Peripheral Nerve Stimulation
In Phoenix Arizona
What is Peripheral Nerve Simulation?
This minimally invasive procedure is particularly effective for neuropathic pain, post-surgical pain, complex regional pain syndrome (CRPS), and even certain types of musculoskeletal pain. Patients who undergo PNS treatment often experience significant pain reduction, improved mobility, and a reduced need for pain medications. Since the device is adjustable and reversible, PNS provides a safe and flexible pain management solution tailored to each individual’s needs.

Benefits
Peripheral Nerve Stimulation
Effective Pain Relief
Minimally Invasive Procedure
Reduced Dependence on Medications
Customizable & Adjustable Therapy
Reversible & Low-Risk Treatment
Improved Quality of Life

Conditions Treated with Peripheral Nerve Stimulation
Purpose
Limitations
Risks
Process
Types

Purpose of Peripheral Nerve Stimulation
The primary purpose of PNS is to interrupt the transmission of pain signals at the nerve level, preventing them from reaching the brain. Unlike medications that mask pain temporarily, PNS provides continuous relief by directly modulating nerve activity. This therapy is particularly beneficial for patients who have not found relief with medications, injections, or physical therapy.
By targeting specific nerves rather than affecting the entire nervous system, PNS minimizes side effects while delivering long-lasting pain control. The ability to adjust stimulation levels gives patients greater control over their pain, making it a customizable and adaptable treatment for those dealing with chronic discomfort.
Limitations of Peripheral Nerve Stimulation
While PNS is highly effective for many types of nerve-related pain, it is not suitable for all pain conditions. The treatment works best for neuropathic pain, meaning it may be less effective for muscle, joint, or inflammatory pain. Patients with widespread pain conditions, such as fibromyalgia, may not experience the same level of relief as those with localized nerve pain.
Additionally, PNS requires a trial period to determine if the therapy is effective before permanent implantation. Not all patients respond to stimulation, and some may require adjustments to find the best settings. Battery maintenance and device adjustments are also necessary over time, making it an ongoing therapy rather than a one-time solution.

Potential Risks of Peripheral Nerve Stimulation
Although PNS is considered a low-risk procedure, there are some potential complications:
- Infection – As with any implanted device, there is a small risk of infection at the surgical site.
- Device Malfunction – The leads or battery pack may require replacement if they stop functioning properly.
- Lead Migration – The electrode may shift slightly, causing changes in stimulation patterns or reduced effectiveness.
- Nerve Irritation – Some patients may experience tingling, burning, or discomfort from overstimulation.
- Allergic Reaction – Though rare, some individuals may react to the implanted materials.
Most risks are minor and manageable, with adjustments or minor corrective procedures if necessary.
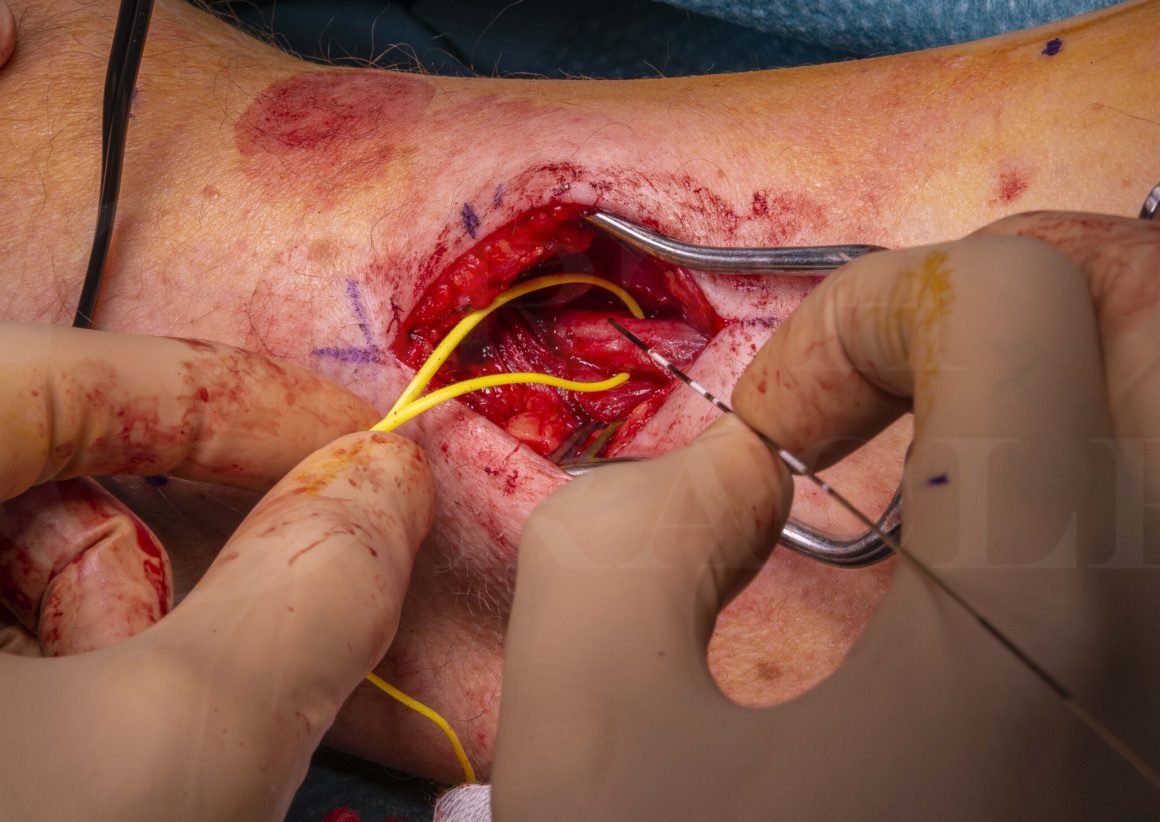
The Peripheral Nerve Stimulation Process
PNS involves a two-step approach: a trial phase and permanent implantation.
- Trial Phase – A temporary electrode is placed near the affected nerve, and the patient wears an external stimulator for about a week to determine if PNS provides significant pain relief.
- Evaluation – If the trial is successful (at least 50% pain reduction), the patient moves forward with permanent implantation.
- Permanent Implantation – A small pulse generator is implanted under the skin, and the electrode leads are permanently placed near the target nerve.
- Device Programming – The stimulation settings are adjusted based on the patient’s comfort and pain levels.
- Recovery & Follow-Up – Patients typically return to normal activities within a few days, with ongoing adjustments to optimize effectiveness.
Types of Peripheral Nerve Stimulation Devices
There are different types of PNS devices available, depending on the patient’s specific needs:
- Traditional PNS Systems – Use continuous stimulation to block pain signals. These systems are rechargeable or battery-powered and can be adjusted as needed.
- Burst Stimulation PNS – Delivers pulsed bursts of electrical stimulation, mimicking natural nerve activity and often providing pain relief without a tingling sensation.
- Wireless & Miniature PNS Devices – Advanced wireless systems eliminate the need for large implants, offering a less invasive option with better cosmetic appeal.
- Temporary PNS Systems – Short-term systems used for acute post-surgical or injury-related pain, typically lasting 60 days before being removed.
Each system is designed to meet different pain management needs, allowing for personalized treatment options that align with a patient’s lifestyle and condition.
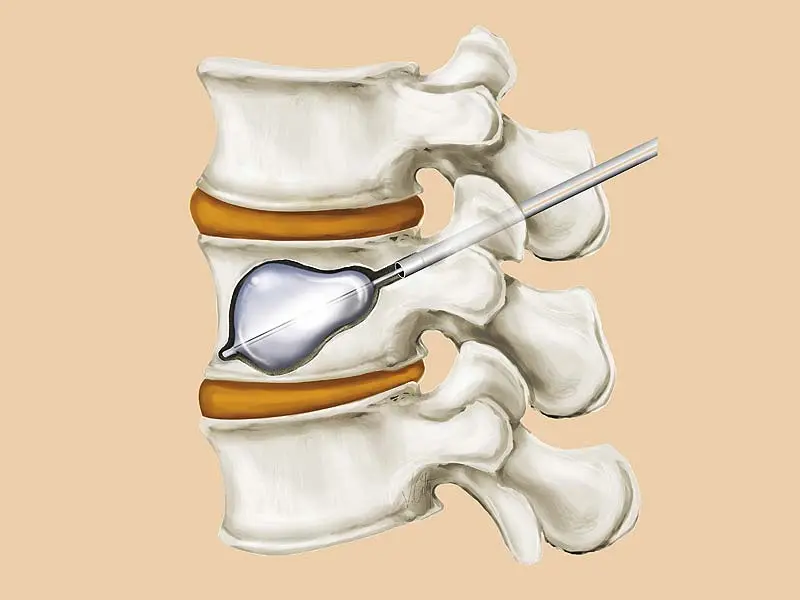
Types of Vertebral Compression Fractures Treated with Kyphoplasty
Kyphoplasty is most effective for acute or subacute compression fractures, meaning fractures that are relatively recent and still causing pain. Some of the common types include:
- Wedge fractures: The front of the vertebra collapses, creating a wedge-like shape and leading to kyphosis (hunchback posture).
- Biconcave fractures: The middle of the vertebra collapses, causing the bone to become concave in appearance.
- Crush fractures: The entire vertebra collapses uniformly, which can lead to severe instability.
The type and severity of the fracture determine whether kyphoplasty or another treatment approach is best.
Ask us anything, or
schedule a same day
appointment.
