
The Connection Between Stress and Pain
Stress and pain have an intricate relationship, significantly impacting human health and quality of life. While everyone experiences stress and pain at varying levels and for different reasons, the link between the two is often overlooked.
Chronic stress can lead to physical pain, and chronic pain can lead to increased stress - a vicious cycle affecting one's physical and mental well-being.
This article explores the connection between stress and pain, delving into the physiological and psychological processes that link these two experiences and strategies for managing their combined effects.
Table of Contents
Understanding Stress and Pain
Stress is the body's natural response to harmful situations, whether real or perceived. When you feel threatened, your body triggers a “fight or flight” response, releasing a surge of hormones such as adrenaline and cortisol, causing an increase in heart rate, blood pressure, and glucose levels. While acute stress is beneficial for survival, chronic stress can lead to various health issues, including pain.
Conversely, pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage. It's the body's way of signaling that something is wrong and needs attention. Pain can be categorized as acute, such as that experienced after an injury, or chronic, where pain persists beyond the normal healing period, often with no discernible cause.
The Interplay between Stress and Pain
The relationship between stress and pain is a complex, often self-perpetuating cycle. Stress, triggered by threats or challenges, activates the 'fight or flight' response, releasing hormones like adrenaline and cortisol. Although this response is useful in acute situations, chronic stress can worsen the pain.
Pain, particularly chronic, can conversely activate the stress response, amplifying the pain perception and creating a persistent cycle. Factors such as emotional state can exacerbate this cycle, with negative emotions heightening pain perception and chronic stress reducing the body's pain threshold.
Stress and pain share neural pathways in the amygdala, hypothalamus, and prefrontal cortex, with stress potentially intensifying pain signals through these pathways. Also, stress hormones like cortisol can alter pain perception.
Management of this interplay necessitates a comprehensive approach, including cognitive-behavioral therapy, mindfulness, stress management, pain management strategies, and potentially medications. Understanding the intricate relationship between stress and pain can assist in developing strategies to mitigate both conditions, enhancing the quality of life for those dealing with chronic stress and pain.
How Chronic Pain Leads to Stress
Chronic pain, defined as pain that lasts for weeks, months, or even years, can significantly impact a person's life, often leading to a state of chronic stress. This connection can be understood through several key pathways.
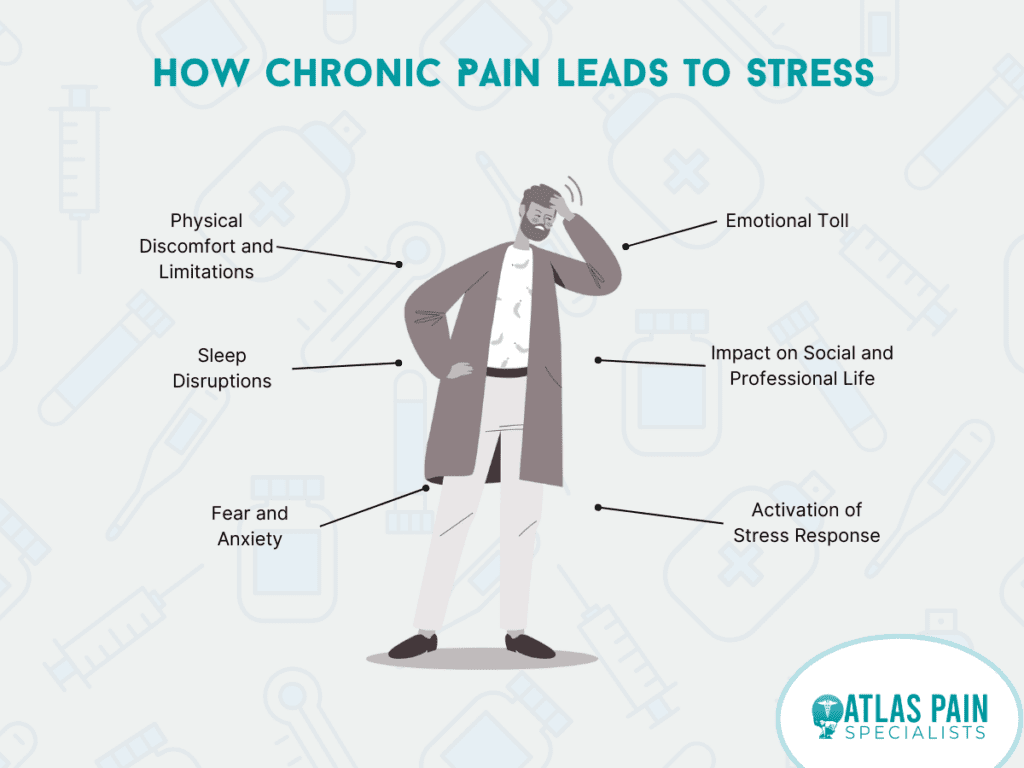
- Physical Discomfort and Limitations: The ongoing physical discomfort associated with chronic pain often inhibits regular activities, such as work, exercise, and social engagement. This limitation can lead to a constant state of stress as individuals struggle to navigate daily life within their physical constraints.
- Sleep Disruptions: Chronic pain frequently disrupts sleep patterns, preventing individuals from getting the rest they need. This can lead to increased fatigue, difficulty concentrating, and mood changes, all of which can contribute to heightened stress levels.
- Emotional Toll: The persistent nature of chronic pain can induce feelings of frustration, sadness, anxiety, and depression. The emotional strain of dealing with chronic pain can significantly increase stress.
- Fear and Anxiety: People with chronic pain may live in fear of the pain worsening or becoming incapacitated by it. This fear and anxiety can create a state of ongoing stress.
- Impact on Social and Professional Life: Chronic pain can affect a person's ability to maintain social relationships and professional responsibilities. The struggle to keep up with these aspects of life can lead to stress.
- Activation of Stress Response: Chronic pain triggers the body's stress response, causing the release of stress hormones such as cortisol. Prolonged exposure to these hormones can result in a state of chronic stress.
Effective chronic pain and stress management often involves a multifaceted approach, including medication, physical therapy, psychological support, and stress management techniques. Recognizing the close relationship between chronic pain and stress can help guide treatment and improve the quality of life for individuals dealing with these conditions.
Strategies for Managing Stress and Pain
Managing stress and pain requires a holistic approach that includes physical, psychological, medical, and lifestyle strategies. Here are some strategies:
Physical Interventions
Regular exercise is one of the most effective ways to manage stress and alleviate chronic pain. It improves blood flow, promotes the release of endorphins (the body's natural painkillers), and can improve sleep quality.
Activities like walking, swimming, yoga, and tai chi can be particularly beneficial. Always consult with a healthcare professional before starting a new exercise regime, especially if you have chronic pain.
Psychological Interventions
The link between the mind and body is significant when dealing with stress and pain. Cognitive-behavioral therapy (CBT) is a type of psychological treatment that can help manage the perception of pain and stress.
It teaches individuals to identify, understand, and change negative thought patterns that can exacerbate stress and pain. Mindfulness and meditation can also help by promoting relaxation and aiding in stress management.

Medical Interventions
Medical interventions may be necessary depending on the nature and severity of your pain. Over-the-counter and prescription medications can help manage pain and stress. In some cases, more invasive procedures like surgery may be required. Always consult with your healthcare provider for personalized advice and treatment plans.
Lifestyle Modifications
A healthy lifestyle can go a long way in managing stress and chronic pain. Balanced nutrition supports overall health, and specific diets may help reduce inflammation, a key contributor to pain. Adequate sleep is crucial for recovery and stress management.
Avoiding nicotine and alcohol, known to exacerbate stress and pain, is also recommended. Integrating relaxation techniques into your daily routine, such as deep breathing, progressive muscle relaxation, or guided imagery, can also be helpful.
Social Support
Never underestimate the power of social support in managing stress and pain. Reach out to loved ones, join a support group, or consider speaking to a counselor or therapist. Feeling understood and supported can significantly reduce feelings of stress and help in the management of pain.
Remembering that what works for one person may not work for another is essential. Therefore, always consult a healthcare professional to develop a personalized plan that suits your needs.

Conclusion
The connection between stress and pain is a complex, bidirectional relationship with significant physical and mental health implications. Understanding this connection is vital for developing effective interventions to break the cycle and improve quality of life.
It's crucial to remember that each individual's experience with stress and pain is unique, and what works for one person may not work for another. Therefore, personalized, holistic approaches are often the most effective in managing stress and pain.
About Dr. Sean Ormond