be just as disruptive as traditional migraines and often go undiagnosed because people do not associate them with migraine disorders.
Common Symptoms of Silent Migraines
Silent migraines can be challenging to identify since they lack the typical headache but still cause significant symptoms. These symptoms can affect vision, cognition, and overall well-being, making daily activities difficult. Here are some common symptoms of silent migraines:
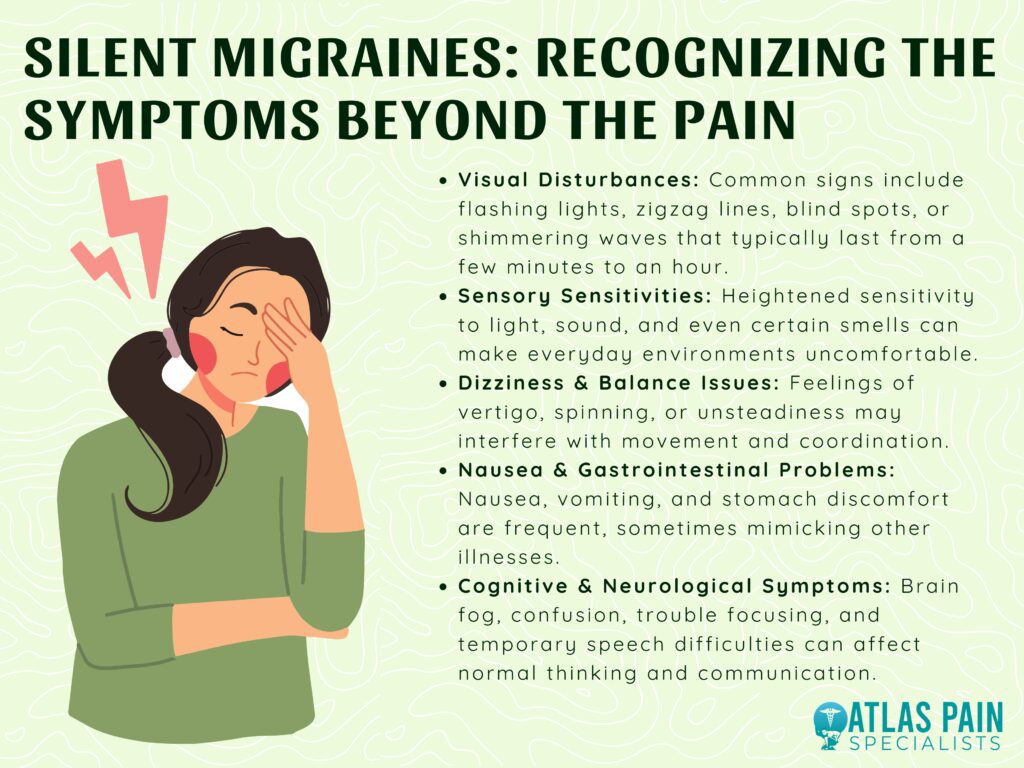
1. Aura and Visual Disturbances
Many people experience flashing lights, zigzag patterns, blind spots, or shimmering waves in their vision. These visual symptoms can last from a few minutes to an hour and often signal the onset of a silent migraine.
2. Sensory Sensitivities
Increased sensitivity to light, sound, and even smells is common. Everyday stimuli, such as bright lights or loud noises, can become overwhelming and contribute to discomfort.
3. Dizziness and Balance Issues
Silent migraines can cause vertigo, unsteadiness, or a spinning sensation. This can make movement difficult and increase the risk of falls or coordination problems.
4. Nausea and Gastrointestinal Problems
Some people experience nausea, vomiting, or stomach discomfort. These symptoms can mimic other conditions, making it harder to recognize a silent migraine.
5. Cognitive and Neurological Symptoms
Brain fog, confusion, difficulty concentrating, and even temporary speech problems can occur. These issues may make tasks like reading, writing, or holding conversations more challenging.
Although silent migraines do not cause head pain, they can still be debilitating. Recognizing these symptoms can help with proper diagnosis and management, improving the quality of life for those affected.
Phases of a Silent Migraine
Silent migraines, like traditional migraines, progress through distinct phases, even though they lack the characteristic headache. Understanding these phases can help identify and manage silent migraines more effectively. Here are the four main phases:
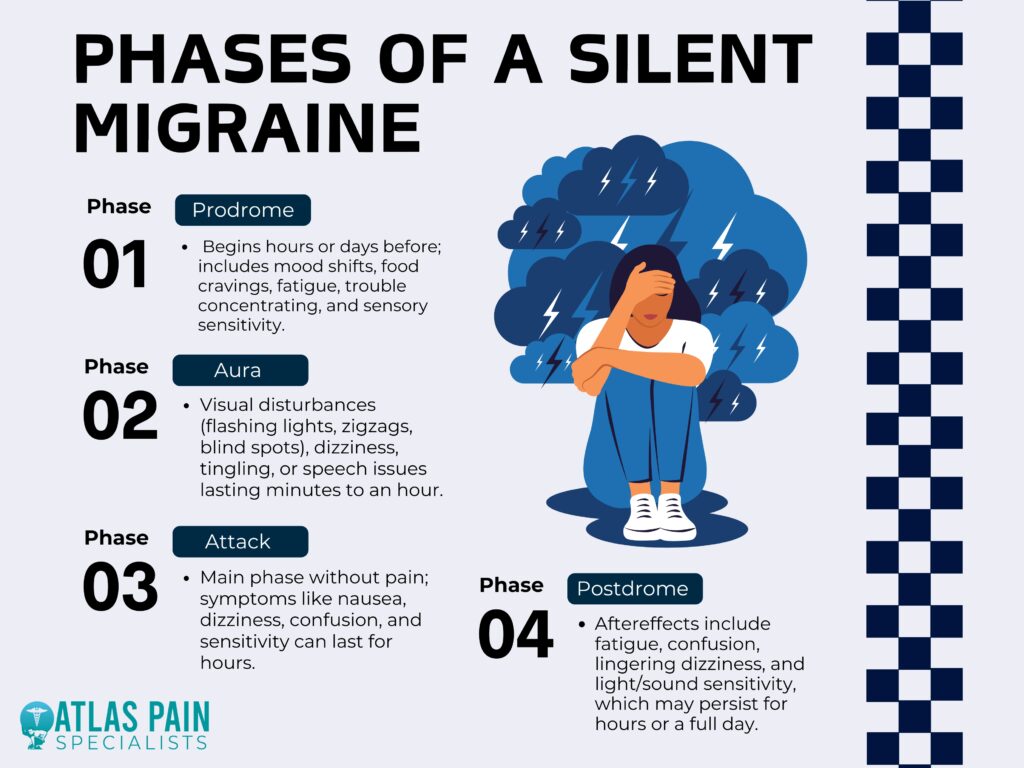
1. Prodrome (Pre-Migraine Phase)
This phase can begin hours or even days before the migraine fully develops. Symptoms may include mood changes, food cravings, fatigue, difficulty concentrating, and increased sensitivity to light or sound.
2. Aura Phase
Many people with silent migraines experience aura, which involves visual disturbances like flashing lights, blind spots, or zigzag patterns. Some may also have tingling sensations, dizziness, or trouble speaking, lasting anywhere from a few minutes to an hour.
3. Attack Phase (Without Headache)
In a silent migraine, the attack phase occurs without head pain but includes symptoms like nausea, dizziness, confusion, or sensory sensitivities. This phase can last from a few minutes to several hours, significantly impacting daily activities.
4. Postdrome (Recovery Phase)
After the attack subsides, many people feel exhausted, confused, or mentally drained. Some may still experience mild dizziness or sensitivity to light and sound, with recovery taking hours or even a full day.
Even without headache pain, silent migraines can be disruptive and challenging to diagnose. Recognizing these phases can help individuals manage symptoms and seek appropriate treatment.
Triggers and Causes of Silent Migraines
Silent migraines can be triggered by various factors, much like traditional migraines. Identifying and avoiding these triggers can help reduce the frequency and severity of episodes. Here are some common triggers and causes of silent migraines:
1. Stress and Anxiety
Emotional stress, anxiety, and tension can trigger silent migraines by affecting brain chemistry and increasing inflammation. Sudden relief from stress, known as the "weekend migraine effect," can also set off an episode.
2. Hormonal Changes
Fluctuations in hormones, especially during menstruation, pregnancy, or menopause, can contribute to silent migraines. Some people are more sensitive to hormonal shifts, making migraines more frequent during certain phases of their cycle.
3. Dietary Triggers
Certain foods and beverages, such as processed meats, aged cheese, chocolate, alcohol, and caffeine, can provoke silent migraines. Additives like MSG and artificial sweeteners may also play a role in triggering attacks. For more insight into whether caffeine can cause dizziness and what steps you might take if this happens to you, click here to learn more about the connection between caffeine and dizziness.
4. Sleep Disturbances
Both too little and too much sleep can contribute to migraines. Irregular sleep patterns, jet lag, or disrupted sleep cycles may increase the likelihood of experiencing a silent migraine.
5. Environmental Factors
Bright lights, strong smells, loud noises, and changes in weather, such as shifts in barometric pressure, can act as triggers. Exposure to screens for extended periods may also increase the risk of silent migraines.
6. Dehydration and Skipped Meals
Not drinking enough water or missing meals can lead to drops in blood sugar levels, which may trigger a silent migraine. Staying hydrated and maintaining a regular eating schedule can help prevent episodes.
Because triggers vary from person to person, keeping a migraine journal can help identify patterns and reduce the frequency of silent migraines. Managing lifestyle factors and avoiding known triggers can improve overall well-being and migraine control.
Diagnosing Silent Migraines
Diagnosing silent migraines can be challenging because they lack the hallmark headache pain, making them easily confused with other neurological or vision-related conditions. Doctors rely on medical history, symptom patterns, and diagnostic tests to rule out other possible causes. Here are the key steps in diagnosing silent migraines:
1. Medical History and Symptom Review
A doctor will ask about the patient’s symptoms, their frequency, duration, and any potential triggers. Since silent migraines can mimic other conditions, a detailed history helps in making an accurate diagnosis.
2. Neurological Examination
A physical and neurological exam is performed to check for abnormalities in vision, coordination, reflexes, and cognitive function. This helps rule out serious conditions like strokes or seizures.
3. Imaging Tests (MRI or CT Scan)
If symptoms are unusual or concerning, doctors may order brain imaging to rule out structural issues, tumors, or other neurological disorders. An MRI or CT scan can help confirm that the symptoms are migraine-related rather than caused by another condition.
4. Electroencephalogram (EEG) (if needed)
In cases where silent migraines resemble seizures, an EEG may be performed to measure brain activity. This test helps distinguish between migraine-related aura and seizure disorders.
5. Migraine Diary and Trigger Identification
Patients are often encouraged to keep a migraine journal, tracking symptoms, triggers, and patterns. This can help confirm a silent migraine diagnosis and guide treatment strategies.
Since silent migraines can be mistaken for other conditions, a thorough evaluation is essential for accurate diagnosis. Once identified, personalized treatment plans can help manage symptoms and reduce migraine episodes.
Treatment and Management
Managing silent migraines involves lifestyle changes, medications, and preventive strategies to reduce symptoms. Since they can be disruptive even without head pain, treatment focuses on controlling triggers and easing symptoms.

1. Lifestyle Modifications
Establishing regular sleep patterns, staying hydrated, and maintaining a balanced diet can help prevent silent migraines. Reducing screen time, managing stress, and avoiding known triggers also play a crucial role in prevention.
2. Medications for Symptom Relief
Over-the-counter pain relievers like ibuprofen or prescription medications such as triptans may help ease migraine symptoms. Anti-nausea drugs and vestibular suppressants can also be used for dizziness or nausea associated with silent migraines.
3. Preventive Medications
For frequent silent migraines, doctors may prescribe beta-blockers, antidepressants, or anti-seizure medications to reduce migraine frequency. Botox injections or CGRP inhibitors may also be options for individuals with chronic migraine patterns.
4. Stress Management Techniques
Practicing relaxation methods such as meditation, deep breathing, and yoga can help lower stress levels and decrease migraine occurrences. Regular physical activity and mindfulness exercises can also contribute to better migraine control.
5. Dietary Adjustments
Identifying and avoiding food triggers like caffeine, alcohol, processed meats, and artificial additives can help prevent silent migraines. Keeping a food journal can be useful in pinpointing specific dietary culprits.
6. Alternative Therapies
Some individuals find relief through acupuncture, biofeedback, or essential oils like peppermint and lavender. Supplements such as magnesium, riboflavin (vitamin B2), and coenzyme Q10 have also been studied for their potential migraine-preventing benefits.
Although silent migraines do not cause head pain, their symptoms can still interfere with daily life. A combination of lifestyle changes, medication, and stress management can help minimize their impact and improve overall well-being.
When to Seek Medical Attention
Silent migraines aren’t life-threatening but can mimic serious conditions like strokes or seizures. Knowing when to seek medical attention ensures proper diagnosis and treatment.
- New or Unusual Symptoms – If migraine-like symptoms appear for the first time, especially without a history of migraines, consult a doctor to rule out other conditions.
- Severe or Prolonged Symptoms – Extreme dizziness, confusion, or vision problems lasting longer than usual should be evaluated.
- Difficulty Speaking or Weakness – Slurred speech, facial drooping, or limb weakness may indicate a stroke and require emergency care.
- Frequent or Disruptive Episodes – Regular silent migraines that interfere with daily life may need preventive treatment.
- No Improvement with Treatment – If symptoms persist despite treatment, a doctor can adjust medications or explore alternatives.
- Sudden Onset After Age 50 – New migraines at this age should be assessed to rule out serious underlying conditions.
Seeking medical attention when necessary can help rule out dangerous conditions and ensure proper management of silent migraines. Early intervention and the right treatment approach can significantly improve quality of life.
Conclusion
Silent migraines can be challenging to recognize and manage due to their lack of head pain and overlapping symptoms with other conditions. However, understanding their signs, triggers, and phases can help individuals take proactive steps to reduce their impact.
By identifying triggers, seeking proper diagnosis, and exploring treatment options, those affected can better manage silent migraines and improve their quality of life. If symptoms are frequent, severe, or unusual, consulting a healthcare professional is essential for proper evaluation and care.
About Dr. Sean Ormond



