How Hormonal Changes Impact Chronic Pain in Women
Chronic pain affects many individuals, and for women, hormonal fluctuations significantly impact pain experience. Hormones like estrogen, progesterone, and testosterone can alter pain sensitivity and modulation throughout life stages such as menstruation, pregnancy, and menopause.
These hormonal changes can exacerbate chronic pain conditions like endometriosis, fibromyalgia, migraines, and irritable bowel syndrome (IBS). Effective pain management involves understanding these hormonal influences.
This article examines how hormonal changes impact chronic pain in women, and provides strategies for managing pain with hormonal considerations. Integrating these factors into pain management can lead to better relief and improved quality of life.
The Role of Hormones in Pain Perception
Hormones play a crucial role in regulating pain perception, influencing how the body experiences and responds to pain. Here’s how different hormones contribute to this complex process:
Estrogen and Pain Sensitivity:
Estrogen, a primary female sex hormone, can affect pain sensitivity by modulating the body's pain pathways. Higher levels of estrogen, such as those during the follicular phase of the menstrual cycle, can increase pain sensitivity, making individuals more susceptible to pain. Conversely, lower levels of estrogen, such as during the luteal phase or menopause, may reduce pain sensitivity, though this effect can vary depending on the individual and the pain condition.
Progesterone and Pain Modulation
Progesterone, another key hormone in the female reproductive system, has been shown to have anti-inflammatory and analgesic properties, which can modulate pain perception. Elevated progesterone levels, particularly during the luteal phase of the menstrual cycle or pregnancy, can help alleviate pain by counteracting some of the inflammatory processes associated with pain. However, fluctuations in progesterone levels can also contribute to variations in pain perception.
Testosterone and Pain Response
Testosterone, though present at lower levels in women, can influence pain perception by exerting analgesic effects. Higher levels of testosterone may contribute to reduced pain sensitivity, while lower levels, such as those observed in menopause, could potentially lead to increased pain sensitivity. The exact impact of testosterone on pain perception in women is still an area of ongoing research.
Cortisol and Stress-Related Pain
Cortisol, a hormone produced by the adrenal glands in response to stress, can influence pain perception by modulating the body’s stress response. Chronic stress and elevated cortisol levels can heighten pain sensitivity and contribute to the development or exacerbation of chronic pain conditions. Conversely, balanced cortisol levels are essential for maintaining proper pain modulation and managing stress-related pain.
These hormonal influences on pain perception underscore the intricate relationship between hormonal fluctuations and pain sensitivity, highlighting the need for personalized approaches to pain management that consider individual hormonal profiles.
Chronic Pain Conditions Affected by Hormonal Changes
Several chronic pain conditions in women are notably influenced by hormonal changes, with fluctuations in hormones often exacerbating symptoms or altering pain perception. Here’s how hormonal changes impact specific chronic pain conditions:
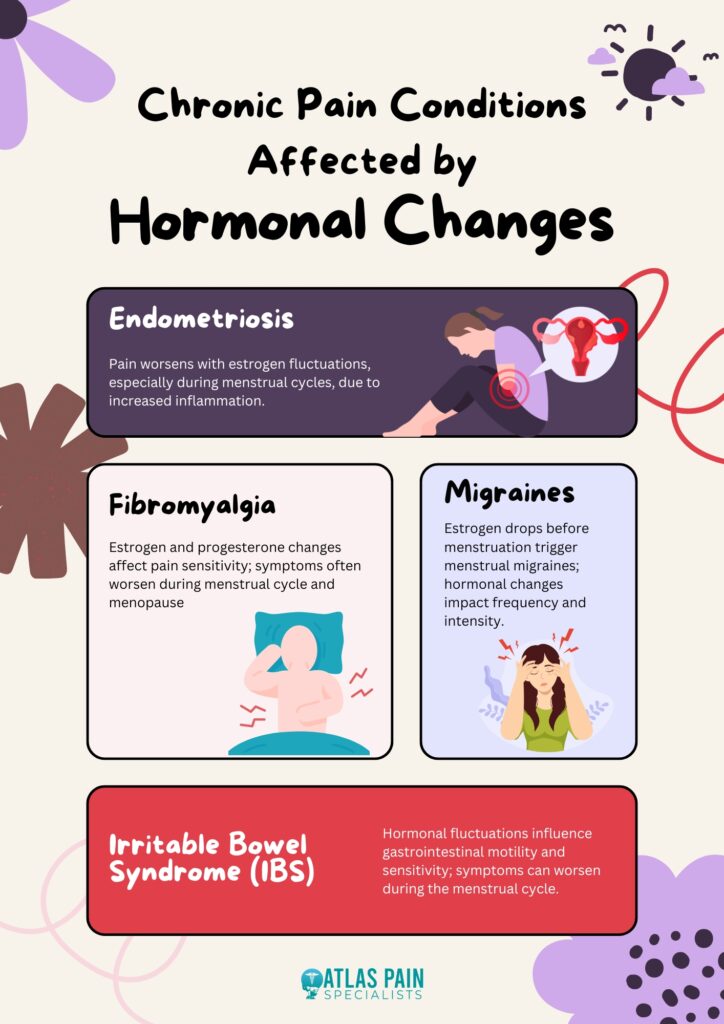
Endometriosis
Endometriosis is a condition characterized by the growth of tissue similar to the uterine lining outside the uterus, leading to significant pain and discomfort. Hormonal fluctuations, particularly variations in estrogen levels, can significantly impact the severity of endometriosis symptoms. Women often experience worsening pain during their menstrual cycle when estrogen levels are high, which can exacerbate the inflammatory processes associated with the condition.
Fibromyalgia
Fibromyalgia is a chronic condition marked by widespread musculoskeletal pain, fatigue, and tenderness. Hormonal changes, including those related to the menstrual cycle and menopause, can influence the severity of fibromyalgia symptoms. Estrogen and progesterone fluctuations are thought to affect pain sensitivity, with some women reporting increased pain during specific phases of their menstrual cycle or around menopause.
Migraines
Migraines are severe, recurring headaches that can be significantly influenced by hormonal changes. Many women experience migraines in relation to their menstrual cycle, a phenomenon known as menstrual migraines. The drop in estrogen levels just before menstruation is often linked to migraine attacks, making hormonal fluctuations a key factor in the frequency and intensity of migraines.
Irritable Bowel Syndrome (IBS)
IBS is a gastrointestinal disorder that can cause chronic abdominal pain, bloating, and changes in bowel habits. Hormonal changes can affect IBS symptoms, with many women experiencing exacerbations of their symptoms during their menstrual cycle. Fluctuations in estrogen and progesterone can influence gastrointestinal motility and sensitivity, contributing to the variability in IBS symptoms.
These chronic pain conditions illustrate the significant impact that hormonal changes can have on pain perception and management, highlighting the need for targeted approaches to treatment that consider hormonal influences.
Managing Chronic Pain with Hormonal Considerations
Effectively managing chronic pain in women requires addressing the impact of hormonal fluctuations on pain perception. Here are some strategies that consider hormonal influences:
Hormone Therapy
Hormone therapy, including estrogen or progesterone treatments, may be used to manage pain related to hormonal fluctuations. This approach needs to be tailored to individual needs and monitored by a healthcare provider to ensure effectiveness and minimize potential side effects.
Lifestyle Modifications
Adopting a healthy lifestyle can help manage chronic pain and its hormonal influences. Regular exercise, a balanced diet, and effective stress management can alleviate some of the symptoms and improve overall well-being. Maintaining a healthy weight and staying active can also enhance pain management.
Pain Management Techniques
Various techniques, such as cognitive-behavioral therapy (CBT), acupuncture, and mindfulness-based stress reduction (MBSR), can be beneficial. These approaches help manage chronic pain and its psychological impacts by developing coping strategies and reducing pain perception.
Medical Interventions
Medications, including analgesics, anti-inflammatory drugs, and hormone-specific treatments, can be used to address chronic pain. A healthcare provider can help determine the most appropriate medication regimen based on individual symptoms and hormonal factors.
By incorporating these strategies, individuals can better manage chronic pain while addressing the underlying hormonal influences.
Additional Tips to Manage Chronic Pain in Women
In addition to the primary strategies for managing chronic pain, there are several additional tips that can help women cope with pain exacerbated by hormonal changes:
Track Hormonal Cycles
Keeping a detailed record of menstrual cycles, hormonal fluctuations, and pain patterns can help identify triggers and patterns. This information can be valuable for adjusting treatments and predicting periods of increased pain.
Consider Hormonal Contraceptives
For some women, hormonal contraceptives can help regulate menstrual cycles and stabilize hormone levels, which may reduce pain associated with conditions like endometriosis or menstrual migraines. Consult a healthcare provider to determine if this approach is suitable.
Explore Dietary Adjustments
Certain dietary changes, such as increasing omega-3 fatty acids, reducing caffeine and sugar intake, and incorporating anti-inflammatory foods, can help manage pain. A nutritionist can provide personalized recommendations based on individual needs and hormonal influences.
Practice Relaxation Techniques
Stress can exacerbate pain and hormonal imbalances. Techniques such as deep breathing exercises, yoga, and progressive muscle relaxation can help reduce stress and improve pain management.
Use Heat and Cold Therapy
Applying heat or cold to affected areas can provide temporary relief from pain. Heat can relax muscles and alleviate stiffness, while cold packs can reduce inflammation and numb painful areas.
Stay Hydrated
Proper hydration is essential for overall health and can help prevent dehydration-related muscle cramps and discomfort. Drinking adequate water throughout the day can support pain management and overall well-being.
Seek Support Groups
Joining support groups or online communities for women with similar pain conditions can provide emotional support and practical advice. Sharing experiences and strategies can be empowering and help manage chronic pain.
Consult a Pain Specialist
Working with a pain specialist who understands the interaction between hormones and pain can lead to more tailored and effective treatment plans. They can offer advanced therapies and interventions specific to hormonal pain issues.
Incorporating these additional tips can enhance the management of chronic pain and address the specific challenges posed by hormonal changes.
Summary
Understanding the impact of hormones on chronic pain is essential for effective management in women. Hormones like estrogen, progesterone, and testosterone can influence pain sensitivity and worsen conditions such as endometriosis, fibromyalgia, migraines, and irritable bowel syndrome (IBS). Addressing these hormonal effects through hormone therapy, lifestyle changes, and targeted pain management strategies can enhance pain relief and overall well-being.
By integrating hormonal considerations into treatment plans, women can achieve better control over chronic pain and improve their quality of life.
About Dr. Sean Ormond