
The Impact of Chronic Pain on Sexual Health
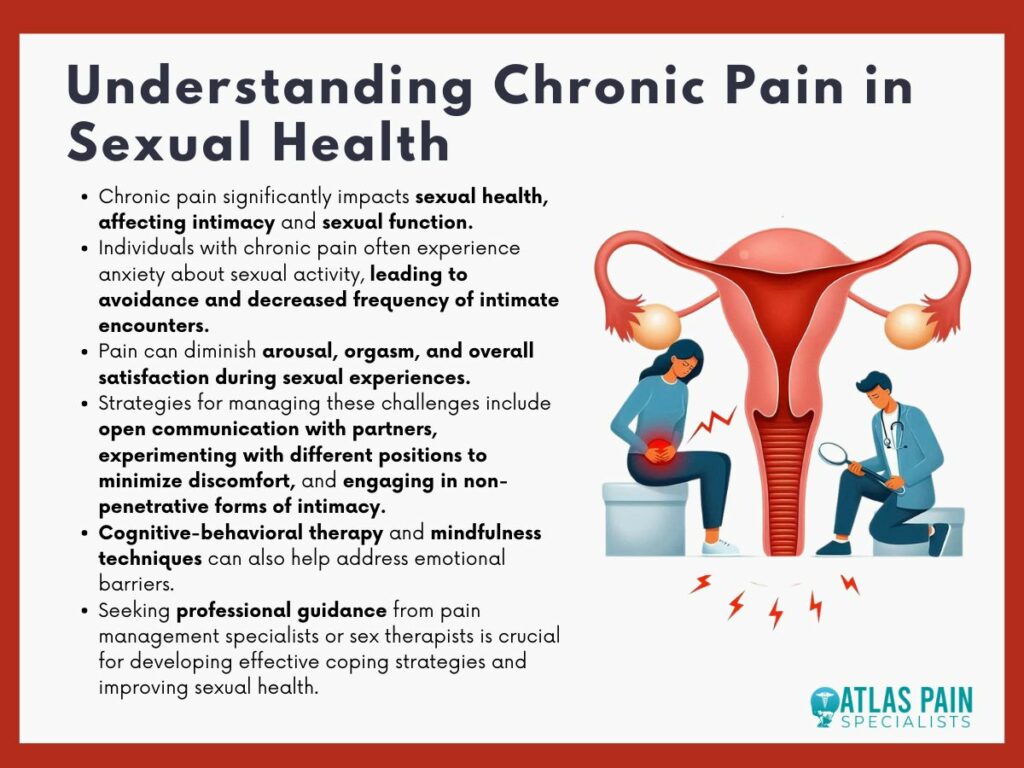
Chronic pain is a pervasive condition that affects millions worldwide, impacting every facet of life, including sexual health. The relationship between chronic pain and sexual dysfunction is complex and intertwined, with pain influencing sexual desire, performance, and satisfaction.
This article delves into the prevalence of sexual dysfunction among chronic pain sufferers, examining the statistical realities, gender-specific challenges, and illustrative case studies. It also highlights the broad spectrum of treatment strategies, from medical interventions to psychological therapies, emphasizing the need for a holistic approach to manage these interlinked aspects of health effectively.
Understanding Chronic Pain
Chronic pain, defined as pain persisting for longer than three months, impacts not just physical well-being but also influences various dimensions of personal health, including sexual health. As a complex and multifaceted condition, chronic pain requires a comprehensive understanding to effectively address its widespread effects.
Types of Chronic Pain
Chronic pain can manifest in various forms, each affecting the body in unique ways:
- Pelvic Pain: Often experienced in the lower abdomen, it can significantly affect sexual function and comfort.
- Fibromyalgia: Characterized by widespread muscle pain and tenderness, which can make physical contact uncomfortable.
- Migraines: Beyond intense headaches, migraines can make one sensitive to light and sound, complicating intimate settings.
Chronic pain arises from various sources, such as injuries, surgeries, and diseases. Conditions like arthritis, multiple sclerosis, and diabetes are common culprits, each leading to persistent pain that affects daily activities and personal relationships.
The psychological impact of chronic pain is profound. Constant pain can lead to emotional distress, anxiety, and depression, all of which are further complicated by the challenges of maintaining personal and intimate relationships.
Effects of Chronic Pain on Sexual Health
Chronic pain not only disrupts daily life but also deeply affects one's sexual health, altering physical capabilities and emotional states.
Physical Impacts
- Pain During Sexual Activity (Dyspareunia): For many, pain directly interferes with sexual activity, making it difficult or impossible to engage in and enjoy sexual encounters.
- Decreased Libido and Arousal Difficulties: Chronic pain can diminish sexual desire and arousal, as ongoing discomfort can make sexual engagement less appealing or more stressful.
- Impact on Physical Intimacy and Sexual Function: Chronic conditions can lead to fatigue, muscle tension, and hormonal imbalances, all of which impair sexual function and intimacy.
Psychological Impacts
- Emotional Distress and Sexual Dysfunction: The stress and frustration of chronic pain can lead to emotional disturbances that compound difficulties in sexual function, often creating a cycle of pain and dissatisfaction.
- Depression and Anxiety as Contributing Factors: These common comorbidities of chronic pain can further decrease sexual desire and satisfaction, as mental health struggles can diminish one’s capacity for sexual enjoyment.
- Cognitive Barriers Affecting Sexual Response: Pain can monopolize attention, making it hard to focus on sexual experiences and responses, which are crucial for satisfying sexual interactions.
Relationship Dynamics
- Changes in Intimacy and Communication: Chronic pain can alter the dynamics of a relationship, often leading to decreased intimacy as the partner without pain may feel neglected or helpless, and the suffering partner may feel burdensome.
- Effects on Relationship Satisfaction and Frequency of Sexual Activity: Frequent pain can reduce the frequency of sexual encounters between partners, which can strain relationships and decrease overall satisfaction within the partnership.
Prevalence of Sexual Dysfunction in Chronic Pain Patients
Sexual dysfunction is a common but often under-discussed issue among individuals with chronic pain. The prevalence of sexual dysfunction in this population is significantly higher than in the general population, owing to the complex interplay of physical, psychological, and pharmacological factors associated with chronic pain conditions.
Sexual dysfunction encompasses a range of issues, including decreased libido, difficulty in achieving or maintaining an erection, reduced sexual satisfaction, and pain during intercourse. In chronic pain patients, these issues are often exacerbated by the persistent nature of pain, which can affect both physical capabilities and mental well-being.
Prevalence and Contributing Factors
Studies indicate that sexual dysfunction affects a substantial proportion of chronic pain patients. Research suggests that more than 50% of individuals with chronic pain report some form of sexual dysfunction. This prevalence is higher compared to the general population, where sexual dysfunction rates range between 20-30%. The higher prevalence among chronic pain patients can be attributed to several factors:
- Physical Limitations: Chronic pain can lead to physical limitations that directly impact sexual activity. Pain during movement, reduced flexibility, and overall fatigue can make sexual activity difficult or unappealing. Conditions like arthritis, fibromyalgia, and lower back pain are particularly associated with these physical challenges.
- Psychological Impact: The psychological burden of chronic pain cannot be overstated. Depression, anxiety, and reduced quality of life are common in chronic pain patients, all of which can negatively affect sexual desire and performance. The stress and emotional strain associated with managing chronic pain can lead to a decreased interest in sexual activity and difficulties in sexual function.
- Medication Side Effects: Many chronic pain patients rely on medications to manage their pain, including opioids, antidepressants, and anticonvulsants. While these medications can provide relief from pain, they are also associated with side effects that can impair sexual function. For instance, opioids are known to reduce testosterone levels in both men and women, leading to decreased libido and erectile dysfunction in men. Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), are also commonly linked to sexual side effects, including anorgasmia and reduced arousal.
- Chronic Pain Conditions: Certain chronic pain conditions are more closely associated with sexual dysfunction. For example, individuals with chronic pelvic pain, endometriosis, or interstitial cystitis often experience pain during intercourse (dyspareunia), which can lead to avoidance of sexual activity and associated emotional distress.
- Relationship Dynamics: Chronic pain can strain relationships, particularly when it comes to intimacy. Partners of chronic pain patients may also experience frustration, emotional withdrawal, or guilt, further complicating sexual relationships. The fear of causing pain or discomfort during sexual activity can lead to reduced frequency of sexual encounters and increased sexual dissatisfaction.
Addressing Sexual Dysfunction in Chronic Pain Patients
Addressing sexual dysfunction in chronic pain patients requires a multidisciplinary approach that considers the physical, psychological, and relational aspects of the issue.
- Open Communication: Encouraging open communication between patients, their partners, and healthcare providers is crucial. Many patients may feel embarrassed or reluctant to discuss sexual issues, but addressing these concerns can lead to better management strategies and improved quality of life.
- Pain Management: Effective pain management is essential in reducing the impact of chronic pain on sexual function. Non-pharmacological approaches, such as physical therapy, acupuncture, and cognitive-behavioral therapy, can complement traditional pain management and potentially reduce the need for medications that have sexual side effects.
- Counseling and Therapy: Psychosexual counseling or therapy can be beneficial for both patients and their partners. This type of therapy can help address the emotional and psychological aspects of sexual dysfunction, improve communication between partners, and develop strategies to enhance intimacy despite physical limitations.
- Medication Review: Healthcare providers should regularly review the medications that chronic pain patients are taking and consider alternatives with fewer sexual side effects. Adjusting dosages or switching to different classes of medications may alleviate some of the sexual dysfunction while still effectively managing pain.
Treatment and Management Strategies
Effective treatment and management of sexual dysfunction in chronic pain patients require a multidisciplinary approach, combining medical interventions, psychological therapies, and strong communication strategies.
Medical Interventions
- Pain Management Techniques: Medications like anti-inflammatories, antidepressants, and opioids can reduce pain but may have side effects affecting sexual function. Nerve blocks and other procedural interventions can also provide relief, potentially restoring some aspects of sexual health.
- Role of Gynecologists and Pain Specialists: These professionals play crucial roles in diagnosing and treating underlying conditions contributing to both chronic pain and sexual dysfunction. Their insight can be vital in developing a tailored treatment plan that addresses both pain management and sexual health.
Psychological and Behavioral Approaches
- Cognitive-Behavioral Therapy (CBT): This therapy helps patients manage the psychological impacts of chronic pain, such as anxiety and depression, which can improve sexual function. CBT can reframe painful experiences and enhance coping strategies, improving overall sexual satisfaction.
- Intimacy Coaching and Mindfulness Practices: These approaches teach couples how to maintain intimacy and manage the impacts of chronic pain on their relationship. Mindfulness can help focus on the present moment, reducing the stress and anxiety associated with sexual interactions.
Communication and Support
- Importance of Discussing Sexual Health with Healthcare Providers: Patients are often reluctant to bring up sexual health issues. Encouraging open discussions with healthcare providers can lead to better diagnosis and management of related conditions.
- Strategies for Improving Communication with Partners: Open communication about the limitations and challenges posed by chronic pain can prevent misunderstandings and foster empathy within relationships. Techniques such as scheduled intimacy sessions or adjusted sexual practices can accommodate physical limitations while maintaining closeness.
Conclusion
Understanding and addressing the impact of chronic pain on sexual health is crucial for enhancing the quality of life for those affected. The discussions presented illustrate not only the high prevalence of sexual dysfunction among individuals with chronic pain but also the importance of an integrated treatment approach.
Effective management requires collaboration between healthcare providers, psychological support, and open communication between partners. By fostering a comprehensive understanding and proactive management strategy, patients can mitigate the effects of chronic pain on sexual health, leading to improved relationships and overall well-being. This holistic approach is key to navigating the complex interplay between chronic pain and sexual dysfunction.
About Dr. Sean Ormond