
The Impact of Weather on Pain Conditions
When you have a chronic pain condition, the weather can have a significant effect on how your body feels. Fall and winter can often indicate greater pain. A shift in temperature can tighten tendons, ligaments, and muscles, causing pain all across the body.
Despite the lack of evidence linking joint pain to the weather, many people believe they can anticipate the weather based on these aches. This article will examine the impact of weather on pain conditions and provide strategies for managing these effects on overall health.
How Weather Affects the Body
The onset of cold weather triggers a cascade of physiological responses within the body, particularly in the musculoskeletal system. When exposed to colder temperatures, muscles tend to contract, leading to increased stiffness and reduced flexibility.
For individuals already contending with chronic pain conditions, this heightened muscular tension can worsen pain. Additionally, cold weather can constrict blood vessels, reducing blood flow to affected areas and intensifying the perception of pain.
- The Role of Barometric Pressure, Humidity, and Temperature
Beyond temperature, other meteorological factors wield considerable influence over pain perception. Barometric pressure, the weight of the atmosphere pressing down on the earth, has been linked to changes in joint pain.
As barometric pressure drops, which often precedes changes in weather, some individuals with joint conditions may experience increased pain. Moreover, humidity levels and temperature variations can impact the viscosity of synovial fluid in joints, affecting their lubrication and contributing to discomfort.
- Neurological Responses to Atmospheric Changes
Changes in weather conditions can influence the activity of nerve endings, altering pain signals and thresholds. In colder weather, nerve conductivity may decrease, potentially leading to heightened sensitivity and amplified pain responses.
This neurological dimension adds another layer of complexity to the intricate dance between meteorology and the human body, emphasizing the need for a holistic understanding of the mechanisms at play.
Conditions Affected by Weather
Weather patterns have an impact on many health issues, but they have an especially obvious effect on chronic pain conditions. Understanding the complex relationships between weather and health is essential for managing and treating these disorders for both individuals and healthcare professionals.
| Condition | Weather Sensitivity |
| Arthritis | Barometric pressure changes, cold and damp weather |
| Fibromyalgia | Cold and damp weather |
| Migraines | Barometric pressure changes, temperature fluctuations |
| Raynaud's Disease | Cold weather, emotional stress |
1. Arthritis
Among the conditions most profoundly impacted by weather changes is arthritis, a term encompassing a spectrum of inflammatory joint disorders. For those with osteoarthritis or rheumatoid arthritis, shifts in atmospheric pressure can herald shifts in pain levels.
Decreases in barometric pressure, often associated with impending storms or changes in weather patterns, may lead to expansion of joint tissues and increased fluid retention, intensifying the ache and stiffness characteristic of arthritis.
2. Fibromyalgia
Another long-term musculoskeletal disorder that is weather-sensitive is fibromyalgia, which is characterized by fatigue, localized discomfort, and generalized pain. Cold and damp weather, in particular, can amplify the symptoms of fibromyalgia, with the cold worsening muscle stiffness and the dampness intensifying the perception of pain.
3. Migraines
Beyond musculoskeletal conditions, migraines are another example of a pain disorder intricately tied to atmospheric changes. Changes in barometric pressure, often preceding storms, have been identified as triggers for migraines in some individuals.
Additionally, fluctuations in temperature and exposure to certain weather patterns can contribute to the onset of migraine attacks.
4. Raynaud's Disease
Raynaud's disease, a disorder affecting blood flow to certain areas of the body, particularly fingers and toes, showcases the impact of temperature on pain conditions. Exposure to cold or emotional stress can trigger vasospasms, leading to reduced blood flow and causing pain, numbness, and color changes in affected areas.
Managing Weather-Related Pain
An all-encompassing strategy that acknowledges the dynamic interaction between weather conditions and personal health is necessary to effectively manage weather-related pain. Achieving the best pain treatment results requires understanding how each person's sensitivity to weather changes is different and tailoring interventions accordingly.

1. Embracing Physical Activity and Flexibility
One of the cornerstones in weather-related pain management lies in the embrace of physical activity and flexibility. Regular exercise, tailored to accommodate weather conditions, promotes joint mobility, muscle strength, and overall physical well-being.
Engaging in activities such as gentle stretching, yoga, or low-impact exercises can counteract the stiffness exacerbated by cold weather, fostering a more resilient musculoskeletal system.
2. Hydration as a Weather-Responsive Ally
In the battle against weather-induced pain, hydration emerges as a powerful ally. Cold and dry weather can contribute to dehydration, exacerbating the perception of pain. Maintaining optimal hydration levels ensures the body's physiological processes function smoothly, reducing the risk of increased discomfort.
Individuals navigating weather-related pain should prioritize regular water intake, considering the impact of both temperature and humidity on their hydration needs.
3. Mindful Pain Management Techniques
Mindfulness and stress-reduction techniques play a pivotal role in managing weather-related pain. The psychological and emotional impact of weather changes can contribute to heightened pain perception.
Practices such as meditation, deep breathing exercises, and mindfulness-based stress reduction (MBSR) provide individuals with tools to navigate the mental aspects of pain.
4. Adaptive Strategies for Cold and Damp Weather
Tailoring strategies to weather conditions is essential for effective pain management. Wearing layers to maintain body heat, applying heated compresses or heating pads to relieve sore joints, and making sure interior spaces are sufficiently heated are all beneficial practices in cold and wet weather.
Additionally, maintaining a well-balanced diet rich in anti-inflammatory foods can contribute to overall resilience.
Debunking Myths and Clarifying Facts
It is important to dispel myths and provide clarity on the facts relevant to the correlation between pain and weather in order to promote a more precise understanding of this complex phenomenon. With this insight, patients can adopt practical tactics, collaborate with healthcare experts, and improve their general well-being.
| Statement | Myth or Fact |
| Weather affects everyone equally | Myth |
| Only cold weather influences pain | Myth |
| There is a scientific basis for weather-pain links | Fact |
| Management strategies are effective | Fact |
| Weather-related pain is purely psychosomatic | Myth |
1. Myth: Weather Affects Everyone Equally
A prevalent misconception regarding weather-related pain is the belief that its impact is uniform across all individuals. In reality, the relationship between weather and pain is highly individualized.
While some may experience heightened discomfort during specific weather conditions, others may find relief. Factors such as genetics, overall health, and the specific nature of the pain condition contribute to this variability.
2. Myth: Only Cold Weather Influences Pain
Another common myth surrounding weather-related pain is the notion that cold weather is the sole culprit. While cold temperatures can indeed impact pain perception, it's essential to recognize that other meteorological factors play significant roles.
Barometric pressure, humidity levels, and temperature fluctuations all contribute to the intricate dance between weather and pain as discussed earlier.
3. Fact: Scientific Basis for Weather-Pain Connections
Contrary to some skeptics, there is a scientific basis for the connection between weather and pain. Studies have investigated the physiological systems involved, examining the ways in which variations in temperature, humidity, and air pressure can impact an individual's feeling of pain.
While the exact mechanisms are complex and vary among individuals and conditions, the scientific community acknowledges the existence of a genuine relationship.
4. Fact: Management Strategies Are Effective
A common misconception is the belief that weather-related pain is insurmountable and uncontrollable. In reality, the development and implementation of effective management strategies can significantly alleviate the impact of weather on pain conditions.
From tailored physical exercises to mindfulness techniques and adaptive lifestyle adjustments, individuals can proactively manage and mitigate the effects of atmospheric changes.
5. Myth: Weather-Related Pain is Psychosomatic
Some skeptics argue that weather-related pain is purely psychosomatic, attributing the perceived discomfort to psychological factors rather than physiological changes.
While the mind-body connection undoubtedly plays a role in pain perception, the physiological responses observed in individuals with conditions like arthritis or fibromyalgia provide concrete evidence of the weather's impact.
The Psychosomatic Aspect Of Weather Related Pain
The complex interaction between psychological variables and bodily experiences is what makes weather-related pain psychosomatic.
Although some skeptics would write off weather-related pain as solely psychological, it's important to understand that the mind and body are closely intertwined and that psychological variables can affect how someone perceives and experiences pain.
Here are key points to consider when discussing the psychosomatic aspect of weather-related pain:
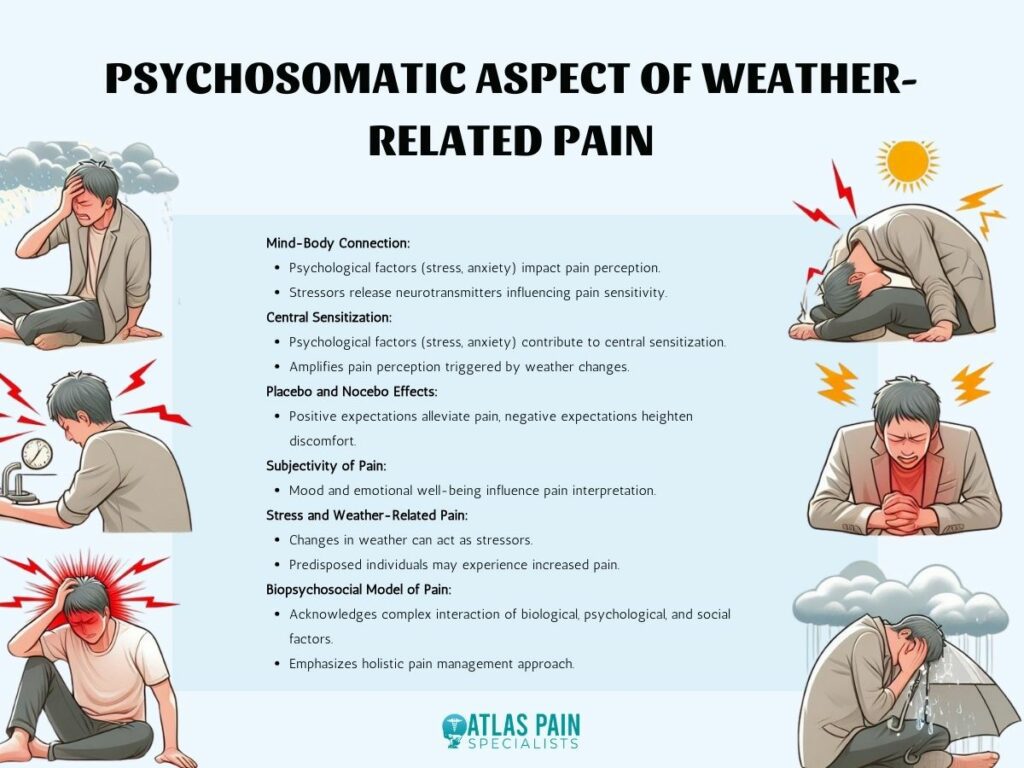
1. Mind-Body Connection
The mind and body are interconnected, and psychological factors such as stress, anxiety, and mood can impact the perception of pain.
Psychological stressors may contribute to the release of certain neurotransmitters and hormones that modulate pain sensitivity, influencing how individuals experience discomfort.
2. Central Sensitization
Central sensitization is a phenomenon where the central nervous system becomes more responsive to stimuli, including pain signals.
Psychological factors, such as chronic stress or anxiety, can contribute to central sensitization, potentially amplifying the perception of pain triggered by weather changes.
3. Placebo and Nocebo Effects
The placebo effect, where a person experiences relief due to their belief in a treatment's efficacy, and the nocebo effect, where negative expectations lead to increased symptoms, are relevant in the context of psychosomatic influences.
Positive expectations about the impact of weather or certain weather conditions might alleviate pain, while negative expectations could heighten discomfort.
4. Subjectivity of Pain
Pain is a subjective experience influenced by individual perceptions and psychological states.
Factors such as mood, outlook, and emotional well-being can shape how individuals interpret and report their pain, including pain associated with changes in weather.
5. Stress and Weather-Related Pain
Stress is a known contributor to the exacerbation of various health conditions, including those associated with pain.
Changes in weather can be stressors, and individuals who are predisposed to stress-induced responses may experience an increase in pain during weather fluctuations.
6. Biopsychosocial Model of Pain
The biopsychosocial model of pain acknowledges the complex interaction between biological, psychological, and social factors in shaping the pain experience.
In the context of weather-related pain, this model underscores the need to consider both physical and psychological aspects when understanding and managing discomfort.
- It's important to stress that, despite the psychosomatic component of weather-related pain, the pain experience is nonetheless legitimate. Instead, it emphasizes how important it is to take a holistic approach to pain management, taking into account both the psychological and physical aspects and acknowledging the interconnectedness of each person's overall health.
In order to gain a better grasp of these complex relationships between pain, psychology, and weather, studies on these links are still ongoing.
Debunking Pain Management Myths
As with illnesses like fibromyalgia, migraines, and arthritis, the association between weather and chronic pain is a complicated and unique phenomenon. While joint stiffness and inflammation may cause some people to feel more uncomfortable in cold and humid weather, the effect varies greatly amongst patients.
It is important to debunk popular myths, such as the idea that moving to a different environment can magically cure all pain or that pain can be uniformly predicted by the weather.
Effective pain management strategies should integrate holistic techniques such as physical therapy and mindfulness, emphasize individualized approaches, and educate patients about the complex nature of chronic pain, instead of merely depending on weather forecasts.
Realistic expectations and empowering people to better manage their circumstances depend on an understanding that weather is only one component of a complex interplay of forces.
About Dr. Sean Ormond